Korean J Pain.
2023 Jan;36(1):137-146. 10.3344/kjp.22327.
An investigation of the relationship between cutaneous allodynia and kinesiophobia, gastrointestinal system symptom severity, physical activity and disability in individuals with migraine
- Affiliations
-
- 1Physiotherapy and Rehabilitation Doctoral Program, Instute of Health Sciences, Ankara Yildirim Beyazit University, Ankara, Turkey
- 2Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, Ankara Yildirim Beyazit University, Ankara, Turkey
- KMID: 2537620
- DOI: http://doi.org/10.3344/kjp.22327
Abstract
- Background
To investigate the relationship between cutaneous allodynia (CA) and kinesiophobia, gastrointestinal system (GIS) symptom severity, physical activity, and disability, and to determine whether CA, pain, and disability were influencing factors for kinesiophobia, GIS symptoms, and physical activity in individuals with migraine.
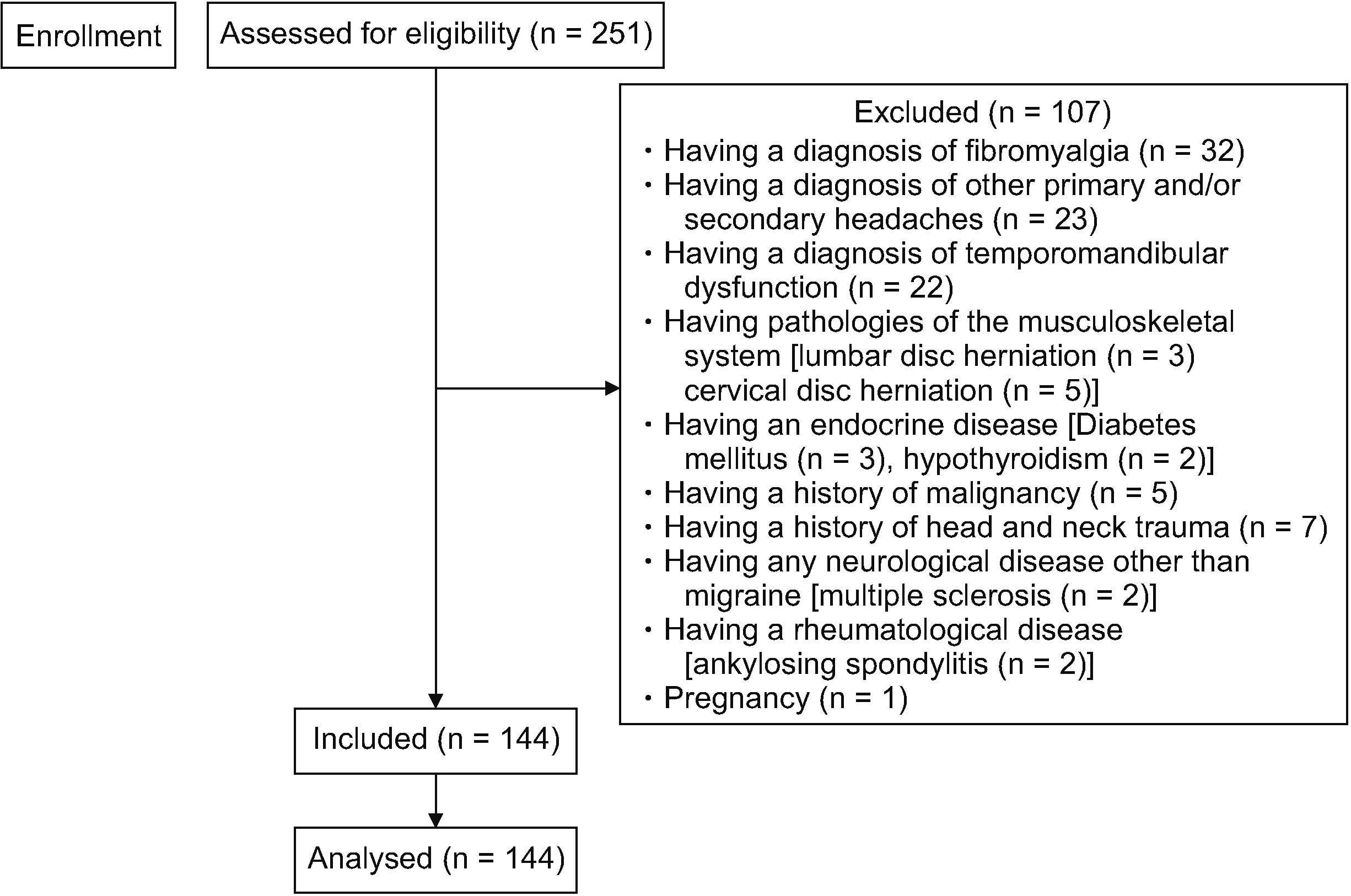
Methods
The study included 144 individuals with migraine. CA, kinesiophobia, GIS symptoms, physical activity level, and migraine-related disability were evaluated with the Allodynia Symptom Checklist, the Tampa Kinesiophobia Scale (TKS), the Gastrointestinal Symptom Rating Scale (GSRS), the International Physical Activity Questionnaire-7, and the Migraine Disability Assessment Scale (MIDAS), respectively.
