Ann Rehabil Med.
2023 Feb;47(1):52-67. 10.5535/arm.22126.
Outcomes of a Multi-Modal Hospital-Associated Home-Based Cancer Prehabilitation Program
- Affiliations
-
- 1Department of Rehabilitation Medicine, Changi General Hospital, Singapore
- KMID: 2539728
- DOI: http://doi.org/10.5535/arm.22126
Abstract
Objective
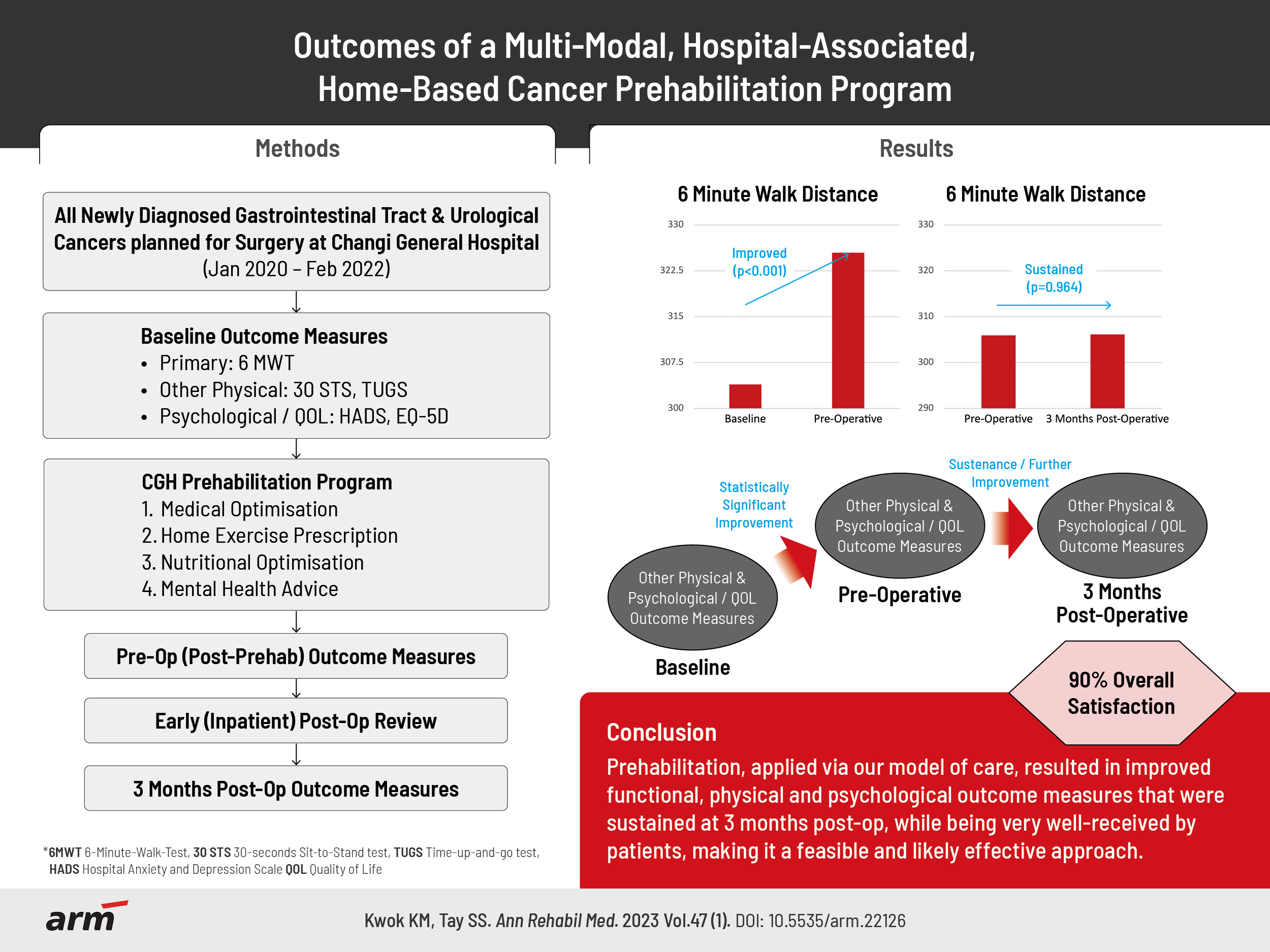
To assess the impact of a “one-stop”, multi-modal, hospital-associated-home-based prehabilitation model, helmed by a small core team, on newly diagnosed gastrointestinal and urological cancer patients planned for surgery.
