Ann Hepatobiliary Pancreat Surg.
2023 Feb;27(1):95-101. 10.14701/ahbps.22-036.
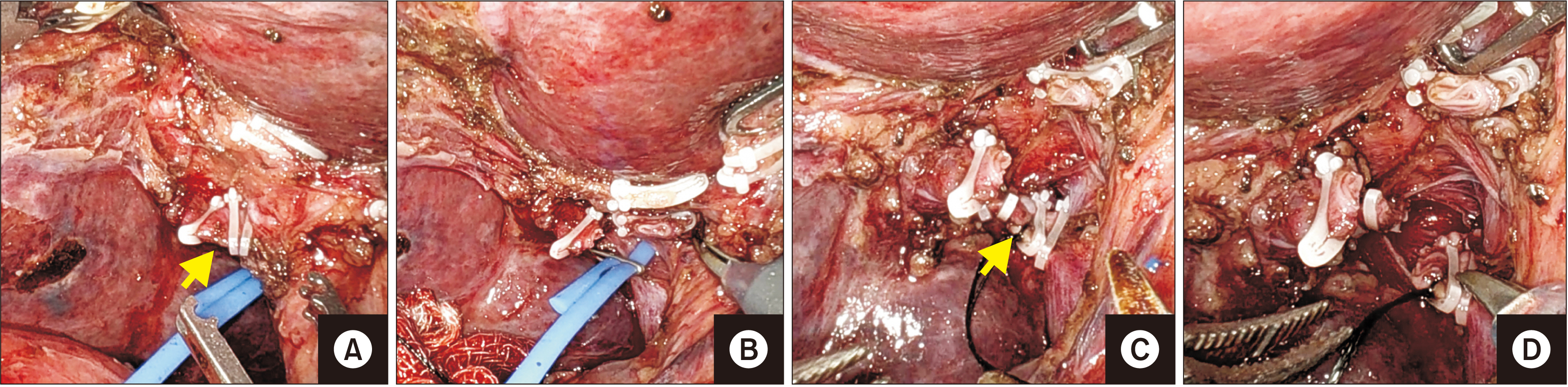
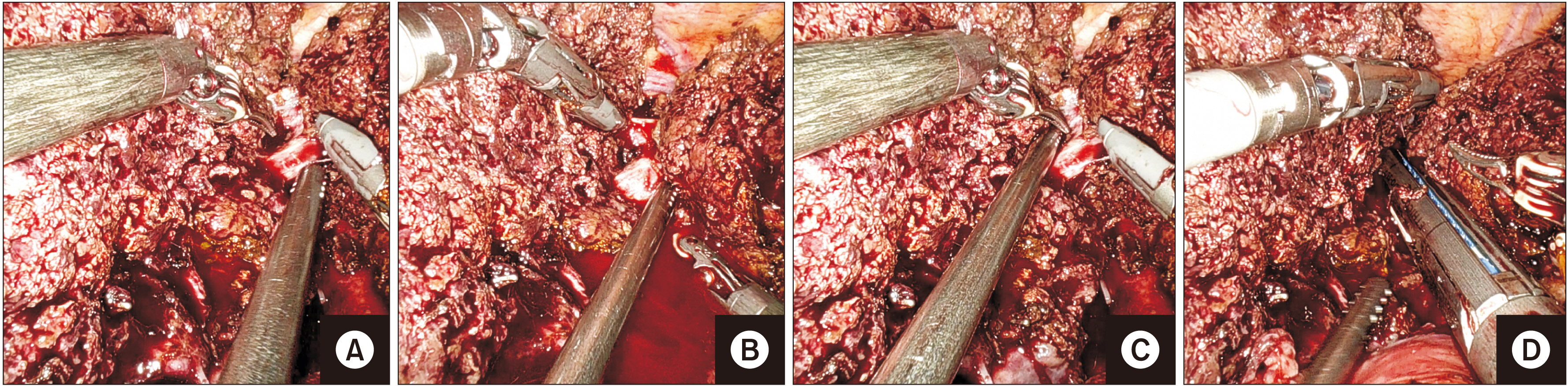
Total robotic right hepatectomy for multifocal hepatocellular carcinoma using vessel sealer
- Affiliations
-
- 1Department of Surgical Gastroenterology, All India Institute of Medical Sciences, Jodhpur, India
- KMID: 2539519
- DOI: http://doi.org/10.14701/ahbps.22-036
Abstract
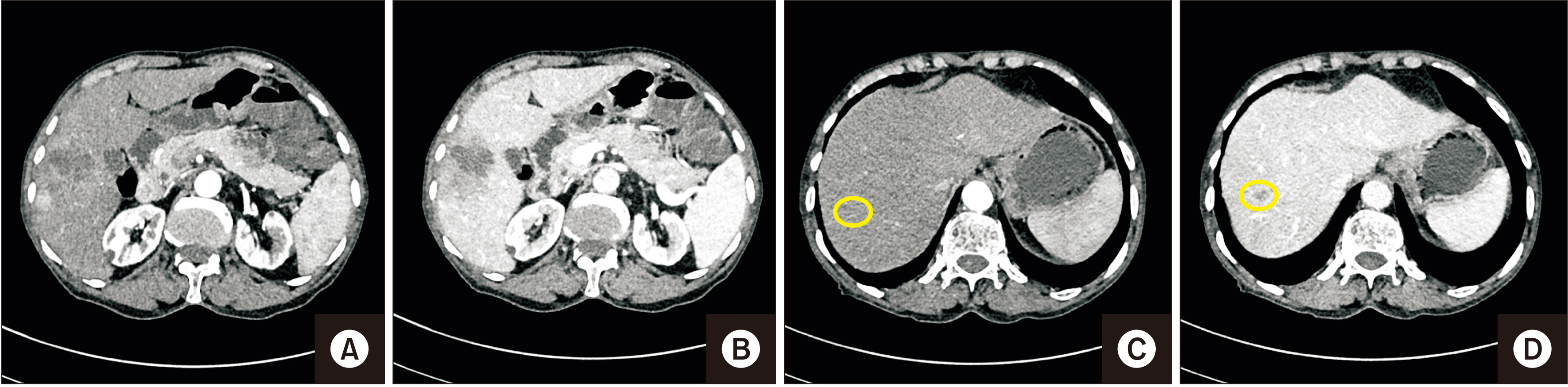
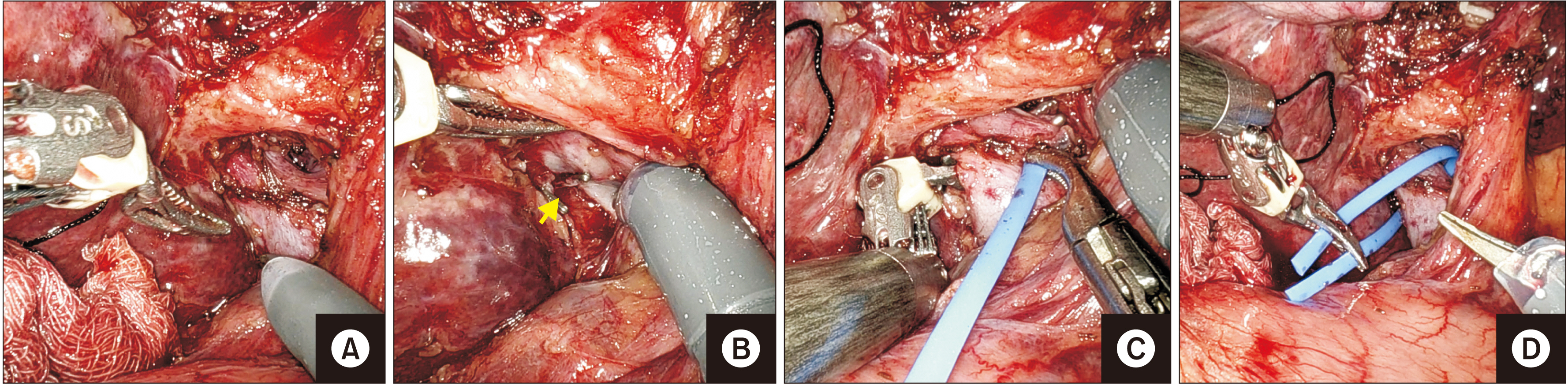
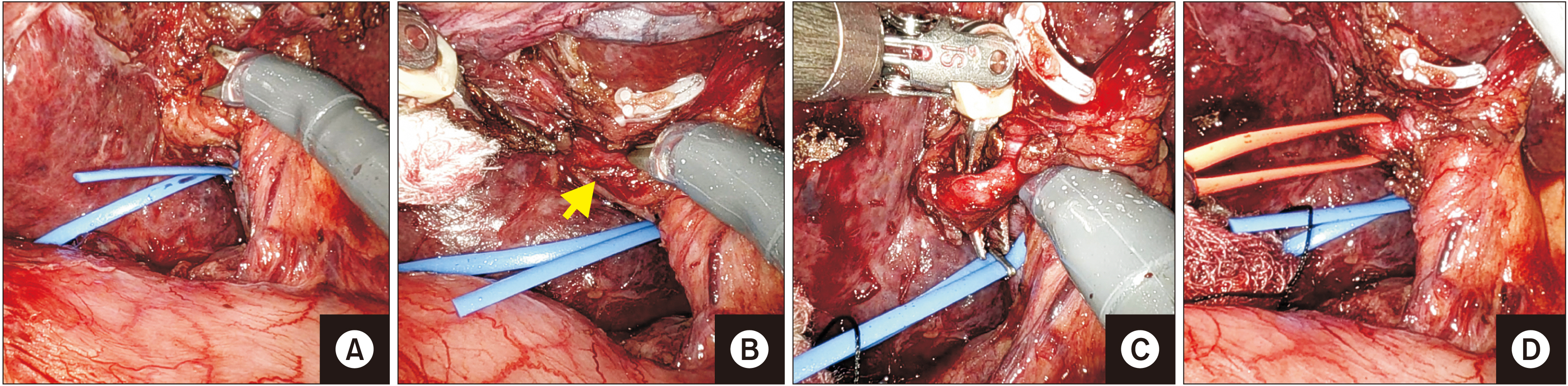
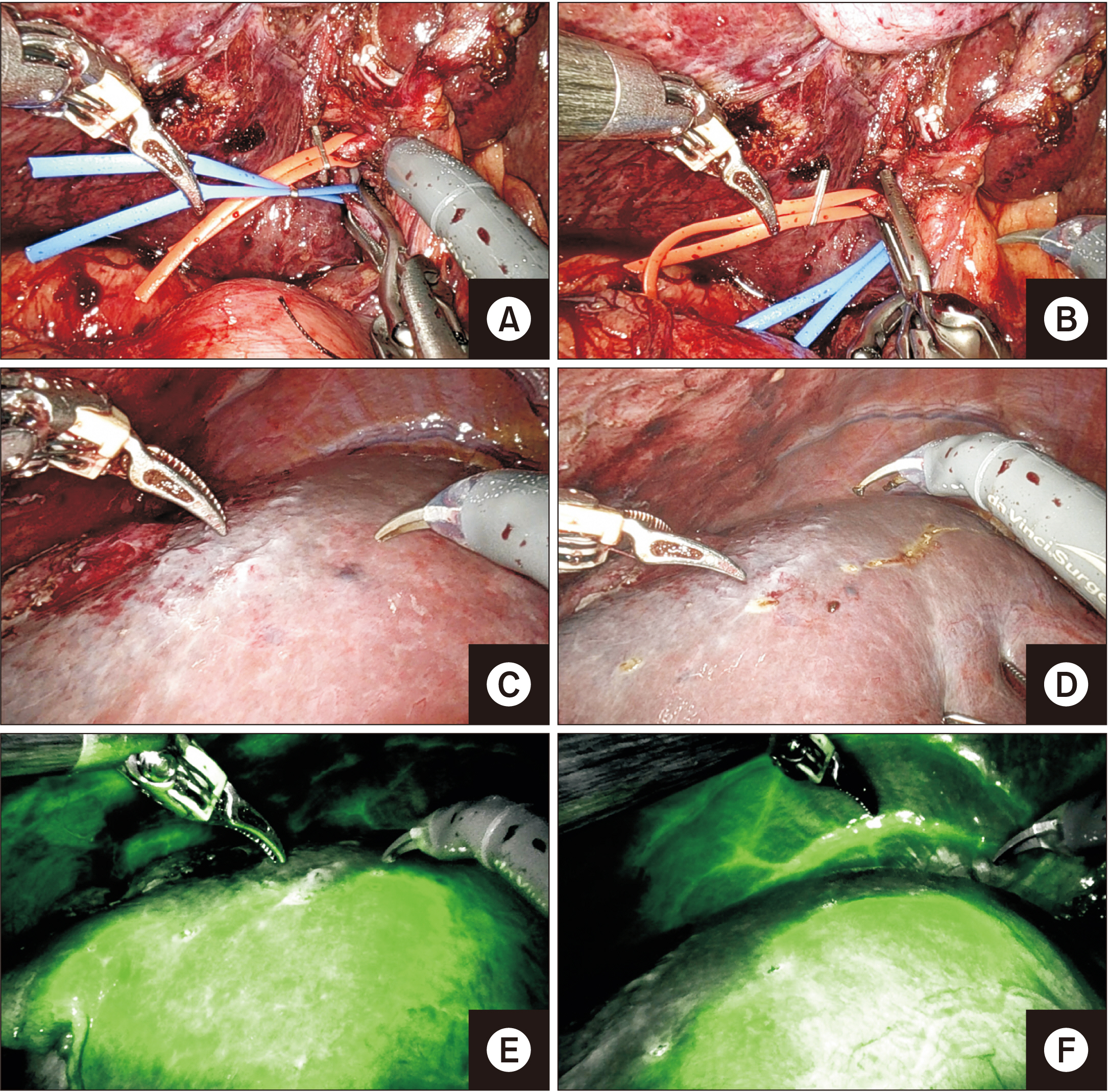
- Rapid adoption of a robotic approach as a minimally invasive surgery tool has enabled surgeons to perform more complex hepatobiliary