Clin Exp Otorhinolaryngol.
2023 Feb;16(1):67-74. 10.21053/ceo.2022.00976.
Tongue Reduction Surgery Improves Mandibular Prognathism in Beckwith-Wiedemann Syndrome Without Compromising Tongue Function
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Boramae Medical Center, Seoul, Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 5Interdisciplinary Program in Stem Cell Biology, Seoul National University, Seoul, Korea
- 6Cancer Research Institute, Seoul National University, Seoul, Korea
- KMID: 2539770
- DOI: http://doi.org/10.21053/ceo.2022.00976
Abstract
Objectives
. This study evaluated the surgical outcomes of patients with Beckwith-Wiedemann syndrome who underwent tongue-reduction surgery and analyzed whether the malocclusion and mandibular prognathism caused by macroglossia could be improved.
Methods
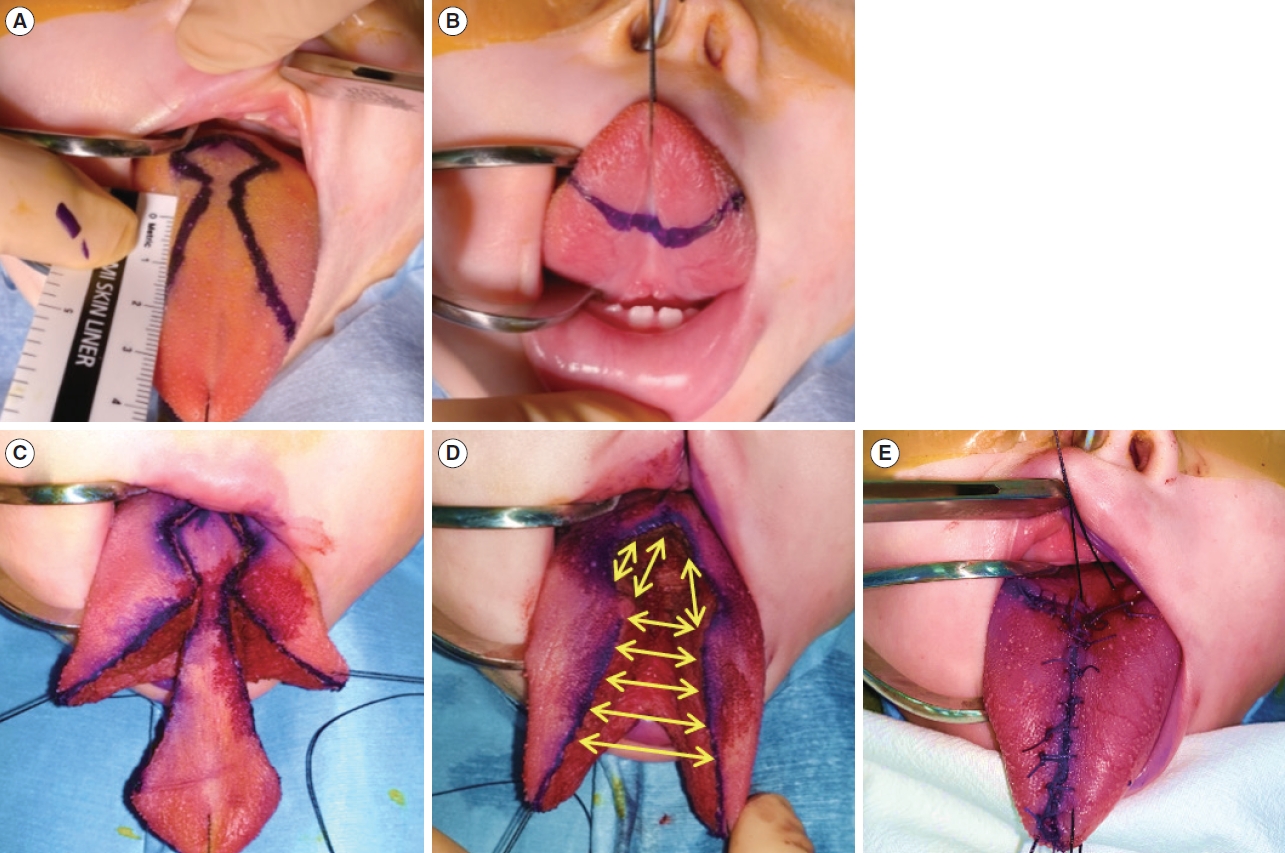
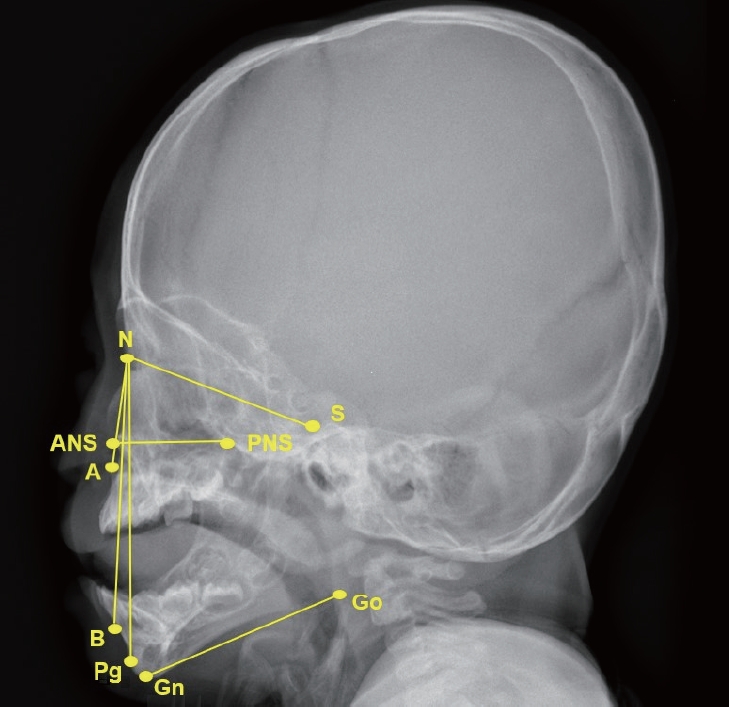
. A retrospective medical record review was performed for 11 patients with Beckwith-Wiedemann syndrome whose macroglossia was surgically treated. Demographic data, symptoms and signs, and intraoperative and postoperative surgical outcomes were evaluated. Surgery was performed by a single surgeon using the “keyhole” technique, involving midline elliptical excision and anterior wedge resection. Preoperative and postoperative plain skull lateral X-rays were evaluated to assess prognathism improvement.
Results
. The median age at the time of surgery was 35.09 months, and the ratio of males to females was 4:7. The median surgical time was 98±31.45 minutes, and the median duration of the postoperative intensive care unit stay was 3.81±2.4 days. There were no airway complications. Two patients (18.2%) had postoperative wound dehiscence; however, there was no nerve