Methods
This is a retrospective study in a tertiary public hospital, involving all newly diagnosed gastrointestinal and urological cancer patients planned for surgery. The primary outcome measure was the 6-minute walk test (6MWT). Other outcomes included physical, psychological and quality-of-life measures, and patient satisfaction surveys, taken at baseline, pre-operatively (post-prehabilitation), and at 3 months post-operatively.
Results
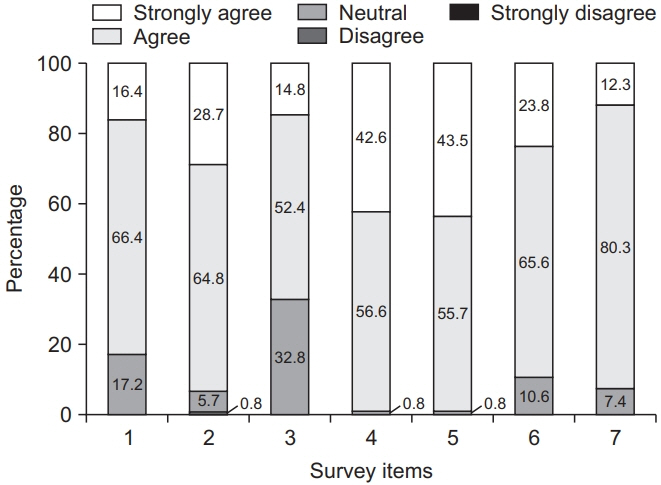
When comparing the baseline to pre-operatively (post-prehabilitation), there was a statistically significant improvement in the 6MWT (21.52 m, p<0.001), 30-Second Sit to Stand test (STS) (1.08 repetitions, p<0.001), Timed Up and Go test (TUG) (0.83 seconds, p=0.014) and Hospital Anxiety and Depression Scale (HADS) (total score 1.77, p<0.001). These were sustained (6MWT: 0.22, p=0.964; STS: 0.08 repetitions, p=0.863; TUG: 0.04 seconds, p=0.939) or further improved (HADS total score 2.06, p=0.003) at 3 months post-operatively. There was also a statistically significant improvement in the EuroQol-5 dimension health score (health-related quality-of-life measure) from baseline to 3 months post-operatively (7.04 points, p=0.001), with more than 90% overall patient satisfaction reported.
Conclusion
Prehabilitation applied via our model resulted in significant improvements in functional capacity, psychological and quality-of-life outcomes, sustained at 3 months post-operatively, and is a feasible and effective approach that is well-received by our patients.
