J Stroke.
2023 Jan;25(1):101-110. 10.5853/jos.2022.01956.
Cerebral Edema in Patients with severe Hemispheric Syndrome: Incidence, Risk Factors, and Outcomes—Data from SITS-ISTR
- Affiliations
-
- 1Department of Neurology, University Hospital La FE, Valencia, Spain
- 2Neurovascular Research Laboratory, Biomedicine Institute IBiS, Sevilla, Spain
- 3Department of Neurology, Danderyd Hospital, Stockholm, Sweden
- 4Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden
- 5Department of Neurology, Heidelberg University Hospital, Heidelberg, Germany
- 6Department of Neurology, Sao Jose Hospital, University Hospital Lisboa, Lisboa, Portugal
- 7Department of Neuroscience, Integrate University Hospital, Verona, Italy
- 8Department of Neurology, North Estonia Medical Centre Foundation, Tallinn, Estonia
- 9Department of Neurology and Stroke Unit in Sandomierz, Collegium Medicum, Jan Kochanowski University in Kielce, Kielce, Poland
- 10Stroke Unit, Department of Neurology, San Carlos Clinic Hospital, Madrid, Spain
- 11Department of Human Neurosciences, Sapienza University of Rome, Rome, Italy
- 12Biogen, Cambridge, MA, USA
- 13Department of Neurology, Karolinska University Hospital, Stockholm, Sweden
- KMID: 2539062
- DOI: http://doi.org/10.5853/jos.2022.01956
Abstract
- Background and Purpose
Cerebral edema (CED) in ischemic stroke can worsen prognosis and about 70% of patients who develop severe CED die if treated conservatively. We aimed to describe incidence, risk factors and outcomes of CED in patients with extensive ischemia.
Methods
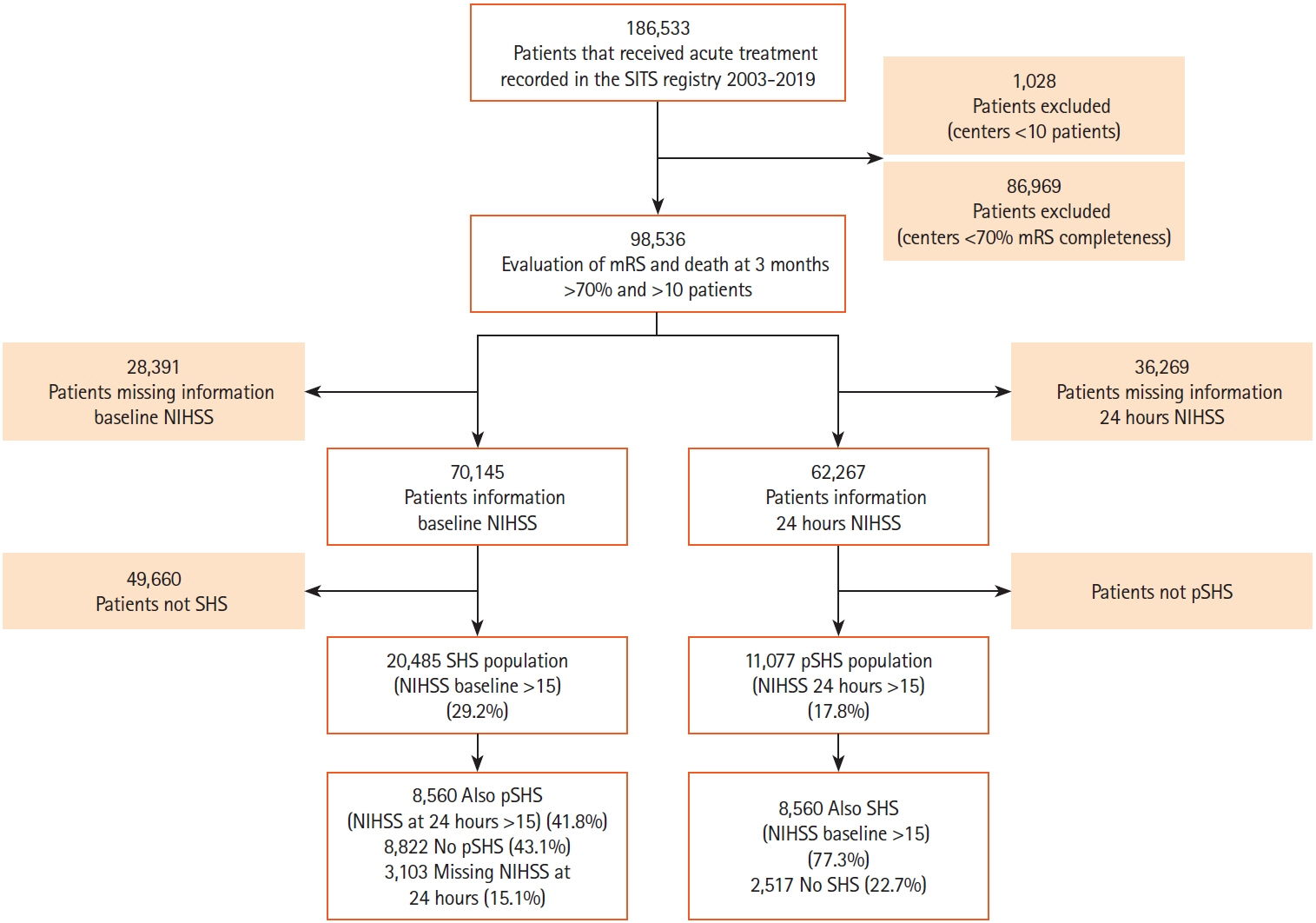
