Korean J Gastroenterol.
2023 Feb;81(2):95-99. 10.4166/kjg.2022.118.
Left Side Appendicitis with Abscess Caused by Midgut Malrotation Mimicked by Complicated Diverticulitis of Sigmoid Colon: A Case Report
- Affiliations
-
- 1Department of Surgery, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- KMID: 2539579
- DOI: http://doi.org/10.4166/kjg.2022.118
Abstract
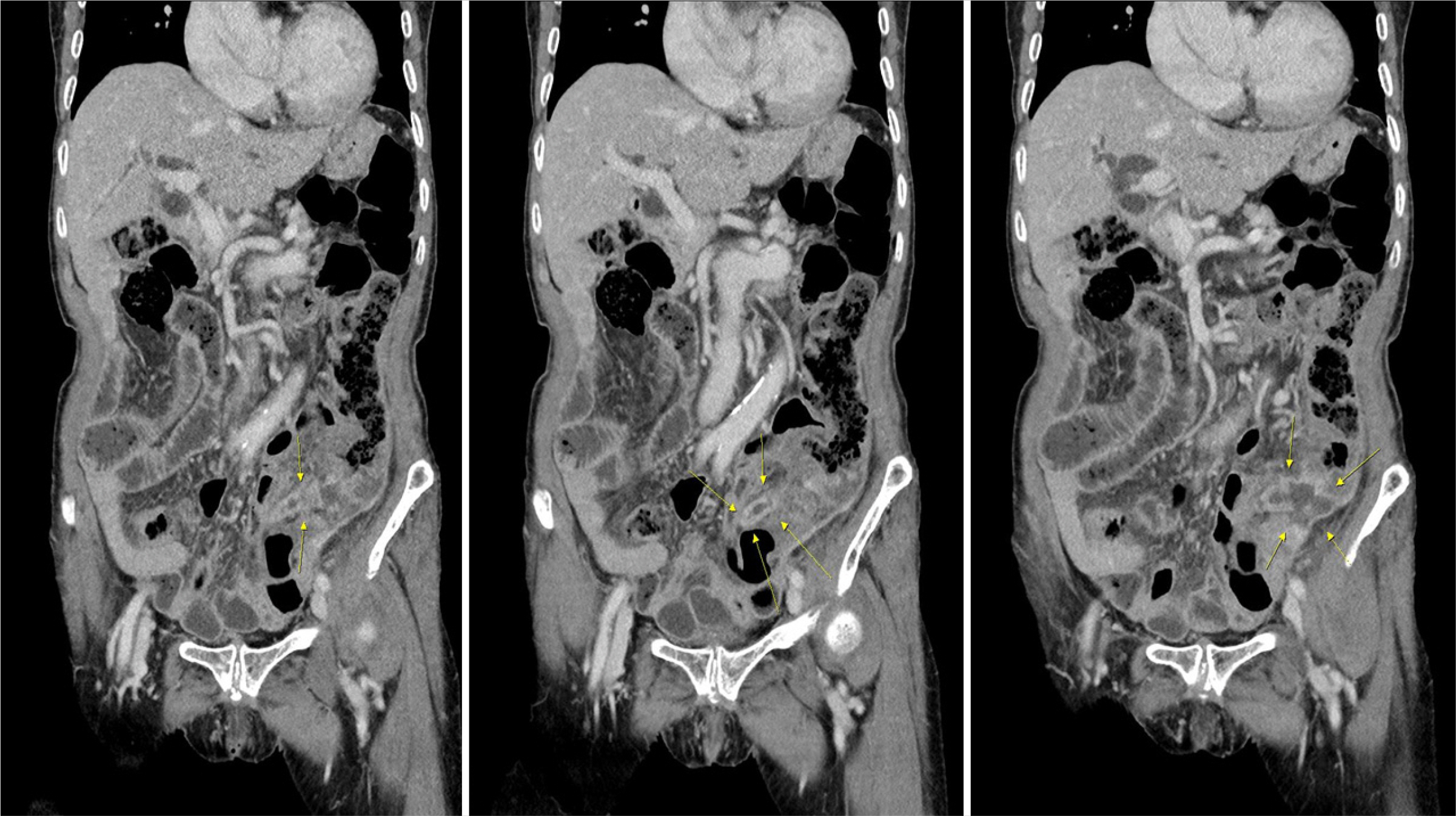
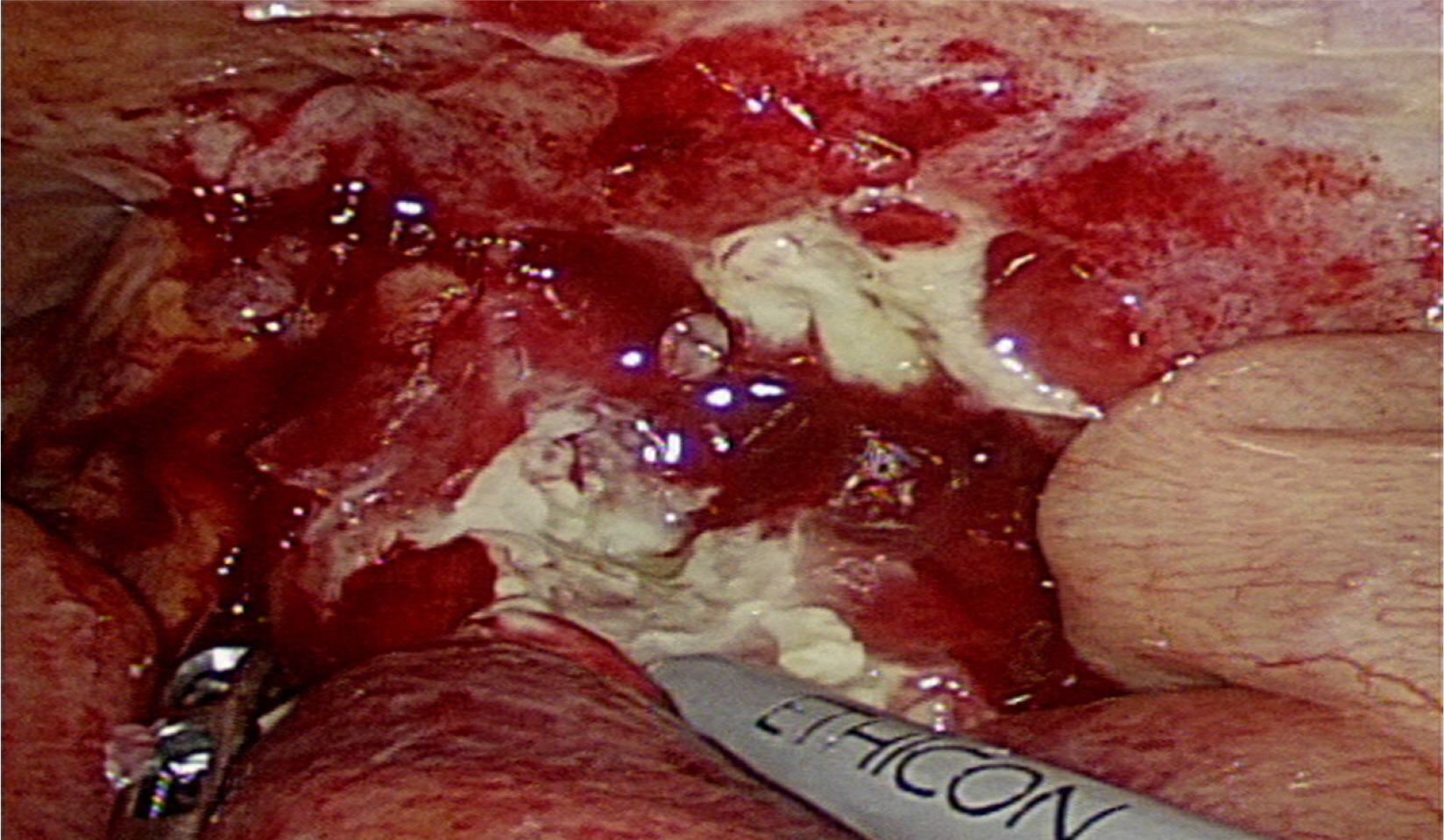
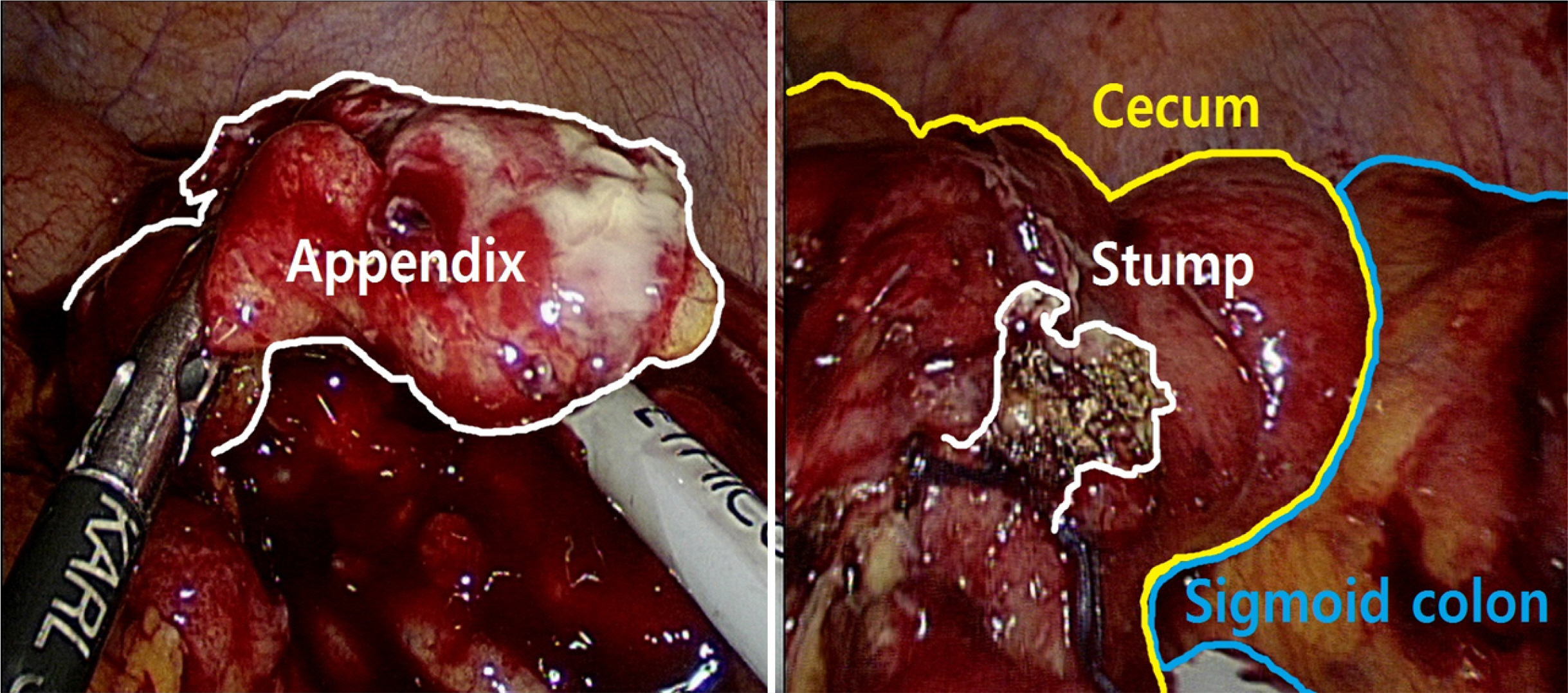
- Midgut malrotation (MM) is a rare anatomical abnormality that complicates the diagnosis and management of acute abdominal pain. Moreover, appendicitis and diverticulitis of the sigmoid colon can be considered when there is pain in the lower left abdomen. The patient in this case report was an 86-year-old female who had continuous abdominal pain two days