J Korean Acad Oral Health.
2022 Dec;46(4):252-259. 10.11149/jkaoh.2022.46.4.252.
A suggestion of the new oral health care system for the caregivers at the long-term care facilities
- Affiliations
-
- 1Department of Preventive and Public Health Dentistry, School of Dentistry, Seoul National University, Seoul, Korea
- 2Dental Research Institute, Seoul National University, Seoul, Korea
- KMID: 2537823
- DOI: http://doi.org/10.11149/jkaoh.2022.46.4.252
Abstract
Objectives
This study aims to suggest ways to improve the oral care competencies of caregivers by strengthening oral care services for the elderly with mobility difficulties in long-term care facilities.
Methods
Through a web survey, 215 caregivers were invited, their actual situation was identified, and necessary educational tasks were listed. We developed 16 types of card news, two types of songs, and four types of video clips that can be used in the field for the listed educational topics. Several meetings with expert developers resulted in developing the components and design of an oral health management platform for caregivers in long-term care facilities.
Results
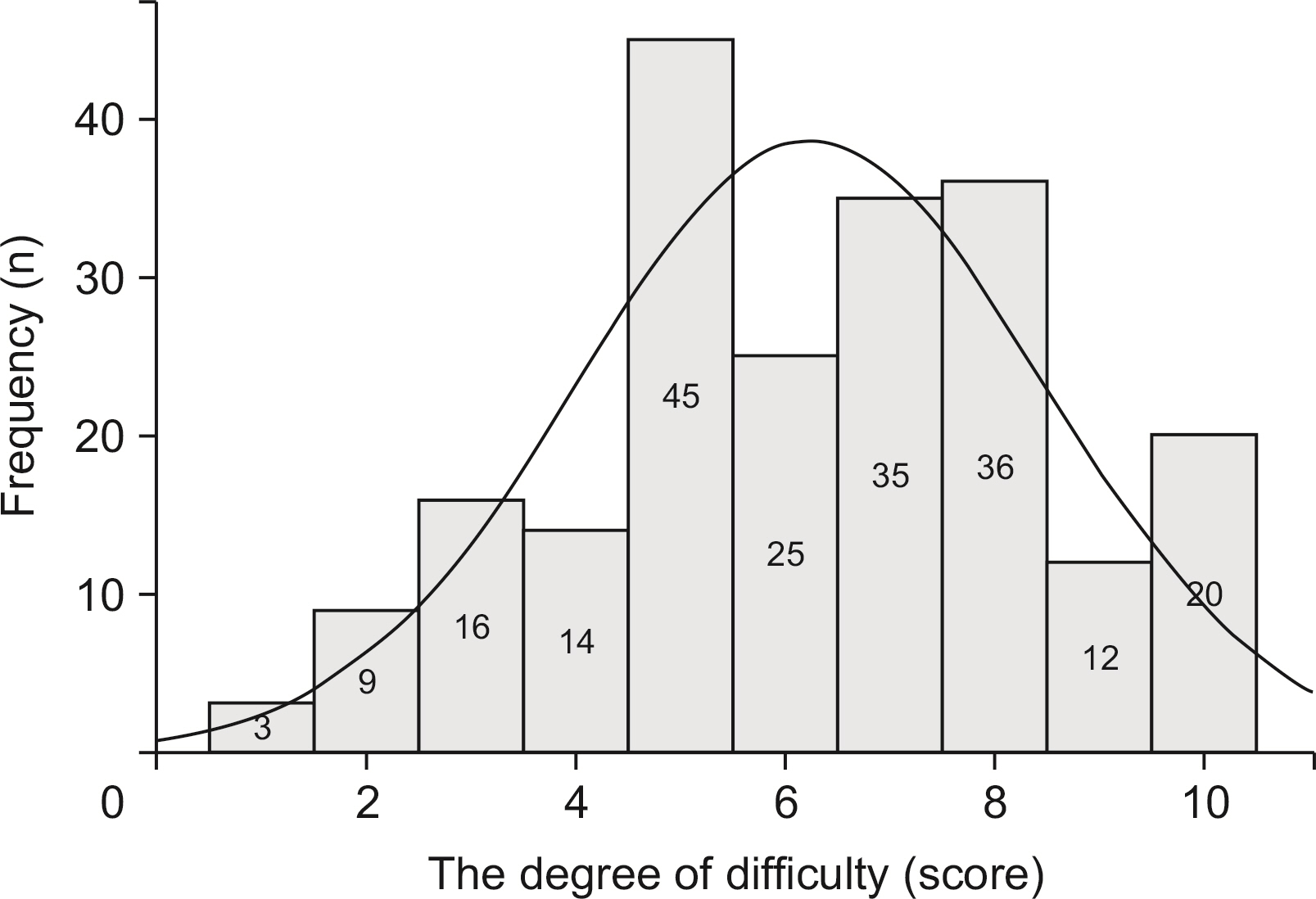
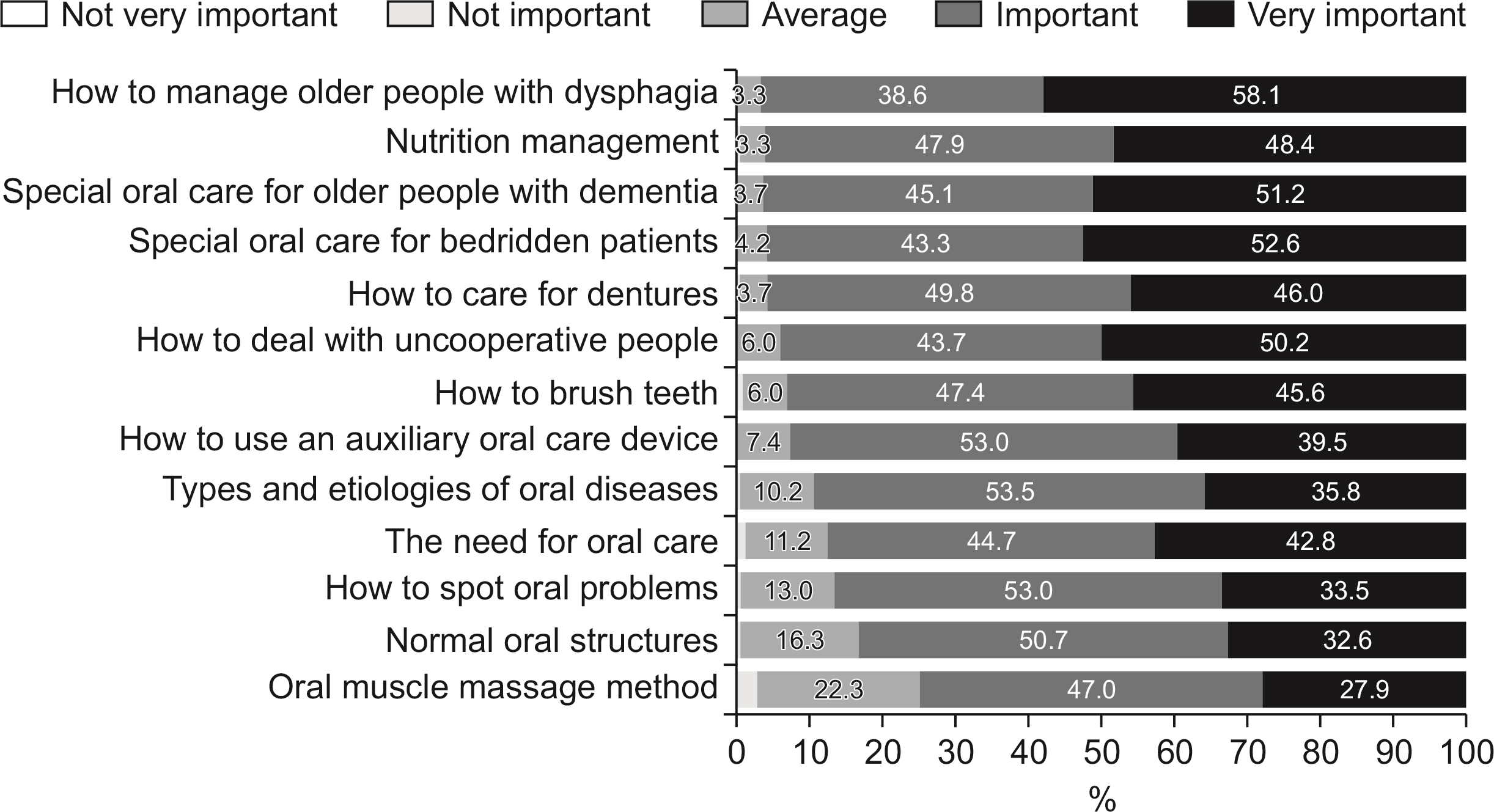
As a result of the web survey, many caregivers in long-term care facilities needed education or information on oral care methods, and many people felt difficulties in oral care for the elderly. About 40% of the caregivers had no experience in oral health education, and many learned how to care through unsystematic apprenticeships. Most of the education content that caregivers prioritized were brushing teeth and denture management, but there were also needs such as management of dementia and bedridden patients, non-cooperative oral care, nutrition management, and oral auxiliary products use.
