Neurointervention.
2023 Mar;18(1):30-37. 10.5469/neuroint.2022.00479.
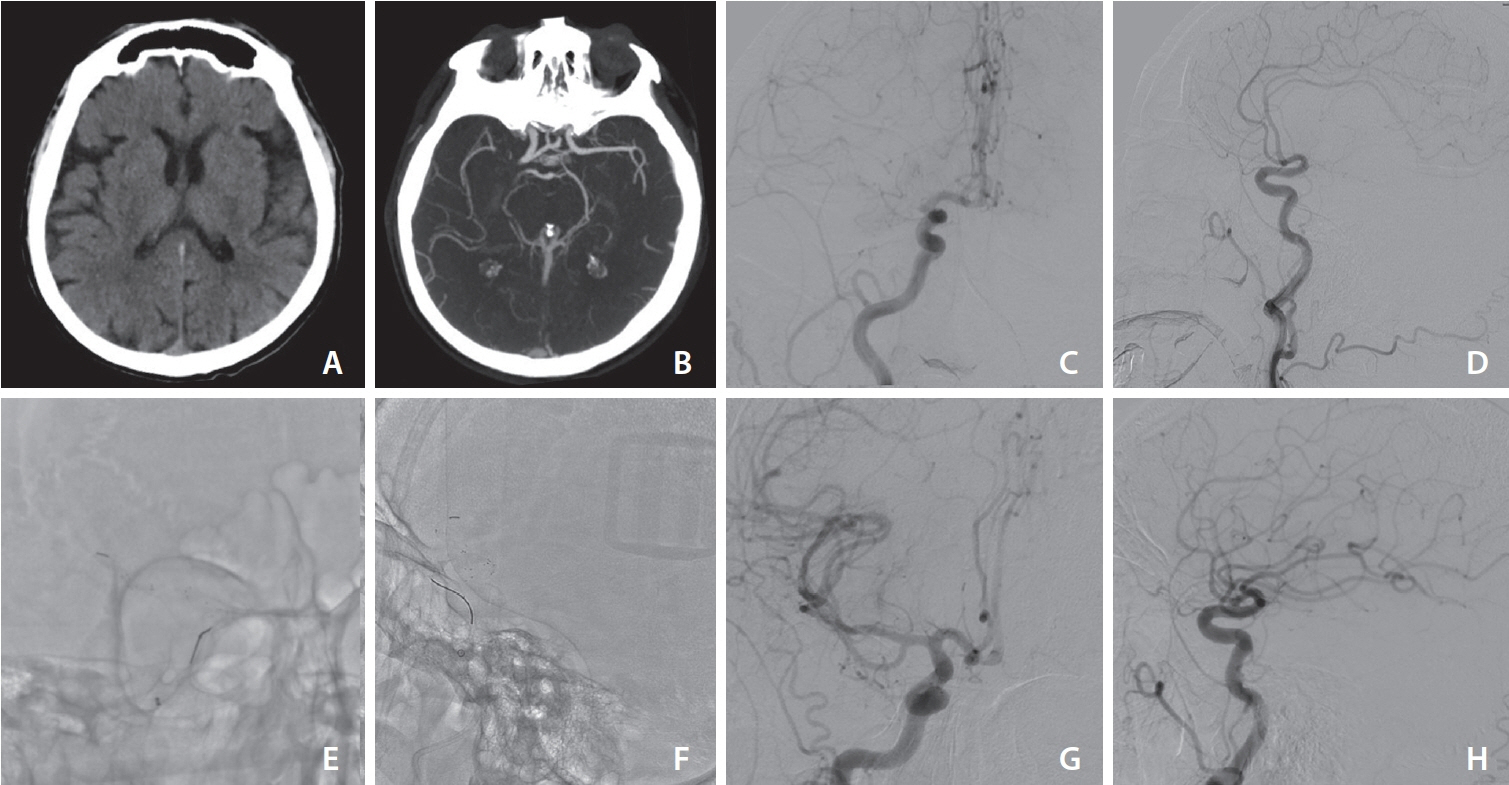
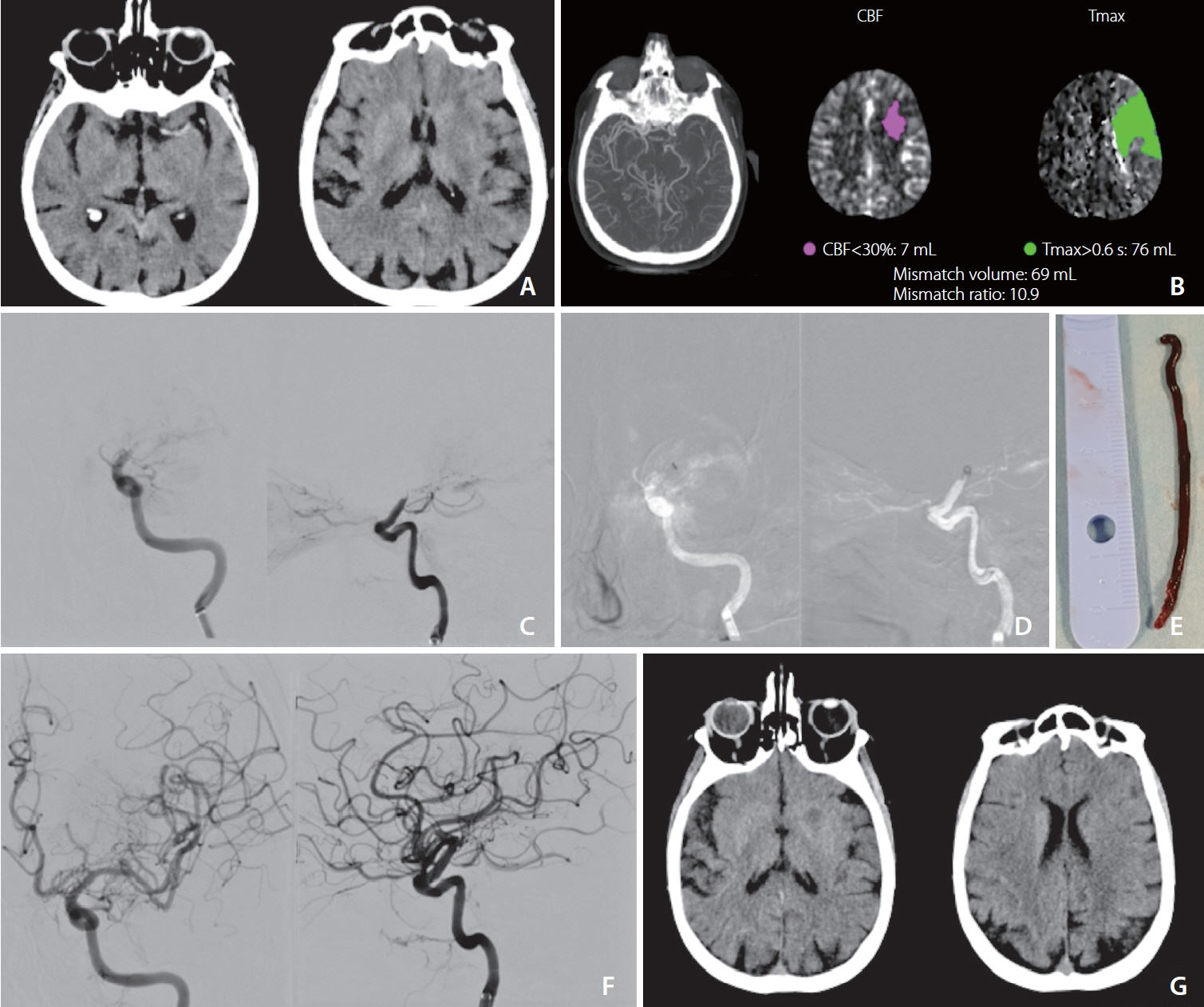
Initial Experience Using the New pHLO 0.072-inch Large-Bore Catheter for Direct Aspiration Thrombectomy in Acute Ischemic Stroke
- Affiliations
-
- 1Unit of Interventional Neuroradiology, Department of Advanced Diagnostic and Therapeutic Technologies, A.O.R.N. Antonio Cardarelli Hospital, Napoli, Italy
- 2Unit of Neuroradiology, AOU San Giovanni di Dio e Ruggi d’Aragona, University of Salerno, Salerno, Italy
- 3Unit of Neurology and Stroke, Department of Emergency and Acceptance, A.O.R.N. Antonio Cardarelli Hospital, Naples, Italy
- KMID: 2539944
- DOI: http://doi.org/10.5469/neuroint.2022.00479
Abstract
- Purpose
A direct aspiration, first pass technique (ADAPT) has been introduced as a rapid and safe thrombectomy strategy in patients with intracranial large vessel occlusion (LVO). The aim of the study is to determine the technical feasibility, safety, and functional outcome of ADAPT using the newly released large bore pHLO 0.072-inch aspiration catheter (AC; Phenox).