Oservational study based on Safe Implementation of Treatments in Stroke-International Stroke Treatment Registry (2003–2019). Severe hemispheric syndrome (SHS) at baseline and persistent SHS (pSHS) at 24 hours were defined as National Institutes of Health Stroke Score (NIHSS) >15. Outcomes were moderate/severe CED detected by neuroimaging, functional independence (modified Rankin Scale 0–2) and death at 90 days.
Results
Patients (n=8,560) presented with SHS and developed pSHS at 24 hours; 82.2% received intravenous thrombolysis (IVT), 10.5% IVT+thrombectomy, and 7.3% thrombectomy alone. Median age was 77 and NIHSS 21. Of 7,949 patients with CED data, 3,780 (47.6%) had any CED and 2,297 (28.9%) moderate/severe CED. In the multivariable analysis, age <50 years (relative risk [RR], 1.56), signs of acute infarct (RR, 1.29), hyperdense artery sign (RR, 1.39), blood glucose >128.5 mg/dL (RR, 1.21), and decreased level of consciousness (RR, 1.14) were associated with moderate/severe CED (for all P<0.05). Patients with moderate/severe CED had lower odds to achieve functional Independence (adjusted odds ratio [aOR], 0.35; 95% confidence interval [CI], 0.23 to 0.55) and higher odds of death at 90 days (aOR, 2.54; 95% CI, 2.14 to 3.02).
Conclusions
In patients with extensive ischemia, the most important predictors for moderate/ severe CED were age <50, high blood glucose, signs of acute infarct, hyperdense artery on baseline scans, and decreased level of consciousness. CED was associated with worse functional outcome and a higher risk of death at 3 months.
