Korean J Transplant.
2022 Dec;36(4):294-297. 10.4285/kjt.22.0016.
The first successful report of liver transplantation from category III donation after circulatory death in South Korea: a case report
- Affiliations
-
- 1Department of Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 2Division of Acute Care Surgery, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 3Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2537542
- DOI: http://doi.org/10.4285/kjt.22.0016
Abstract
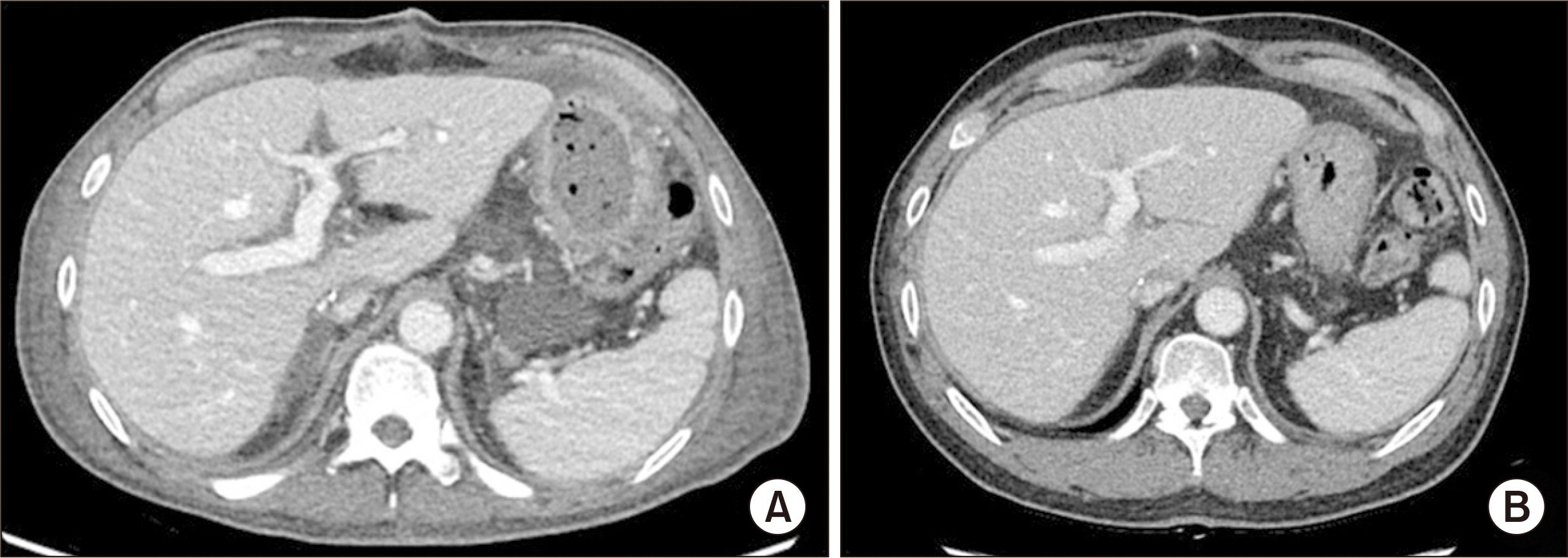
- Deceased donor liver transplantation (DDLT) using donations after brain death (DBDs) has been widely performed in Korea. However, to date, there is no report regarding donation after circulatory death (DCD) category III. A 56-year-old male patient diagnosed with hepatitis B virus-associated liver cirrhosis underwent DDLT using DCD category III. The recipient’s recovery was uneventful, and he was discharged on postoperative day 37. Currently, the patient is alive, with no complications 20 months after transplanta-tion. This case suggests that DCD with LT is both feasible and safe. Further studies are required to validate this finding.
