J Korean Med Sci.
2023 Jan;38(4):e17. 10.3346/jkms.2023.38.e17.
Sex Differences in COVID-19 Infection Fear in a Community Sample of Korean Adults Using Quantile Regression
- Affiliations
-
- 1College of Nursing, The Catholic University of Korea, Seoul, Korea
- 2Department of Psychiatry, College of Medicine, Jeju National University, Jeju, Korea
- 3College of Nursing, University of Illinois at Chicago, Chicago, IL, USA
- 4Department of Psychiatry, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2539188
- DOI: http://doi.org/10.3346/jkms.2023.38.e17
Abstract
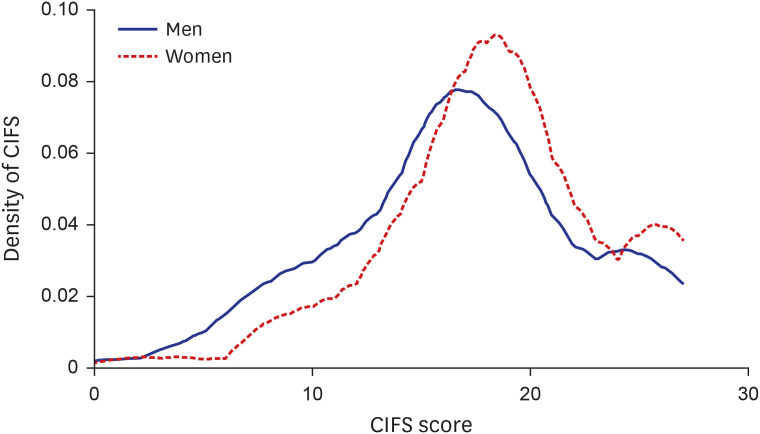
- This study aims to explore the impact of distributional changes in coronavirus disease 2019 (COVID-19) infection fear with sex differences. A quota sampling strategy was followed and 483 Korean adults were surveyed in a community sample. Self-report questionnaires were used to assess COVID-19 infection fear, depressive symptoms, and general characteristics. Quantile regression was used to explore the regression relationship of COVID-19 infection fear and an individual’s sex. There was a significant difference in COVID-19 infection fear (P= 0.001) and depression (P = 0.008) between the sexes - male and female. The differences between sexes at the 20th and 30th percentiles were significant (β = 2.04, P = 0.006; β = 1.5, P = 0.004, respectively). The results demonstrate that sex significantly predicts COVID-19 infection fear and women had significantly greater fear than men in the mild-level of COVID-19 infection fear.
Keyword
Figure
Cited by 1 articles
-
Factors Affecting Fear of COVID-19 Infection in Healthcare Workers in COVID-19 Dedicated Teams: Focus on Professional Quality of Life
Eulji Jung, Young-Eun Jung, Moon-Doo Kim
J Korean Med Sci. 2023;38(43):e366. doi: 10.3346/jkms.2023.38.e366.
Reference
-
1. Wu YC, Chen CS, Chan YJ. The outbreak of COVID-19: an overview. J Chin Med Assoc. 2020; 83(3):217–220. PMID: 32134861.2. Qian M, Jiang J. COVID-19 and social distancing. Z Gesundh Wiss. 2022; 30:259–261. PMID: 32837835.3. NHS Foundation Trust. Health anxiety. Updated 2020. Accessed April 7, 2020. https://www.nhs.uk/mental-health/conditions/health-anxiety/ .4. Asmundson GJ, Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: what all decision-makers, health authorities, and health care professionals need to know. J Anxiety Disord. 2020; 71:102211. PMID: 32179380.5. Wu Q, Zhuo L, Li H, Zheng L, Ma G, Tao H. Factors associated with the mental health of back-to-Wuhan university students based on quantile regression model during the COVID-19 period. BMC Psychiatry. 2022; 22(1):284. PMID: 35448992.6. Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. 2014; 35(3):320–330. PMID: 24887405.7. Vesga-López O, Schneier FR, Wang S, Heimberg RG, Liu SM, Hasin DS, et al. Gender differences in generalized anxiety disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. 2008; 69(10):1606–1616. PMID: 19192444.8. Korean Society for Traumatic Stress Studies. Coronavirus disease-19 1st National Mental Health Survey 2020. Updated 2020. Accessed April 7, 2020. http://kstss.kr/?p=1370 .9. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID: 11556941.10. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma. 2020; 12:S17–S21. PMID: 32496100.11. Martínez-Lorca M, Martínez-Lorca A, Criado-Álvarez JJ, Armesilla MD, Latorre JM. The fear of COVID-19 scale: validation in Spanish university students. Psychiatry Res. 2020; 293:113350. PMID: 32777619.12. Reznik A, Gritsenko V, Konstantinov V, Khamenka N, Isralowitz R. COVID-19 fear in Eastern Europe: validation of the fear of COVID-19 scale. Int J Ment Health Addict. 2021; 19(5):1903–1908. PMID: 32406404.13. Lee D, Kim Y, Lee D, Hwang H, Nam S, Kim J. The influence of public fear, and psycho-social experiences during the coronavirus disease 2019 (COVID-19) pandemic on depression and anxiety in South Korea. Korean J Couns Psychother. 2020; 32:2119–2156.14. Jung AR, Hong EJ. A study on anxiety, knowledge, infection possibility, preventive possibility and preventive behavior level of COVID-19 in general public. J Converg Inf Technol. 2020; 10:87–98.15. Cerda AA, García LY. Factors explaining the fear of being infected with COVID-19. Health Expect. 2022; 25(2):506–512. PMID: 33974721.16. Uz B, Savaşan E, Soğancı D. Anxiety, depression and burnout levels of Turkish healthcare workers at the end of the first period of COVID-19 pandemic in Turkey. Clin Psychopharmacol Neurosci. 2022; 20(1):97–108. PMID: 35078952.17. Bronfman N, Repetto P, Cordón P, Castañeda J, Cisternas P. Gender differences on psychosocial factors affecting COVID-19 preventive behaviors. Sustainability (Basel). 2021; 13(11):6148.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19–Related Functional Impairment in a Community Sample of Korean Adults: Associations With Depression, COVID-19 Infection Fear, and Resilience
- Factors Affecting Fear of COVID-19 Infection in Healthcare Workers in COVID-19 Dedicated Teams: Focus on Professional Quality of Life
- Factors Associated with Depression in Older Adults Living Alone during the COVID-19 Pandemic
- Factors influencing handwashing among community dwelling older adults, using the 2021 Community Health Survey: A secondary analysis study
- Fear of COVID-19 and Its Impact on Job Satisfaction and Turnover Intention Among Egyptian Physicians