damage, recurrence, or other complications. Among the five patients who underwent postoperative speech evaluation, all showed normal speech development, except one patient who had brain dysfunction and developmental delay. Measurements of the A point-nasion-B point (ANB) angles and sella-nasion-B point (SNB) angles (point A is the most concave point of the anterior maxilla; point B is the most concave point on the mandibular symphysis) on plain X-rays showed a significant decrease in the postoperative SNB angle (P <0.001) and a significant increase in the ANB angle (P <0.011).
Conclusion
. Tongue-reduction surgery is an effective and safe technique for severe forms of macroglossia associated with Beckwith-Wiedemann syndrome. In addition, it improves mandibular prognathism in young Beckwith-Wiedemann syndrome patients with macroglossia.
Figure
Reference
-
1. Beckwith JB. Extreme cytomegaly of the adrenal fetal cortex, omphalocele, hyperplasia of the kidneys and pancreas, and Leydig-cell hyperplasia: another syndrome? In : Proceedings of the annual meeting of the Western Society for Pediatric Research; 1963 Nov; Los Angeles, CA.2. Wiedemann HR. Familial malformation complex with umbilical hernia and macroglossia: a “new syndrome”. J Genet Hum. 1964; Sep. 13:223–32.3. Higurashi M, Iijima K, Sugimoto Y, Ishikawa N, Hoshina H, Watanabe N, et al. The birth prevalence of malformation syndromes in Tokyo infants: a survey of 14,430 newborn infants. Am J Med Genet. 1980; 6(3):189–94.
Article4. Elliott M, Maher ER. Beckwith-Wiedemann syndrome. J Med Genet. 1994; Jul. 31(7):560–4.
Article5. Lodeiro JG, Byers JW 3rd, Chuipek S, Feinstein SJ. Prenatal diagnosis and perinatal management of the Beckwith-Wiedeman syndrome: a case and review. Am J Perinatol. 1989; Oct. 6(4):446–9.
