J Korean Neurosurg Soc.
2023 Jan;66(1):24-32. 10.3340/jkns.2022.0085.
Role of Neurosurgeons in the Treatment of Acute Ischemic Stroke in the Emergency Room
- Affiliations
-
- 1Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 2Department of Radiology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 3Department of Neurology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 4Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 5Department of Neurosurgery, Dongnam Institute of Radiological & Medical Sciences, Busan, Korea
- KMID: 2537845
- DOI: http://doi.org/10.3340/jkns.2022.0085
Abstract
Objective
: With the recent increase in mechanical thrombectomy (MT) for acute ischemic stroke (AIS), the role of neurosurgeons in AIS treatment has become increasingly important. This study aimed to assess the outcomes of patients with AIS treated by neurosurgeons and neurologists in the emergency room (ER) of a tertiary hospital in South Korea.
Methods
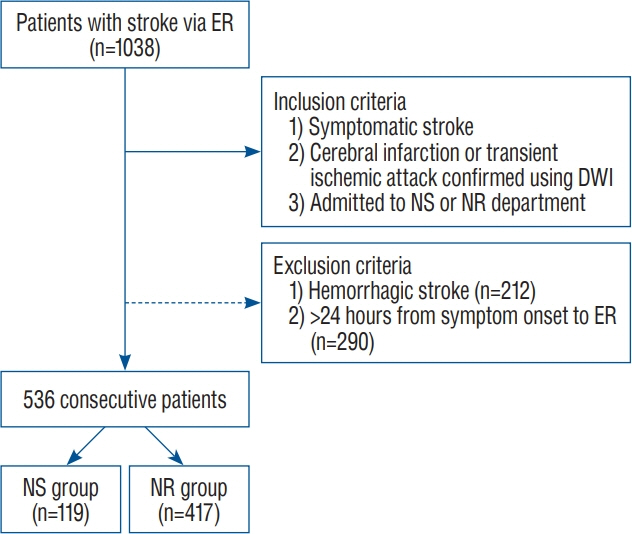
: From January 2020 to June 2021, 536 patients with AIS within 24 hours of symptom onset were admitted to our hospital via the ER. Based on the type of doctors who provided initial care for AIS in the ER, patients were divided into two groups : (a) neurosurgeon group (n=119, 22.2%) and (b) neurologist group (n=417, 77.8%).
Results
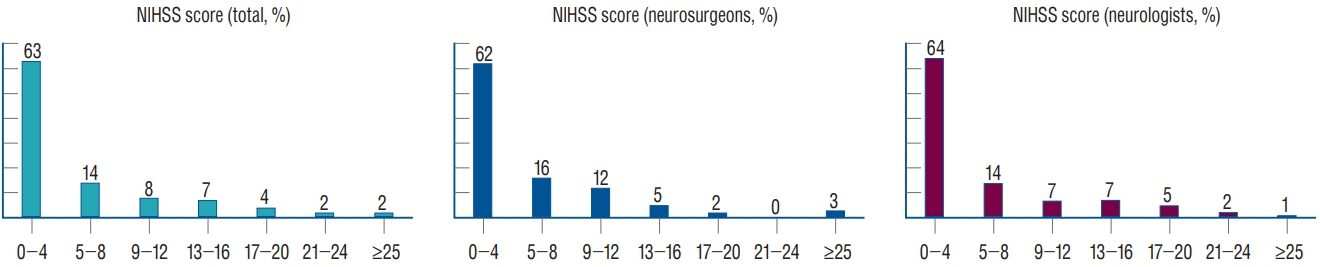
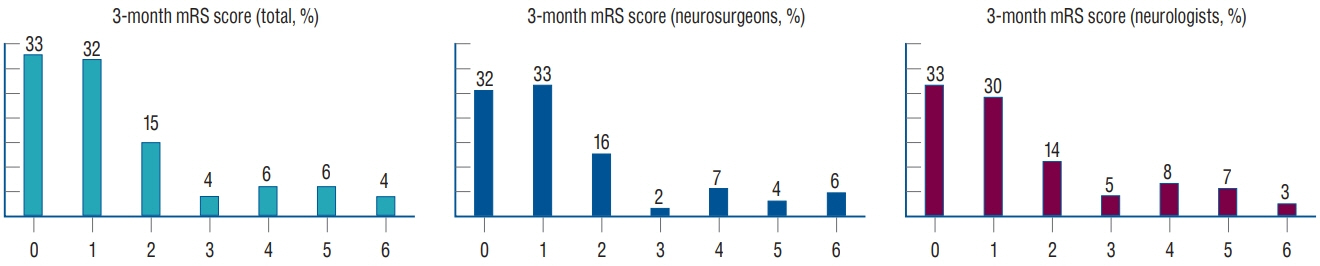
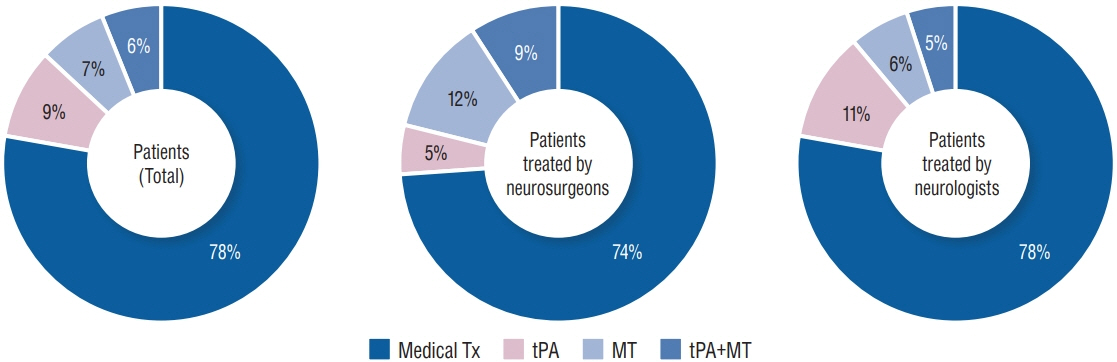
: Intravenous tissue plasminogen activator (tPA) was administered in 82 (15.3%) of 536 patients (n=17 [14.3%] in the neurosurgeon group and n=65 [15.6%] in the neurologist group). The door-to-tPA time was not significantly different between both groups (median, 53 minutes; interquartile range [IQR], 45–58 vs. median, 54 minutes; IQR, 46–74; p=0.372). MT was performed in 69 patients (12.9%) (n=25, 36.2% in the neurosurgeon group and n=44, 63.8% in the neurologist group). The neurosurgeon group achieved a shorter door-to-puncture time than the neurologist group (median, 115 minutes; IQR, 107–151 vs. median, 162 minutes; IQR, 117–189; p=0.049). Good clinical outcomes (3-month modified Rankin Scale 0–2) did not differ significantly between the two groups (96/119 [80.7%] vs. 322/417 [77.2%], p=0.454).