before the visit to the emergency room. Abdominopelvic computed tomography revealed MM, and uneven concentric wall thickening from the distal descending colon to the proximal sigmoid colon with surrounding fatty infiltration was confirmed in the left lower abdomen. Moreover, the possibility of left-sided appendicitis due to MM could not be excluded. The patient’s abdominal pain increased next day. The surgery was performed laparoscopically, and the location of the appendix was reversed. The surgical findings revealed an abscess caused by perforation from inflammation of the proximal part of the appendix, and the sigmoid colon adhered mildly to the side immediately behind the abscess cavity. The base of the appendix was intact, and only an appendectomy was performed. Left-sided appendicitis due to MM was discriminated from the diverticulitis of the sigmoid colon. Diagnostic laparoscopic surgery through a physical examination based on the surgeon’s experience is important.
Figure
Reference
-
1. Oba T, Yamada T, Matsuda A, et al. 2021; Patient backgrounds and short-term outcomes of complicated appendicitis differ from those of uncomplicated appendicitis. Ann Gastroenterol Surg. 6:273–281. DOI: 10.1002/ags3.12523. PMID: 35261953. PMCID: PMC8889856.
Article2. Stull MC, Servey JT, Hale DF. 2022; A practical guide to appendicitis evaluation and treatment. J Fam Pract. 71:11–17. DOI: 10.12788/jfp.0341. PMID: 35259325.
Article3. Talan DA. 2022; Diagnosis and management of acute appendicitis. JAMA. 327:1183. DOI: 10.1001/jama.2022.1262. PMID: 35315898.
Article4. Peng S, Biggar M. 2022; Left sided appendicitis. ANZ J Surg. 92:3343–3344. DOI: 10.1111/ans.17600. PMID: 35322525.