Results
The CA severity was only associated with TKS (r = 0.515; P < 0.001), GSRS-total (r = 0.336; P < 0.001), GSRS-abdominal pain (r = 0.323; P < 0.001), GSRS-indigestion (r = 0.257; P = 0.002), GSRS-constipation (r = 0.371; P < 0.001), and MIDAS scores (r = 0.178; P = 0.033). Attack frequency (P = 0.015), attack duration (P = 0.035) and presence of CA (P < 0.001) were risk factors for kinesiophobia. Attack frequency (P = 0.027) and presence of CA (P = 0.004) were risk factors for GIS symptoms.
Conclusions
There was a relationship between the CA and kinesiophobia, GIS symptoms, and disability. CA and attack frequency were found to be risk factors for kinesiophobia and GIS symptoms. Migraine patients with CA should be assessed in terms of kinesiophobia, GIS, and disability. Lifestyle changes such as exercise and dietary changes and/or pharmacological treatment options for CA may increase success in migraine management.
Keyword
Figure
Reference
-
1. Headache Classification Committee of the International Headache Society (IHS). 2018; the international classification of headache disorders, 3rd edition. Cephalalgia. 38:1–211. DOI: 10.1177/0333102417738202. PMID: 29368949.2. Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton RB, Scher AI, et al. 2007; The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 27:193–210. DOI: 10.1111/j.1468-2982.2007.01288.x. PMID: 17381554.3. Chen PK, Wang SJ. 2018; Non-headache symptoms in migraine patients. F1000Res. 7:188. DOI: 10.12688/f1000research.12447.1. PMID: 29511532. PMCID: PMC5814742.4. Bigal ME, Ashina S, Burstein R, Reed ML, Buse D, Serrano D, et al. 2008; Prevalence and characteristics of allodynia in headache sufferers: a population study. Neurology. 70:1525–33. DOI: 10.1212/01.wnl.0000310645.31020.b1. PMID: 18427069. PMCID: PMC2664547.5. Burstein R, Yarnitsky D, Goor-Aryeh I, Ransil BJ, Bajwa ZH. 2000; An association between migraine and cutaneous allodynia. Ann Neurol. 47:614–24. DOI: 10.1002/1531-8249(200005)47:5<614::AID-ANA9>3.0.CO;2-N. PMID: 10805332.6. Çelenay ŞT, Mete O, Çoban Ö, Karahan N. 2020; A comparison of pain severity, sleep quality, and psychological status between migraine patients with and without cutaneous allodynia. Anatol Clin. 25:102–7. Turkish. DOI: 10.1002/1531-8249(200005)47:5<614::aid-ana9>3.0.co;2-n.7. Lipton RB, Bigal ME, Ashina S, Burstein R, Silberstein S, Reed ML, et al. 2008; Cutaneous allodynia in the migraine population. Ann Neurol. 63:148–58. DOI: 10.1002/ana.21211. PMID: 18059010. PMCID: PMC2729495.8. Kori SH, Miller RP, Todd DD. 1990; Kinisiophobia: a new view of chronic pain behavior. Pain Manage. 3:35–43.9. McLean SA, Clauw DJ, Abelson JL, Liberzon I. 2005; The development of persistent pain and psychological morbidity after motor vehicle collision: integrating the potential role of stress response systems into a biopsychosocial model. Psychosom Med. 67:783–90. DOI: 10.1097/01.psy.0000181276.49204.bb. PMID: 16204439.10. Benatto MT, Bevilaqua-Grossi D, Carvalho GF, Bragatto MM, Pinheiro CF, Straceri Lodovichi S, et al. 2019; Kinesiophobia is associated with migraine. Pain Med. 20:846–51. DOI: 10.1093/pm/pny206. PMID: 30462312.11. Chen X, D'Souza R, Hong ST. 2013; The role of gut microbiota in the gut-brain axis: current challenges and perspectives. Protein Cell. 4:403–14. DOI: 10.1007/s13238-013-3017-x. PMID: 23686721. PMCID: PMC4875553.12. Finkel AG, Yerry JA, Mann JD. 2013; Dietary considerations in migraine management: does a consistent diet improve migraine? Curr Pain Headache Rep. 17:373. DOI: 10.1007/s11916-013-0373-4. PMID: 24068338.13. Martami F, Ghorbani Z, Abolhasani M, Togha M, Meysamie A, Sharifi A, et al. 2018; Comorbidity of gastrointestinal disorders, migraine, and tension-type headache: a cross-sectional study in Iran. Neurol Sci. 39:63–70. DOI: 10.1007/s10072-017-3141-0. PMID: 29022143.14. Lankarani KB, Akbari M, Tabrizi R. 2017; Association of gastrointestinal functional disorders and migraine headache: a population base study. Middle East J Dig Dis. 9:139–45. DOI: 10.15171/mejdd.2017.64. PMID: 28894515. PMCID: PMC5585926.15. Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, et al. 2009; Allodynia in migraine: association with comorbid pain conditions. Headache. 49:1333–44. DOI: 10.1111/j.1526-4610.2009.01521.x. PMID: 19788473.16. Caspersen CJ, Powell KE, Christenson GM. 1985; Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 100:126–31. PMID: 3920711. PMCID: PMC1424733.17. Wöber C, Brannath W, Schmidt K, Kapitan M, Rudel E, Wessely P, et al. 2007; Prospective analysis of factors related to migraine attacks: the PAMINA study. Cephalalgia. 27:304–14. DOI: 10.1111/j.1468-2982.2007.01279.x. PMID: 17376107.18. Varkey E, Sveälv BG, Edin F, Ravn-Fischer A, Cider Å. 2017; Provocation of migraine after maximal exercise: a test-retest study. Eur Neurol. 78:22–7. DOI: 10.1159/000477166. PMID: 28564648.19. Martins IP, Gouveia RG, Parreira E. 2006; Kinesiophobia in migraine. J Pain. 7:445–51. DOI: 10.1016/j.jpain.2006.01.449. PMID: 16750801.20. Koppen H, van Veldhoven PL. 2013; Migraineurs with exercise-triggered attacks have a distinct migraine. J Headache Pain. 14:99. DOI: 10.1186/1129-2377-14-99. PMID: 24359317. PMCID: PMC3880028.21. Nijs J, Leysen L, Vanlauwe J, Logghe T, Ickmans K, Polli A, et al. 2019; Treatment of central sensitization in patients with chronic pain: time for change? Expert Opin Pharmacother. 20:1961–70. DOI: 10.1080/14656566.2019.1647166. PMID: 31355689.22. Renjith V, Pai MS, Castelino F, Pai A, George A. 2016; Clinical profile and functional disability of patients with migraine. J Neurosci Rural Pract. 7:250–6. DOI: 10.4103/0976-3147.176188. PMID: 27114657. PMCID: PMC4821934.23. Louter MA, Bosker JE, van Oosterhout WP, van Zwet EW, Zitman FG, Ferrari MD, et al. 2013; Cutaneous allodynia as a predictor of migraine chronification. Brain. 136(Pt 11):3489–96. DOI: 10.1093/brain/awt251. PMID: 24080152.24. Kwong WJ, Pathak DS. 2007; Validation of the eleven-point pain scale in the measurement of migraine headache pain. Cephalalgia. 27:336–42. DOI: 10.1111/j.1468-2982.2007.01283.x. PMID: 17376110.25. Yalin OÖ, Uludüz D, Sungur MA, Sart H, Özge A. 2017; Identification of allodynic migraine patients with the Turkish version of the allodynia symptom checklist: reliability and consistency study. Noro Psikiyatr Ars. 54:260–6. DOI: 10.5152/npa.2016.15953. PMID: 29033640. PMCID: PMC5630106.26. Yilmaz ÖT, Yakut Y, Uygur F, Uluğ N. 2011; Turkish version of the Tampa Scale for Kinesiophobia and its test-retest reliability. Fizyoter Rehabil. 22:44–9. Turkish. DOI: 10.1111/j.1468-2982.2007.01283.x.27. Bränström H, Fahlström M. 2008; Kinesiophobia in patients with chronic musculoskeletal pain: differences between men and women. J Rehabil Med. 40:375–80. DOI: 10.2340/16501977-0186. PMID: 18461263.28. Turan N, Aştı TA, Kaya N. 2017; Reliability and validity of the Turkish version of the Gastrointestinal Symptom Rating Scale. Gastroenterol Nurs. 40:47–55. DOI: 10.1097/SGA.0000000000000177. PMID: 28134719.29. Saglam M, Arikan H, Savci S, Inal-Ince D, Bosnak-Guclu M, Karabulut E, et al. 2010; International physical activity questionnaire: reliability and validity of the Turkish version. Percept Mot Skills. 111:278–84. DOI: 10.2466/06.08.PMS.111.4.278-284. PMID: 21058606.30. Ertaş M, Siva A, Dalkara T, Uzuner N, Dora B, Inan L, et al. 2004; Validity and reliability of the Turkish Migraine Disability Assessment (MIDAS) questionnaire. Headache. 