Conclusions
In conclusion, this study reviewed and suggested digital platforms such as strengthening caregivers’ competency in long-term care facilities, providing customized educational information, discovering oral problems of the elderly, and reporting oral difficulties to experts.
Keyword
Figure
Reference
-
References
1. Statistics Korea. Press release. Social statistics. Population ageing. 2022 Statistics on the aged. [internet]. Available from:http://www.kostat.go.kr. cited 2022 Dec 12.2. Lee HS, Kwon SH. 2020; Problems and suggestions of welfare system for the elderly in super-aged society. J Labor Law. 50:1–29.3. Statistics Korea. 2021. 2020 National Health Insurance Statistical Yearbook. Health Insurance Review and Assessment Service, National Health Insurance Service;Wonju: 3. Available from:http://www.kostat.go.kr. cited 2022 Dec 12.4. Health Insurance Review and Assessment Service, National Health Insurance Service. 2020 National Health Insurance Statistical Yearbook. Health Insurance Review and Assessment Service, National Health Insurance Service;Wonju:5. Health Insurance Review and Assessment Service, National Health Insurance Service. 2020 National Health Insurance Statistical Yearbook. Health Insurance Review and Assessment Service, National Health Insurance Service;Wonju:6. Lee HJ. 2020; Comparison of oral health status of the elderly living in long-term care facilities and non-resident elderly. J Converg Inform Technol. 10:134–140.7. Han DH, Kim NH, Ko SM, Kwak JM, So JS, Lee SK, et al. 2015; Oral health status of institutionalized elderly in Korea. J Korean Dent Assoc. 53:688–695.8. MacEntee MI. 2000; Oral care for successful aging in long-term care. J Public Health Dent. 60:326–29. DOI: 10.1111/j.1752-7325.2000.tb03343.x. PMID: 11243055.9. de Visschere LMJ, van der Putten GJ, Vanobbergen JNO, Schols JMGA, de Baat C. 2011; An oral health care guideline for institutionalised older people. Gerodontology. 28:307–310. DOI: 10.1111/j.1741-2358.2010.00406.x. PMID: 22092286.10. Komulainen K, Ylöstalo P, Syrjälä AM, Ruoppi P, Knuuttila M, Sulkava R, et al. 2014; Determinants for preventive oral health care need among community-dwelling older people: a population-based study. Spec Care Dentist. 34:19–26. DOI: 10.1111/scd.12021. PMID: 24382367.11. Tsukada S, Shibata S, Kajii Y, Stegaroiu R, Ohuchi A. 2012; Investigation of screening sheet for multiple-professional use to judge necessity for dental intervention in patients: considerations based on comparison of screening results by dentist and dental hygienist. J Jpn Soc Dent Hyg. 7:43–54.12. Tsukada S, Ito K, Stegaroiu R, Shibata S, Ohuchi A. 2017; An oral health and function screening tool for nursing personnel of long-term care facilities to identify the need for dentist referral without preliminary training. Gerodontology. 34:232–239. DOI: 10.1111/ger.12255. PMID: 28066920.13. Jin BH, Paik HR, Park JA, Lee JY, Lee GR, Han S. 2020. Oral health survey of the elderly and development of oral health status evaluation tools. SNU R&DB Foundation;Seoul: p. 69–73.14. Jeon HS, Han SY, Chung WG, Choi JH. 2015; Knowledge, attitude, and behavior status on oral health care of geriatric care workers in long-term care facilities. J Dent Hyg Sci. 15:569–576. DOI: 10.17135/jdhs.2015.15.5.569.15. Kim SH, Kim CH, Son GY, Yang SY, Cho MS, Oh SH. 2015; The perception of elderly oral health care in the care workers in nursing homes. J Korean Soc Dent Hyg. 14:715–721. DOI: 10.13065/jksdh.2014.14.05.715.16. Park MS. 2010; Educational needs in the provision of oral care by nursing staff in long-term care facility for elderly people. J Korean Gerontol Nurs. 12:72–80.17. Kim HK, Kim KM, Kim SI, Kim EJ, Namkoong EJ, Bae SM, et al. 2019; Oral health care status and educational needs of care workers. J Korean Dent Hyg Sci. 2:41–51.18. Ministry of Health and Welfare. 