Article5. Akbulut S, Caliskan A, Ekin A, Yagmur Y. 2010; Left-sided acute appendicitis with situs inversus totalis: review of 63 published cases and report of two cases. J Gastrointest Surg. 14:1422–1428. DOI: 10.1007/s11605-010-1210-2. PMID: 20567931.
Article6. Akbulut S, Ulku A, Senol A, Tas M, Yagmur Y. 2010; Left-sided appendicitis: review of 95 published cases and a case report. World J Gastroenterol. 16:5598–5602. DOI: 10.3748/wjg.v16.i44.5598. PMID: 21105193. PMCID: PMC2992678.
Article7. Birnbaum DJ, Geffroy Y, Goin G, Balandraud P. 2013; Left side appendicitis with midgut malrotation in an adult. J Surg Tech Case Rep. 5:38–40. DOI: 10.4103/2006-8808.118627. PMID: 24470850. PMCID: PMC3889003.
Article8. Kusumo Rahardjo A. 2022; Case series: Treatment outcome of late presentation of acute appendicitis. Int J Surg Case Rep. 92:106881. DOI: 10.1016/j.ijscr.2022.106881. PMID: 35231734. PMCID: PMC8885464.
Article9. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. 2015; Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 386:1278–1287. Erratum in: Lancet 2017;390:1736. DOI: 10.1016/S0140-6736(15)00275-5. PMID: 26460662.
Article10. Moris D, Paulson EK, Pappas TN. 2021; Diagnosis and management of acute appendicitis in adults: a review. JAMA. 326:2299–2311. DOI: 10.1001/jama.2021.20502. PMID: 34905026.
Article11. Fernandez EM, Favre Rizzo J, Arteaga González I, Hernández Hernández JR. 2014; Left-sided appendicitis: diagnosis and minimally invasive treatment. Acta Gastroenterol Latinoam. 44:62–66.12. Lin JN, Lou CC, Wang KL. 1995; Intestinal malrotation and midgut volvulus: a 15-year review. J Formos Med Assoc. 94:178–181.13. Strouse PJ. 2004; Disorders of intestinal rotation and fixation ("malrotation"). Pediatr Radiol. 34:837–851. DOI: 10.1007/s00247-004-1279-4. PMID: 15378215.
Article14. Chen W, Guo Z, Qian L, Wang L. 2020; Comorbidities in situs inversus totalis: A hospital-based study. Birth Defects Res. 112:418–426. DOI: 10.1002/bdr2.1652. PMID: 31994846.
Article15. Spoon JM. 2001; Situs inversus totalis. Neonatal Netw. 20:59–63. DOI: 10.1891/0730-0832.20.1.63. PMID: 12143842.
Article16. Kobus C, Targarona EM, Bendahan GE, et al. 2004; Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbecks Arch Surg. 389:396–399. DOI: 10.1007/s00423-004-0500-0. PMID: 15243744.
Article17. Perera WR, Hennessy OF. 2010; An unusual case of appendicitis. Am J Surg. 199:e79–81. DOI: 10.1016/j.amjsurg.2009.08.047. PMID: 20189162.
Article18. Miheţiu AF, Bratu DG, Popescu OM, Juravle C, Dumitrean IE, Chicea R. 2021; A rare case of situs inversus totalis associated with sigmoid diverticulitis and appendicular agenesis. Embryological, clinical considerations and literature review. Rom J Morphol Embryol. 62:861–867. DOI: 10.47162/RJME.62.3.27. PMID: 35263418. PMCID: PMC9019675.
Article19. Perez AA, Pickhardt PJ. 2021; Intestinal malrotation in adults: prevalence and findings based on CT colonography. Abdom Radiol (NY). 46:3002–3010. DOI: 10.1007/s00261-021-02959-3. PMID: 33558953.
Article20. Rincon-Sanchez RAM, Ramirez-Barranco R. 2020; [Intestinal malrotation in adults diagnosed after presentation of post polypectomy syndrome in the cecum: report of a case]. Rev Gastroenterol Peru. 40:185–187. Spanish. DOI: 10.47892/rgp.2020.402.1089. PMID: 32876637.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Right side fixation of sigmoid colon with a hepato-sigmoidocolic fistula in patient with hepatocellular carcinoma and midgut malrotation
- Colouterine Fistula Caused by Diverticulitis of the Sigmoid Colon
- Appendico-Sigmoid Fistula Due to Appendicitis
- Left Sided Appendicitis in Patient with Intestinal Malrotation
- Diverticulitis of the Cecum and Ascending Colon