Keyword
Figure
Reference
-
References
1. Battey TW, Karki M, Singhal AB, Wu O, Sadaghiani S, Campbell BC, et al. Brain edema predicts outcome after nonlacunar ischemic stroke. Stroke. 2014; 45:3643–3648.2. Huttner HB, Schwab S. Malignant middle cerebral artery infarction: clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol. 2009; 8:949–958.3. Wijdicks EF, Sheth KN, Carter BS, Greer DM, Kasner SE, Kimberly WT, et al. Recommendations for the management of cerebral and cerebellar infarction with swelling: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:1222–1238.4. Torbey MT, Bösel J, Rhoney DH, Rincon F, Staykov D, Amar AP, et al. Evidence-based guidelines for the management of large hemispheric infarction: a statement for health care professionals from the Neurocritical Care Society and the German Society for Neuro-intensive Care and Emergency Medicine. Neurocrit Care. 2015; 22:146–164.5. Qureshi AI, Suarez JI, Yahia AM, Mohammad Y, Uzun G, Suri MF, et al. Timing of neurologic deterioration in massive middle cerebral artery infarction: a multicenter review. Crit Care Med. 2003; 31:272–277.6. Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007; 6:215–222.7. Wartenberg KE. Malignant middle cerebral artery infarction. Curr Opin Crit Care. 2012; 18:152–163.8. Hofmeijer J, Algra A, Kappelle LJ, van der Worp HB. Predictors of life-threatening brain edema in middle cerebral artery infarction. Cerebrovasc Dis. 2008; 25:176–184.9. Strbian D, Meretoja A, Putaala J, Kaste M, Tatlisumak T; Helsinki Stroke Thrombolysis Registry Group. Cerebral edema in acute ischemic stroke patients treated with intravenous thrombolysis. Int J Stroke. 2013; 8:529–534.10. Thorén M, Azevedo E, Dawson J, Egido JA, Falcou A, Ford GA, et al. Predictors for cerebral edema in acute ischemic stroke treated with intravenous thrombolysis. Stroke. 2017; 48:2464–2471.11. Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007; 369:275–282.12. Thorén M, Dixit A, Escudero-Martínez I, Gdovinová Z, Klecka L, Rand VM, et al. Effect of recanalization on cerebral edema in ischemic stroke treated with thrombolysis and/or endovascular therapy. Stroke. 2020; 51:216–223.13. Larrue V, von Kummer RR, Müller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 2001; 32:438–441.14. Li J, Zhang P, Wu S, Wang Y, Zhou J, Yi X, et al. Stroke-related complications in large hemisphere infarction: incidence and influence on unfavorable outcome. Ther Adv Neurol Disord. 2019; 12:1756286419873264.15. Du M, Huang X, Li S, Xu L, Yan B, Zhang Y, et al. A nomogram model to predict malignant cerebral edema in ischemic stroke patients treated with endovascular thrombectomy: an observational study. Neuropsychiatr Dis Treat. 2020; 16:2913–2920.16. Simard JM, Sheth KN, Kimberly WT, Stern BJ, del Zoppo GJ, Jacobson S, et al. Glibenclamide in cerebral ischemia and stroke. Neurocrit Care. 2014; 20:319–333.17. Ng FC, Yassi N, Sharma G, Brown SB, Goyal M, Majoie CBLM, et al. Cerebral edema in patients with large hemispheric infarct undergoing reperfusion treatment: a HERMES Meta-Analysis. Stroke. 2021; 52:3450–3458.18. Reinink H, Jüttler E, Hacke W, Hofmeijer J, Vicaut E, Vahedi K, et al. Surgical decompression for space-occupying hemispheric infarction: a systematic review and individual patient meta-analysis of randomized clinical trials. JAMA Neurol. 2021; 78:208–216.19. van der Worp HB, Hofmeijer J, Jüttler E, Lal A, Michel P, Santalucia P, et al. European Stroke Organisation (ESO) guidelines on the management of space-occupying brain infarction. Eur Stroke J. 2021; 6:XC–CX.20. Pledl HW, Hoyer C, Rausch J, Ebert AD, Seiz M, Arp M, et al. Decompressive hemicraniectomy in malignant middle cerebral artery infarction: the ‘Real World’ Beyond Studies. Eur Neurol. 2016; 76:48–56.21. Cook AM, Morgan Jones G, Hawryluk GW, Mailloux P, McLaughlin D, Papangelou A, et al. Guidelines for the acute treatment of cerebral edema in neurocritical care patients. Neurocrit Care. 2020; 32:647–666.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Where are We Now with Decompressive Hemicraniectomy for Malignant Middle Cerebral Artery Infarction?
- The Effectiveness of Decompressive Craniectomy with Dural Augmentation in Malignant Cerebral Infarction
- Exertional heat stroke with reversible severe cerebral edema
- Study on the Cerebral Laterality Pattern of Medical Students
- Cerebral Ptosis