surgeries than conventional laparoscopic surgery. Although various types of liver resections have been performed robotically, parenchymal transection is challenging as commonly used instruments (Cavitron Ultrasonic Surgical Aspirator [CUSA] and Harmonic) lack articulation. Further, CUSA also requires a patient-side assistant surgeon with hepatobiliary laparoscopic skills. We present a case report of total robotic right hepatectomy for multifocal hepatocellular carcinoma in a 70-year-old male using ‘Vessel Sealer’ for parenchymal transection. Total operative time was 520 minutes with a blood loss of ~400 mL. There was no technical difficulty or instrument failure encountered during surgery. The patient was discharged on postoperative day five without any significant complications such as bile leak. Thus, Vessel Sealer, a fully articulating instrument intended to seal vessels and tissues up to 7 mm, can be a promising tool for parenchymal transection in a robotic surgery.
Figure
Reference
-
1. Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. 2003; Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 138:777–784. DOI: 10.1001/archsurg.138.7.777. PMID: 12860761.2. Nota CL, Molenaar IQ, te Riele WW, van Santvoort HC, Borel Rinkes IHM, Hagendoorn J. 2020; Parenchymal transection in robotic liver resection: results of 70 resections using the Vessel Sealer. Mini-invasive Surg. 4:74. DOI: 10.20517/2574-1225.2020.57.
Article3. Zhang L, Yuan Q, Xu Y, Wang W. 2020; Comparative clinical outcomes of robot-assisted liver resection versus laparoscopic liver resection: a meta-analysis. PLoS One. 15:e0240593. DOI: 10.1371/journal.pone.0240593. PMID: 33048989. PMCID: PMC7553328.
Article4. Liu R, Wakabayashi G, Kim HJ, Choi GH, Yiengpruksawan A, Fong Y, et al. 2019; International consensus statement on robotic hepatectomy surgery in 2018. World J Gastroenterol. 25:1432–1444. DOI: 10.3748/wjg.v25.i12.1432. PMID: 30948907. PMCID: PMC6441912.
Article5. Choi SB, Park JS, Kim JK, Hyung WJ, Kim KS, Yoon DS, et al. 2008; Early experiences of robotic-assisted laparoscopic liver resection. Yonsei Med J. 49:632–638. DOI: 10.3349/ymj.2008.49.4.632. PMID: 18729307. PMCID: PMC2615291.