Conclusion
: The neurosurgeon group showed similar door-to-treatment time and clinical outcomes to the neurologist group in patients with AIS in the ER. This study suggests that neurosurgeons have comparable abilities to care for patients with AIS in the ER.
Keyword
Figure
Reference
-
References
1. Atallah E, Bekelis K, Saad H, Chalouhi N, Dang S, Li J, et al. A comparison of two stroke cohorts cared for by two different specialties in a practice-based tele-stroke population. Clin Neurol Neurosurg. 168:67–71. 2018.2. Candelise L, Gattinoni M, Bersano A, Micieli G, Sterzi R, Morabito A, et al. Stroke-unit care for acute stroke patients: an observational followup study. Lancet. 369:299–305. 2007.3. Costalat V, Lobotesis K, Machi P, Mourand I, Maldonado I, Heroum C, et al. Prognostic factors related to clinical outcome following thrombectomy in ischemic stroke (RECOST study). 50 patients prospective study. Eur J Radiol. 81:4075–4082. 2012.4. Hand PJ, Kwan J, Lindley RI, Dennis MS, Wardlaw JM. Distinguishing between stroke and mimic at the bedside: the brain attack study. Stroke. 37:769–775. 2006.5. Kicielinski KP, Ogilvy CS. Role of the neurosurgeon in acute ischemic stroke treatment from triage to intensive care unit. Neurosurgery. 85:S47–S51. 2019.6. Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the epidemiology research council of the Korean Stroke Society. J Stroke. 21:42–59. 2019.7. Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013-2014: national averages and disparities. J Korean Med Sci. 35:e167. 2020.8. Kim SH, Nam TM, Jang JH, Kim YZ, Kim KH, Kim DH, et al. Improving door-to-puncture time in mechanical thrombectomy with direct care from a neurointerventionalist in the emergency department. World Neurosurg. 152:e455–e461. 2021.9. Lee HJ, Shin DH, Yang KI, Koh IS, Lee KB, Lee WW, et al. The investigation on the burden of neurology residents to manage the patient who received thrombolytic treatment in the emergency department with hyperacute stroke. J Korean Neurol Assoc. 39:305–311. 2021.10. Lee KB, Park HK, Park TH, Lee SJ, Bae HJ, Lee KS, et al. Policy making committee, the Korean Stroke Society. Current status and problems of stroke units in Korea: results of a nationwide acute care hospital survey by the Korean Stroke Society. J Korean Neurol Assoc. 33:141–155. 2015.11. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea : part II. Cerebral infarction, cerebral arterial stenosis, and moyamoya disease. J Korean Neurosurg Soc. 63:69–79. 2020.12. Muñoz Venturelli P, Robinson T, Lavados PM, Olavarría VV, Arima H, Billot L, et al. Regional variation in acute stroke care organisation. J Neurol Sci. 371:126–130. 2016.13. Park H, Kim BM, Baek JH, Kim JH, Heo JH, Kim DJ, et al. Predictors of good outcomes in patients with failed endovascular thrombectomy. Korean J Radiol. 21:582–587. 2020.14. Reeves M, Khoury J, Alwell K, Moomaw C, Flaherty M, Woo D, et al. Distribution of national institutes of health stroke scale in the Cincinnati/ Northern Kentucky stroke study. Stroke. 44:3211–3213. 2013.15. Rizos T, Ringleb PA, Huttner HB, Kohrmann M, Juttler E. Evolution of stroke diagnosis in the emergency room--a prospective observational study. Cerebrovasc Dis. 28:448–453. 2009.16. Rudd AG, Hoffman A, Irwin P, Lowe D, Pearson MG. Stroke unit care and outcome: results from the 2001 National Sentinel Audit of Stroke (England, Wales, and Northern Ireland). Stroke. 36:103–106. 2005.17. Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013:CD000197. 2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Future Role of Neurosurgeons: Toward Convergence Neurosurgeon Beyond Hybrid Neurosurgeon
- A Case of Hemoperitoneum after Intraarterial Urokinase Infusion for Acute Ischemic Stroke
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Characteristics of the Early Electrocardiographic Findings and Their Relations h i p with the Location of the Lesion and Its Severity in Acute Ischemic Stroke