2020. 2019 Caregiver Training Standard Textbook. Ministry of Health and Welfare;Sejong: p. 254–258.19. Kim SU, Cho YJ, Kim JH. 2017; UX design of next generation web platform. Proc Korean Soc Comp Inf Conf. 25:251–254.20. Paterson DH, Warburton DER. 2010; Physical activity and functional limitations in older adults: a systematic review related to Canada's Physical Activity Guidelines. Int J Behav Nutr Phys Act. 7:38. DOI: 10.1186/1479-5868-7-38. PMID: 20459782. PMCID: PMC2882898.21. Kozakai R, von Bonsdorff M, Sipilä S, Rantanen T. 2013; Mobility limitation as a predictor of inpatient care in the last year of life among community-living older people. Aging Clin Exp Res. 25:81–87. DOI: 10.1007/s40520-013-0013-1. PMID: 23740637.22. Mahmoudi R, Novella JL, Manckoundia P, Ahssaini F, Lange PO, Blanchard F, et al. 2017; Is functional mobility an independent mortality risk factor in subjects with dementia? Maturitas. 103:65–70. DOI: 10.1016/j.maturitas.2017.06.031. PMID: 28778335.23. Kotronia E, Wannamethee SG, Papacosta AO, Whincup PH, Lennon LT, Visser M, et al. 2019; Oral health, disability and physical function: results from studies of older people in the United Kingdom and United States of America. J Am Med Dir Assoc. 20:1654. DOI: 10.1016/j.jamda.2019.06.010. PMID: 31409558. PMCID: PMC7477793.24. Kohli R, Nelson S, Ulrich S, Finch T, Hall K, Schwarz E. 2017; Dental care practices and oral health training for professional caregivers in long-term care facilities: an interdisciplinary approach to address oral health disparities. Geriatr Nurs. 38:296–301. DOI: 10.1016/j.gerinurse.2016.11.008. PMID: 28063685.25. Koistinen S, Ståhlnacke K, Olai L, Ehrenberg A, Carlsson E. 2021; Older people's experiences of oral health and assisted daily oral care in short-term facilities. BMC Geriatr. 21:388. DOI: 10.1186/s12877-021-02281-z. PMID: 34176481. PMCID: PMC8237451.26. Wu YP, Linder LA, Kanokvimankul P, Fowler B, Parsons BG, Macpherson CF, et al. 2018; Use of a smartphone application for prompting oral medication adherence among adolescents and young adults with cancer. Oncol Nurs Forum. 45:69–76. DOI: 10.1188/18.ONF.69-76. PMID: 29251285. PMCID: PMC5927589.27. Atkinson TM, Rodriguez VM, Gordon M, Avildsen IK, Emanu JC, Jewell ST, et al. 2016; The association between patient-reported and objective oral anticancer medication adherence measures: a systematic review. Oncol Nurs Forum. 43:576–582. DOI: 10.1188/16.ONF.576-582. PMID: 27541550. PMCID: PMC5008846.28. Macpherson CF, Linder LA, Ameringer S, Erickson J, Stegenga K, Woods NF. 2014; Feasibility and acceptability of an iPad application to explore symptom clusters in adolescents and young adults with cancer. Pediatr Blood Cancer. 61:1996–2003. DOI: 10.1002/pbc.25152. PMID: 25066927.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Exploration of the experience of caregivers for oral health care for the elderly in long-term care facilities: based on the grounded theory
- Long-Term Care System in Korea
- Long-Term Care Facility Caregivers’ Need to Reduce Physical Burdens
- Perceptions of Facility Workers and Family Caregivers toward CCTV in Long-Term Care Facilities
- Differences in Family Caregivers' Opinions about Out-of-Pocket Payment for Long-Term Care Facilities by Income Levels