44:786–93. DOI: 10.1111/j.1526-4610.2004.04146.x. PMID: 15330825.31. Turk DC, Wilson HD. 2010; Fear of pain as a prognostic factor in chronic pain: conceptual models, assessment, and treatment implications. Curr Pain Headache Rep. 14:88–95. DOI: 10.1007/s11916-010-0094-x. PMID: 20425197. PMCID: PMC2872063.32. Crombez G, Vlaeyen JW, Heuts PH, Lysens R. 1999; Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 80:329–39. DOI: 10.1016/S0304-3959(98)00229-2. PMID: 10204746.33. Cai L, Liu Y, Xu H, Xu Q, Wang Y, Lyu P. 2018; Incidence and risk factors of kinesiophobia after total knee arthroplasty in Zhengzhou, China: a cross-sectional study. J Arthroplasty. 33:2858–62. DOI: 10.1016/j.arth.2018.04.028. PMID: 29776855.34. Bilgin S, Cetin H, Karakaya J, Kose N. 2019; Multivariate analysis of risk factors predisposing to kinesiophobia in persons with chronic low back and neck pain. J Manipulative Physiol Ther. 42:565–71. DOI: 10.1016/j.jmpt.2019.02.009. PMID: 31771838.35. Aamodt AH, Stovner LJ, Hagen K, Zwart JA. 2008; Comorbidity of headache and gastrointestinal complaints. The Head-HUNT Study. Cephalalgia. 28:144–51. DOI: 10.1111/j.1468-2982.2007.01486.x. PMID: 18197884.36. Midenfjord I, Grinsvall C, Koj P, Carnerup I, Törnblom H, Simrén M. 2021; Central sensitization and severity of gastrointestinal symptoms in irritable bowel syndrome, chronic pain syndromes, and inflammatory bowel disease. Neurogastroenterol Motil. 33:e14156. DOI: 10.1111/nmo.14156. PMID: 33860970.37. Saberi HR, Moravveji AR. 2010; Gastrointestinal complaints in shift-working and day-working nurses in Iran. J Circadian Rhythms. 8:9. DOI: 10.1186/1740-3391-8-9. PMID: 20929565. PMCID: PMC2958856.38. Goyal O, Nohria S, Dhaliwal AS, Goyal P, Soni RK, Chhina RS, et al. 2021; Prevalence, overlap, and risk factors for Rome IV functional gastrointestinal disorders among college students in northern India. Indian J Gastroenterol. 40:144–53. DOI: 10.1007/s12664-020-01106-y. PMID: 33226570.39. Stronks DL, Tulen JH, Bussmann JB, Mulder LJ, Passchier J. 2004; Interictal daily functioning in migraine. Cephalalgia. 24:271–9. DOI: 10.1111/j.1468-2982.2004.00661.x. PMID: 15030535.40. Amin FM, Aristeidou S, Baraldi C, Czapinska-Ciepiela EK, Ariadni DD, Di Lenola D, et al. 2018; The association between migraine and physical exercise. J Headache Pain. 19:83. DOI: 10.1186/s10194-018-0902-y. PMID: 30203180. PMCID: PMC6134860.41. Seefeldt V, Malina RM, Clark MA. 2002; Factors affecting levels of physical activity in adults. Sports Med. 32:143–68. DOI: 10.2165/00007256-200232030-00001. PMID: 11839079.42. Burstein R, Jakubowski M, Rauch SD. 2011; The science of migraine. J Vestib Res. 21:305–14. DOI: 10.3233/VES-2012-0433. PMID: 22348935. PMCID: PMC3690498.43. Latremoliere A, Woolf CJ. 2009; Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 10:895–926. DOI: 10.1016/j.jpain.2009.06.012. PMID: 19712899. PMCID: PMC2750819.44. Polk AN, Protti TA, Smitherman TA. 2020; Allodynia and disability in migraine: the mediating role of stress. Headache. 60:2281–90. DOI: 10.1111/head.14012. PMID: 33169381.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Health-Related Quality of Life is Associated With Pain, Kinesiophobia, and Physical Activity in Individuals Who Underwent Cervical Spine Surgery
- Is there an Association between Migraine and Gastrointestinal Disorders?
- Cerebrovascular Function in Migraine Patients during, their Interictal Period, Compared to Normal Healthy Controls
- Sensitization of the Trigeminovascular Pathway: Perspective and Implications to Migraine Pathophysiology
- The association between pain, balance, fall, and disability in patients with lumbar spinal stenosis with vascular claudication