Article6. Croner RS, Perrakis A, Brunner M, Matzel KE, Hohenberger W. 2015; Pioneering robotic liver surgery in Germany: first experiences with liver malignancies. Front Surg. 2:18. DOI: 10.3389/fsurg.2015.00018. PMID: 26052515. PMCID: PMC4440394.
Article7. Quijano Y, Vicente E, Ielpo B, Duran H, Diaz E, Fabra I, et al. 2017; Hepatobilio-pancreatic robotic surgery: initial experience from a single center institute. J Robot Surg. 11:355–365. DOI: 10.1007/s11701-016-0663-z. PMID: 28039607.
Article8. Giulianotti PC, Tzvetanov I, Jeon H, Bianco F, Spaggiari M, Oberholzer J, et al. 2012; Robot-assisted right lobe donor hepatectomy. Transpl Int. 25:e5–e9. DOI: 10.1111/j.1432-2277.2011.01373.x. PMID: 22029717.
Article9. Machado MAC, Lobo-Filho MM, Mattos BH, Ardengh AO, Makdissi FF. 2021; Robotic liver resection. Report of the first 50 cases. Arq Gastroenterol. 58:514–519. DOI: 10.1590/s0004-2803.202100000-92. PMID: 34909859.
Article10. Wong DJ, Wong MJ, Choi GH, Wu YM, Lai PB, Goh BKP. 2019; Systematic review and meta-analysis of robotic versus open hepatectomy. ANZ J Surg. 89:165–170. DOI: 10.1111/ans.14690. PMID: 29943881.
Article11. Ziogas IA, Giannis D, Esagian SM, Economopoulos KP, Tohme S, Geller DA. 2021; Laparoscopic versus robotic major hepatectomy: a systematic review and meta-analysis. Surg Endosc. 35:524–535. DOI: 10.1007/s00464-020-08008-2. PMID: 32989544.
Article12. Cortolillo N, Patel C, Parreco J, Kaza S, Castillo A. 2019; Nationwide outcomes and costs of laparoscopic and robotic vs. open hepatectomy. J Robot Surg. 13:557–565. DOI: 10.1007/s11701-018-0896-0. PMID: 30484059.
Article13. Daskalaki D, Gonzalez-Heredia R, Brown M, Bianco FM, Tzvetanov I, Davis M, et al. 2017; Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A. 27:375–382. DOI: 10.1089/lap.2016.0576. PMID: 28186429. PMCID: PMC5397272.
Article14. Sham JG, Richards MK, Seo YD, Pillarisetty VG, Yeung RS, Park JO. 2016; Efficacy and cost of robotic hepatectomy: is the robot cost-prohibitive? J Robot Surg. 10:307–313. DOI: 10.1007/s11701-016-0598-4. PMID: 27153838.
Article15. Kingham TP, Leung U, Kuk D, Gönen M, D'Angelica MI, Allen PJ, et al. 2016; Robotic liver resection: a case-matched comparison. World J Surg. 40:1422–1428. DOI: 10.1007/s00268-016-3446-9. PMID: 26913732. PMCID: PMC4870111.
Article16. Ortenzi M, Ghiselli R, Baldarelli M, Cardinali L, Guerrieri M. 2018; Is the bipolar vessel sealer device an effective tool in robotic surgery? A retrospective analysis of our experience and a meta-analysis of the literature about different robotic procedures by investigating operative data and post-operative course. Minim Invasive Ther Allied Technol. 27:113–118. DOI: 10.1080/13645706.2017.1329212. PMID: 28604140.
Article17. Kong SH, Kim TH, Huh YJ, Oh SY, Ahn HS, Park SY, et al. 2017; A feasibility study and technical tips for the use of an articulating bipolar vessel sealer in da Vinci robot-assisted gastrectomy. J Laparoendosc Adv Surg Tech A. 27:1172–1179. DOI: 10.1089/lap.2017.0093. PMID: 28622078.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical techniques for robotic right donor hepatectomy, part 1: robotic hilar dissection and right lobe mobilization
- Surgical techniques for robotic right donor hepatectomy, part 2: robotic parenchymal transection and bile duct division
- The method of using robotic Harmonic ACE curved shears for parenchymal transection in robotic hepatectomy
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- Current status of robotic surgery for liver transplantation