Article6. Weksberg R, Squire JA. Molecular biology of Beckwith-Wiedemann syndrome. Med Pediatr Oncol. 1996; Nov. 27(5):462–9.
Article7. Limbrock GJ, Fischer-Brandies H, Avalle C. Castillo-Morales’ orofacial therapy: treatment of 67 children with Down syndrome. Dev Med Child Neurol. 1991; Apr. 33(4):296–303.
Article8. Ainuz BY, Geisler EL, Hallac RR, Perez JK, Seaward JR, Kane AA. Anterior “W” tongue reduction for macroglossia in Beckwith-Wiedemann syndrome. Cleft Palate Craniofac J. 2022; Sep. 59(9):1145–54.
Article9. Steiner CC. Cephalometrics in clinical practice. Angle Orthod. 1959; Jan. 29(1):8–29.10. Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996; Aug. 110(2):170–7.
Article11. Balaji SM. Reduction glossectomy for large tongues. Ann Maxillofac Surg. 2013; Jul. 3(2):167–72.
Article12. Rimell FL, Shapiro AM, Shoemaker DL, Kenna MA. Head and neck manifestations of Beckwith-Wiedemann syndrome. Otolaryngol Head Neck Surg. 1995; Sep. 113(3):262–5.
Article13. Shipster C, Oliver B, Morgan A. Speech and oral motor skills in children with Beckwith Wiedemann Syndrome: pre-and post-tongue reduction surgery. Adv Speech Lang Pathol. 2006; Jan. 8(1):45–55.
Article14. Alonso-Rodriguez E, Gomez E, Martin M, Munoz JM, HernandezGodoy J, Burgueno M. Beckwith-Wiedemann syndrome: open bite evolution after tongue reduction. Med Oral Patol Oral Cir Bucal. 2018; Mar. 23(2):e225–9.
Article15. Kole H. Results, experience, and problems in the operative treatment of anomalies with reverse overbite (mandibular protrusion). Oral Surg Oral Med Oral Pathol. 1965; Apr. 19(4):427–50.
Article16. Meazzini MC, Besana M, Tortora C, Cohen N, Rezzonico A, Ferrari M, et al. Long-term longitudinal evalutation of mandibular growth in patients with Beckwith-Wiedemann syndrome treated and not treated with glossectomy. J Craniomaxillofac Surg. 2020; Dec. 48(12):1126–31.
Article17. Massengill R, Pickrell K. Surgical correction of macroglossia. Pediatrics. 1978; Mar. 61(3):485–8.
Article18. Kaufman Y, Cole P, McKnight A, Hatef DA, Hollier L, Edmonds J. A modified keyhole technique for correction of macroglossia. Plast Reconstr Surg. 2008; Dec. 122(6):1867–9.
Article19. Gardon MA, Andre CV, Ernenwein D, Teissier N, Bennaceur S. New surgical method of tongue reduction for macroglossia: technical note. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019; Jan. 127(1):e1–7.
Article20. Egyedi P. Reduction of tongue size in the surgical correction of jaw deformity. Br J Oral Surg. 1965; Jul. 3(1):13–21.
Article21. Davalbhakta A, Lamberty BG. Technique for uniform reduction of macroglossia. Br J Plast Surg. 2000; Jun. 53(4):294–7.
Article22. Heggie AA, Vujcich NJ, Portnof JE, Morgan AT. Tongue reduction for macroglossia in Beckwith Wiedemann syndrome: review and application of new technique. Int J Oral Maxillofac Surg. 2013; Feb. 42(2):185–91.
Article23. Matsune K, Miyoshi K, Kosaki R, Ohashi H, Maeda T. Taste after reduction of the tongue in Beckwith-Wiedemann syndrome. Br J Oral Maxillofac Surg. 2006; Feb. 44(1):49–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A CASE OF TONGUE RESECTION IN MACROGLOSSIA AS A PRESENTATION OF BECKWITH-WIEDEMANN SYNDROME
- A Case of Beckwith-Wiedemann Syndrome
- Beckwith-Wiedemann Sydrome with Left Adrenal Cortical Neoplasm
- Testicular Yolk Sac Tumor in Beckwith-Wiedemann Syndrome
- A study on changes of airway, tongue, and hyoid position following orthognathic surgery