Clin Endosc.
2023 Jan;56(1):119-124. 10.5946/ce.2021.081.
A large and pedunculated inflammatory pseudotumor with pseudosarcomatous change of the cecum mimicking a malignant polyp: a case report and literature review
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2538760
- DOI: http://doi.org/10.5946/ce.2021.081
Abstract
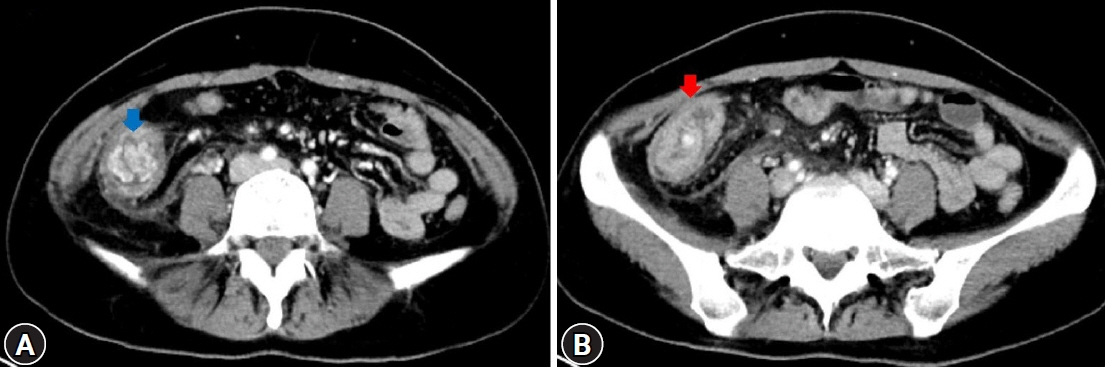
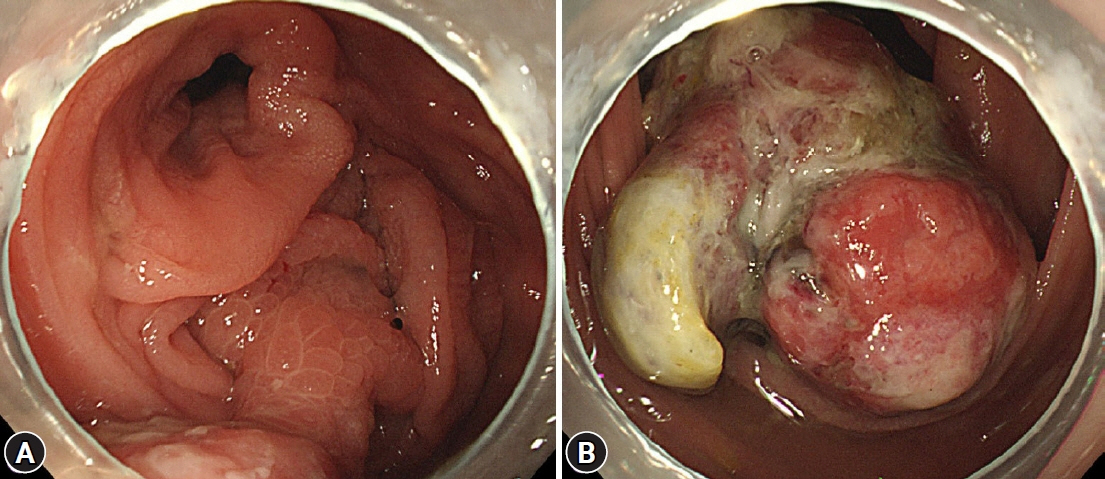
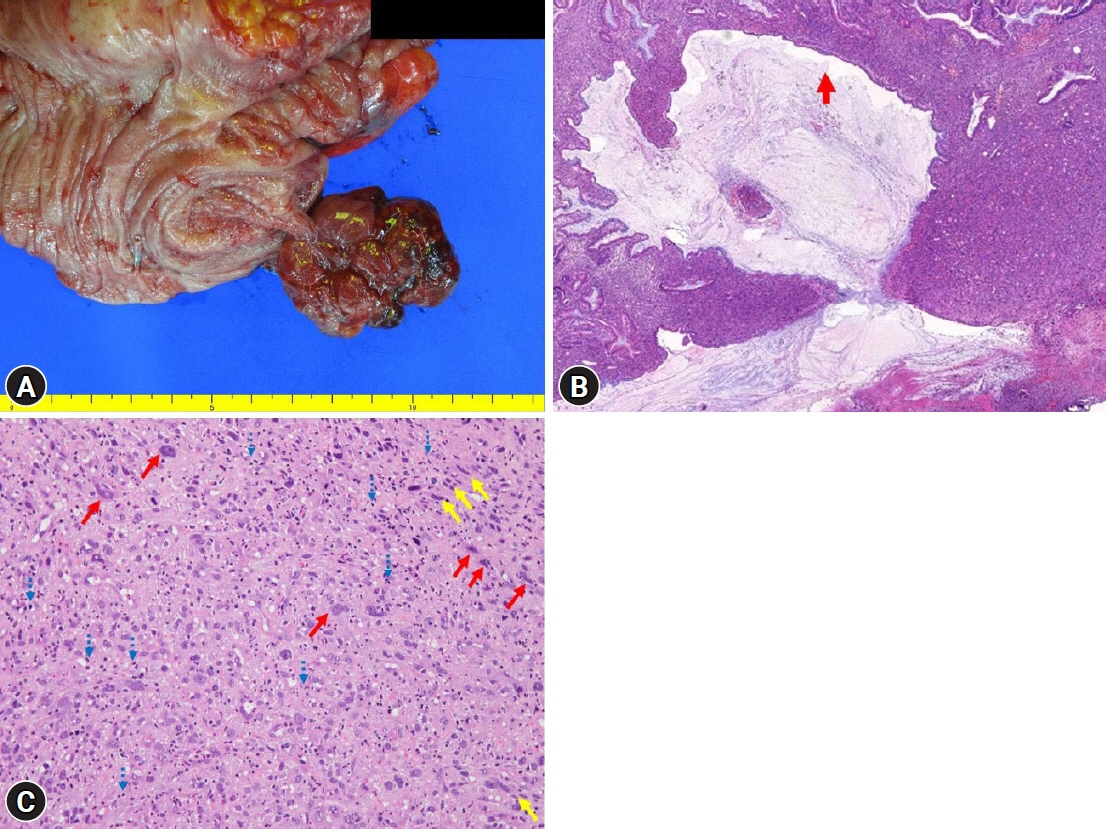
- Inflammatory pseudotumor (IPT) is a rare benign tumor of unknown etiology that can occur in almost any organ system. It has neoplastic features such as local recurrence, invasive growth, and vascular invasion, leading to the possibility of malignant sarcomatous changes. The clinical presentations of colonic IPT may include abdominal pain, anemia, a palpable mass, and intestinal obstruction. A few cases of colonic IPT have been reported, but colonic IPT with pedunculated morphology is very rare. Furthermore, since it can mimic malignant polyps, understanding the endoscopic findings of colonic IPT is important for proper treatment. Herein, we present a case of colonic IPT with pseudosarcomatous changes, presenting as a large polyp, mimicking a malignant polyp in the cecum, along with a literature review.