Keyword
Figure
Reference
-
1. Bohorquez H, Seal JB, Cohen AJ, Kressel A, Bugeaud E, Bruce DS, et al. 2017; Safety and outcomes in 100 consecutive donation after circulatory death liver transplants using a protocol that includes thrombolytic therapy. Am J Transplant. 17:2155–64. DOI: 10.1111/ajt.14261. PMID: 28276658.2. Jeong E, Oh J, Lee Y, Lee J. 2020; The first donation after circulatory death following withdrawal of life-sustaining treatment in Korea. Korean J Transplant. 34(Suppl 1):S30. DOI: 10.4285/ATW2020.OR-1066.3. Kang I, Lee JG, Choi SH, Kim HJ, Han DH, Choi GH, et al. 2021; Impact of everolimus on survival after liver transplantation for hepatocellular carcinoma. Clin Mol Hepatol. 27:589–602. DOI: 10.3350/cmh.2021.0038. PMID: 34293849. PMCID: PMC8524068.4. Choi HJ. 2022; Current status and outcome of liver transplantation in South Korea. Clin Mol Hepatol. 28:117–9. DOI: 10.3350/cmh.2021.0381. PMID: 34875151. PMCID: PMC8755474.5. Goldaracena N, Cullen JM, Kim DS, Ekser B, Halazun KJ. Expanding the donor pool for liver transplantation with marginal donors. Int J Surg. 2020; 82 Suppl:30–5. DOI: 10.1016/j.ijsu.2020.05.024. PMID: 32422385.6. Renz JF, Yersiz H, Reichert PR, Hisatake GM, Farmer DG, Emond JC, et al. 2003; Split-liver transplantation: a review. Am J Transplant. 3:1323–35. DOI: 10.1046/j.1600-6135.2003.00254.x. PMID: 14525591.7. Marques HP, Barros I, Li J, Murad SD, di Benedetto F. Current update in domino liver transplantation. Int J Surg. 2020; 82S:163–8. DOI: 10.1016/j.ijsu.2020.03.017. PMID: 32244002.8. Kootstra G, Daemen JH, Oomen AP. 1995; Categories of non-heart-beating donors. Transplant Proc. 27:2893–4. PMID: 7482956.9. Thuong M, Ruiz A, Evrard P, Kuiper M, Boffa C, Akhtar MZ, et al. 2016; New classification of donation after circulatory death donors definitions and terminology. Transpl Int. 29:749–59. DOI: 10.1111/tri.12776. PMID: 26991858.10. Hashimoto K. 2020; Liver graft from donation after circulatory death donor: real practice to improve graft viability. Clin Mol Hepatol. 26:401–10. DOI: 10.3350/cmh.2020.0072. PMID: 32646199. PMCID: PMC7641554.11. Mathur AK, Heimbach J, Steffick DE, Sonnenday CJ, Goodrich NP, Merion RM. 2010; Donation after cardiac death liver transplantation: predictors of outcome. Am J Transplant. 10:2512–9. DOI: 10.1111/j.1600-6143.2010.03293.x. PMID: 20977642.12. Narvaez JR, Nie J, Noyes K, Kayler LK. 2020; Transplant outcomes of donation after circulatory death livers recovered with versus without premortem heparin administration. Liver Transpl. 26:247–55. DOI: 10.1002/lt.25685. PMID: 31755633.13. Schlegel A, Muller X, Kalisvaart M, Muellhaupt B, Perera MT, Isaac JR, et al. 2019; Outcomes of DCD liver transplantation using organs treated by hypothermic oxygenated perfusion before implantation. J Hepatol. 70:50–7. DOI: 10.1016/j.jhep.2018.10.005. PMID: 30342115.14. Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. 2006; Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 6:783–90. DOI: 10.1111/j.1600-6143.2006.01242.x. PMID: 16539636.15. Park H, Jung ES, Oh JS, Lee YM, Lee JM. 2021; Organ donation after controlled circulatory death (Maastricht classification III) following the withdrawal of life-sustaining treatment in Korea: a suggested guideline. Korean J Transplant. 35:71–6. DOI: 10.4285/kjt.21.0004. PMID: 35769520. PMCID: PMC9235338.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organ donation after controlled circulatory death (Maastricht classification III) following the withdrawal of life-sustaining treatment in Korea: a suggested guideline
- Donation after Circulatory Death in Lung Transplantation
- First Organ Donation after Circulatory Death Following Withdrawal of Life-sustaining Treatment in Korea: a Case Report
- The first donation after circulatory death following withdrawal of life-sustaining treatment in Korea
- Liver graft from donation after circulatory death donor: Real practice to improve graft viability