Materials and Methods
We performed a retrospective analysis of data collected prospectively (October 2019–November 2021) from 2 comprehensive stroke centers. Accessibility of the thrombus, vascular recanalization, time to recanalization, and procedure-related complications were evaluated. National Institutes of Health stroke scale scores at presentation and discharge and the modified Rankin scale (mRS) score at 90 days post-procedure were recorded.
Results
Twenty-five patients (14 female, 11 male) with occlusions of the anterior circulation were treated. In 84% of cases, ADAPT led to successful recanalization with a median procedure time of 28 minutes. In the remaining cases, successful recanalization required (to a total of 96%; modified thrombolysis in cerebral infarction score 2b/3) the use of stent retrievers. No AC-related complications were reported. Other complications included distal migration of the thrombus, requiring a stent-retriever, and symptomatic PH2 hemorrhage in 16% and 4%, respectively. After 3 months, 52% of the patients had mRS scores of 0–2 with an overall mortality rate of 20%.
Conclusion
Results from our retrospective case series revealed that thrombectomy of LVOs with pHLO AC is safe and effective in cases of large-vessel ischemic stroke. Rates of complete or near-complete recanalization after the first pass with this method might be used as a new benchmark in future trials.
Keyword
Figure
Reference
-
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, HERMES Collaborators, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418. Erratum in: Stroke 2019;50:e440-e441.
Article3. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2018; 10(Suppl 1):i4–i7.
Article4. Turk AS 3rd, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. 2019; 393:998–1008.
Article5. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, ASTER Trial Investigators, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA. 2017; 318:443–452.
Article6. Gory B, Armoiry X, Sivan-Hoffmann R, Piotin M, Mazighi M, Lapergue B, et al. A direct aspiration first pass technique for acute stroke therapy: a systematic review and meta-analysis. Eur J Neurol. 2018; 25:284–292.
Article7. Heit JJ, Wong JH, Mofaff AM, Telischak NA, Dodd RL, Marks MP, et al. Sofia intermediate catheter and the SNAKE technique: safety and efficacy of the Sofia catheter without guidewire or microcatheter construct. J Neurointerv Surg 2018;10:401-406 Erratum in: J Neurointerv Surg. 2021; 13:e12.
Article8. Raymond SB, Nasir-Moin M, Koch MJ, Rabinov JD, Leslie-Mazwi T, Patel AB. Initial experience with react 68 aspiration catheter. Interv Neuroradiol. 2020; 26:358–363.
Article9. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.10. Boisseau W, Escalard S, Fahed R, Lapergue B, Smajda S, Maier B, et al. Direct aspiration stroke thrombectomy: a comprehensive review. J Neurointerv Surg. 2020; 12:1099–1106.
Article11. Chivot C, Renier J, Deramond H, Bouzerar R, Yzet T. Direct aspiration for thrombectomy in ischemic stroke: impact of dwell time. Interv Neuroradiol. 2020; 26:211–215.
Article12. Kaschner MG, Rubbert C, Caspers J, Karsten J, Kraus B, Lee JI, et al. A retrospective single-center case series of direct aspiration thrombectomy as first-line approach in ischemic stroke and review of the literature. J Stroke Cerebrovasc Dis. 2019; 28:640–648.