Keyword
Figure
Reference
-
1. Dehner LP. The enigmatic inflammatory pseudotumours: the current state of our understanding, or misunderstanding. J Pathol. 2000; 192:277–279.2. Narla LD, Newman B, Spottswood SS, et al. Inflammatory pseudotumor. Radiographics. 2003; 23:719–729.3. Karnak I, Senocak ME, Ciftci AO, et al. Inflammatory myofibroblastic tumor in children: diagnosis and treatment. J Pediatr Surg. 2001; 36:908–912.4. Fletcher C, Senocak J, Fletcher C. Inflammatory myofibroblastic tumour: World Health Organization classification of tumours. IARC Press;Lyon, France: 2002.5. Coffin CM, Watterson J, Priest JR, et al. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995; 19:859–872.6. Höhne S, Milzsch M, Adams J, et al. Inflammatory pseudotumor (IPT) and inflammatory myofibroblastic tumor (IMT): a representative literature review occasioned by a rare IMT of the transverse colon in a 9-year-old child. Tumori. 2015; 101:249–256.7. Kovach SJ, Fischer AC, Katzman PJ, et al. Inflammatory myofibroblastic tumors. J Surg Oncol. 2006; 94:385–391.8. Kim EY, Lee IK, Lee YS, et al. Inflammatory myofibroblastic tumor in colon. J Korean Surg Soc. 2012; 82:45–49.9. Patnana M, Sevrukov AB, Elsayes KM, et al. Inflammatory pseudotumor: the great mimicker. AJR Am J Roentgenol. 2012; 198:W217–W227.10. Karaisli S, Kamer E, Ekinci N, et al. Inflammatory myofibroblastic tumour of the colon: 2 case reports and a comprehensive review of the literature. Int J Colorectal Dis. 2020; 35:947–958.11. Jeong JH, Cho IH, Kong EJ, et al. (18)F-FDG PET/CT in inflammatory pseudotumor of the colon causing intussusception. Ann Nucl Med. 2011; 25:447–450.12. Rosenbaum A, Arnold JC, Rebel M, et al. Pseudotumor of the sigmoid mimicking carcinoma. Endoscopy. 2000; 32:546–548.13. Nakamura Y, Kayano H, Shimada T, et al. Plasma cell granuloma of the sigmoid colon associated with diverticular disease and accompanying IgM-type monoclonal gammopathy. Intern Med. 2010; 49:227–230.14. Tanaka A, Hirabayashi K, Sadahiro S, et al. Inflammatory myofibroblastic tumor of the ascending colon in adults manifested by positive fecal occult blood test. Gastrointest Endosc. 2010; 71:214–216.15. Salameh M, Sultan I, Barbar M, et al. Inflammatory myofibroblastic tumor causing unexplained anemia in a toddler: a case report. J Med Case Rep. 2011; 5:69.16. Satahoo SS, Brathwaite C, Davis JS, et al. Obstructing apple core lesion of the rectum: a case report of inflammatory pseudotumor masquerading as colorectal carcinoma. J Pediatr Surg. 2013; 48:677–680.17. Walia R, Gjikopulli A, Williams H, et al. Polypoid mass in the ascending colon with intussusception: a rare presentation of an inflammatory myofibroblastic tumor. J Pediatr Gastroenterol Nutr. 2014; 58:e35.18. Przkora R, Bolder U, Schwarz S, et al. Regression of nonresectable inflammatory myofibroblastic tumours after treatment with nonsteroidal anti-inflammatory drugs. Eur J Clin Invest. 2004; 34:320–321.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long, Pedunculated, Large Hyperplastic Polyp of the Terminal Ileum Protruding Through the Ileocecal Valve: A Case Report
- A Case of Pseudosarcomatous Change of an Inflammatory Colon Polyp Associated with Tuberculous Colitis
- A Case of Pedunculated Malignant Melanoma
- Inflammatory Pseud0tumor of the Liver: A case report
- Inflammatory Pseudotumor in the Liver and Right Omentum Caused by Pelvic Inflammatory Disease: A Case Report