Keyword
Figure
Reference
-
1. Silver JK, Baima J. Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am J Phys Med Rehabil. 2013; 92:715–27.2. Michael CM, Lehrer EJ, Schmitz KH, Zaorsky NG. Prehabilitation exercise therapy for cancer: a systematic review and meta-analysis. Cancer Med. 2021; 10:4195–205.3. Waterland JL, McCourt O, Edbrooke L, Granger CL, Ismail H, Riedel B, et al. Efficacy of prehabilitation including exercise on postoperative outcomes following abdominal cancer surgery: a systematic review and meta-analysis. Front Surg. 2021; 8:628848.4. McIsaac DI, Gill M, Boland L, Hutton B, Branje K, Shaw J, Prehabilitation Knowledge Network, et al. Prehabilitation in adult patients undergoing surgery: an umbrella review of systematic reviews. Br J Anaesth. 2022; 128:244–57.5. Treanor C, Kyaw T, Donnelly M. An international review and meta-analysis of prehabilitation compared to usual care for cancer patients. J Cancer Surviv. 2018; 12:64–73.6. Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014; 121:937–47.7. Santa Mina D, Hilton WJ, Matthew AG, Awasthi R, Bousquet-Dion G, Alibhai SMH, et al. Prehabilitation for radical prostatectomy: a multicentre randomized controlled trial. Surg Oncol. 2018; 27:289–98.8. Bundred JR, Kamarajah SK, Hammond JS, Wilson CH, Prentis J, Pandanaboyana S. Prehabilitation prior to surgery for pancreatic cancer: a systematic review. Pancreatology. 2020; 20:1243–50.9. Santa Mina D, Brahmbhatt P, Lopez C, Baima J, Gillis C, Trachtenberg L, et al. The case for prehabilitation prior to breast cancer treatment. PM R. 2017; 9(9S2):S305–16.10. Winningham ML, MacVicar MG, Bondoc M, Anderson JI, Minton JP. Effect of aerobic exercise on body weight and composition in patients with breast cancer on adjuvant chemotherapy. Oncol Nurs Forum. 1989; 16:683–9.11. MacVicar MG, Winningham ML, Nickel JL. Effects of aerobic interval training on cancer patients’ functional capacity. Nurs Res. 1989; 38:348–51.12. Winningham ML, MacVicar MG. The effect of aerobic exercise on patient reports of nausea. Oncol Nurs Forum. 1988; 15:447–50.13. Jones LW, Alfano CM. Exercise-oncology research: past, present, and future. Acta Oncol. 2013; 52:195–215.14. Clifford BK, Mizrahi D, Sandler CX, Barry BK, Simar D, Wakefield CE, et al. Barriers and facilitators of exercise experienced by cancer survivors: a mixed methods systematic review. Support Care Cancer. 2018; 26:685–700.15. Wong JN, McAuley E, Trinh L. Physical activity programming and counseling preferences among cancer survivors: a systematic review. Int J Behav Nutr Phys Act. 2018; 15:48.16. Santa Mina D, Au D, Auger LE, Alibhai SMH, Matthew AG, Sabiston CM, et al. Development, implementation, and effects of a cancer center’s exercise-oncology program. Cancer. 2019; 125:3437–47.17. Tay SS, Meng KK. Setting up a cancer prehabilitation framework in Singapore. J Cancer Rehabil. 2021; 4:1–6.18. Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015; 47:2473–9. Erratum in: Med Sci Sports Exerc 2016;48:579.19. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, American College of Sports Medicine, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011; 43:1334–59.20. Zhang Y, Tan S, Wu G. ESPEN practical guideline: clinical nutrition in surgery. Clin Nutr. 2021; 40:5071.21. Chia CL, Mantoo SK, Tan KY. ‘Start to finish transinstitutional transdisciplinary care’: a novel approach improves colorectal surgical results in frail elderly patients. Colorectal Dis. 2016; 18:O43–50.22. Tay MRJ, Wong CJ. Cancer rehabilitation-improving cancer survivorship in Singapore. Asia Pac J Oncol Nurs. 2021; 8:346–48.23. Waterland JL, Ismail H, Granger CL, Patrick C, Denehy L, Riedel B; Centre for Prehabilitation and Perioperative Care. Prehabilitation in high-risk patients scheduled for major abdominal cancer surgery: a feasibility study. Perioper Med (Lond). 2022; 11:32.24. Shaw JF, Mulpuru S, Kendzerska T, Moloo H, Martel G, Eskander A, et al. Association between frailty and patient outcomes after cancer surgery: a population-based cohort study. Br J Anaesth. 2022; 128:457–64.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prehabilitation for medically frail patients undergoing surgery for epithelial ovarian cancer: a cost-effectiveness analysis
- Effect of prehabilitation on patients with frailty undergoing colorectal cancer surgery: a systematic review and meta-analysis
- The changes in muscle strength and relaxation time after a comprehensive rehabilitation program for patients with myotonic dystrophy
- Effect of Multi-modal Interventions for Smoking Cessation in a University Setting: A Short Course of Varenicline, Financial Incentives, E-mail and Short Message Service
- Outcomes of an outpatient home-based prehabilitation program before pancreaticoduodenectomy: A retrospective cohort study