Article13. Romano DG, Cioni S, Vinci SL, Pero G, Comelli C, Comai A, et al. Thromboaspiration technique as first approach for endovascular treatment of acute ischemic stroke: initial experience at nine Italian stroke centers. J Neurointerv Surg. 2017; 9:6–10.
Article14. Zhang Y, Zhang Y, Hu C, Zhao W, Zhang Z, Li W. A direct aspiration first-pass technique (ADAPT) versus stent retriever for acute ischemic stroke (AIS): a systematic review and meta-analysis. J Neurol. 2021; 268:4594–4606.
Article15. Bernava G, Rosi A, Boto J, Brina O, Kulcsar Z, Czarnetzki C, et al. Direct thromboaspiration efficacy for mechanical thrombectomy is related to the angle of interaction between the aspiration catheter and the clot. J Neurointerv Surg. 2020; 12:396–400.
Article16. Hu YC, Stiefel MF. Force and aspiration analysis of the ADAPT technique in acute ischemic stroke treatment. J Neurointerv Surg. 2016; 8:244–246.
Article17. Primiani CT, Vicente AC, Brannick MT, Turk AS, Mocco J, Levy EI, et al. Direct aspiration versus stent retriever thrombectomy for acute stroke: a systematic review and meta-analysis in 9127 patients. J Stroke Cerebrovasc Dis. 2019; 28:1329–1337.
Article18. Phan K, Dmytriw AA, Teng I, Moore JM, Griessenauer C, Ogilvy C, et al. A direct aspiration first pass technique vs standard endovascular therapy for acute stroke: a systematic review and meta-analysis. Neurosurgery. 2018; 83:19–28.
Article19. Anadani M, Alawieh A, Vargas J, Chatterjee AR, Turk A, Spiotta A. First attempt recanalization with ADAPT: rate, predictors, and outcome. J Neurointerv Surg. 2019; 11:641–645.
Article20. Nogueira RG, Ryan D, Mullins L, Thornton J, Fitzgerald S. Maximizing the catheter-to-vessel size optimizes distal flow control resulting in improved revascularization in vitro for aspiration thrombectomy. J Neurointerv Surg. 2022; 14:184–188.
Article21. Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, Distal Thrombectomy Summit Group, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020; 51:2872–2884. Erratum in: Stroke 2020;51:e296.22. Alawieh A, Chatterjee AR, Vargas J, Chaudry MI, Lena J, Turner R, et al. Lessons learned over more than 500 stroke thrombectomies using adapt with increasing aspiration catheter size. Neurosurgery. 2020; 86:61–70.
Article23. Chueh JY, Puri AS, Wakhloo AK, Gounis MJ. Risk of distal embolization with stent retriever thrombectomy and ADAPT. J Neurointerv Surg. 2016; 8:197–202.
Article24. Nabil M, Chater G, Correia P, Wegener S, Baltsavias G. Thrombectomy-related emboli: direct aspiration versus stent retriever thrombectomy for acute ischemic stroke: our experience and literature review. World Neurosurg. 2020; 135:e588–e597.
Article25. Li J, Ribo M. REACT aspiration catheters: clinical experience and technical considerations. Neurointervention. 2022; 17:70–77.
Article26. Settecase F, Kim WT, English JD. AXS Vecta 0.071-0.074 inch aspiration catheters for mechanical thrombectomy: case series and literature review. [published online ahead of print Nov 4, 2022] Neurointervention 2022.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Effectiveness of Anchoring with Balloon Guide Catheter and Stent Retriever in Difficult Mechanical Thrombectomy for Large Vessel Occlusion
- The Aspirations of Direct Aspiration for Thrombectomy in Ischemic Stroke: A Critical Analysis
- Initial Experience Using the 5MAX(TM) ACE Reperfusion Catheter in Intra-arterial Therapy for Acute Ischemic Stroke
- Pull-Through Buddy Wire Technique for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke: Technical Note