J Cerebrovasc Endovasc Neurosurg.
2022 Dec;24(4):372-379. 10.7461/jcen.2022.E2021.10.005.
Undeflatable balloon guide catheter (BGC) during endovascular procedure: Rescue strategy
- Affiliations
-
- 1Department of Neurosurgery, Cheju Halla General Hospital, Jeju, Korea
- KMID: 2537322
- DOI: http://doi.org/10.7461/jcen.2022.E2021.10.005
Abstract
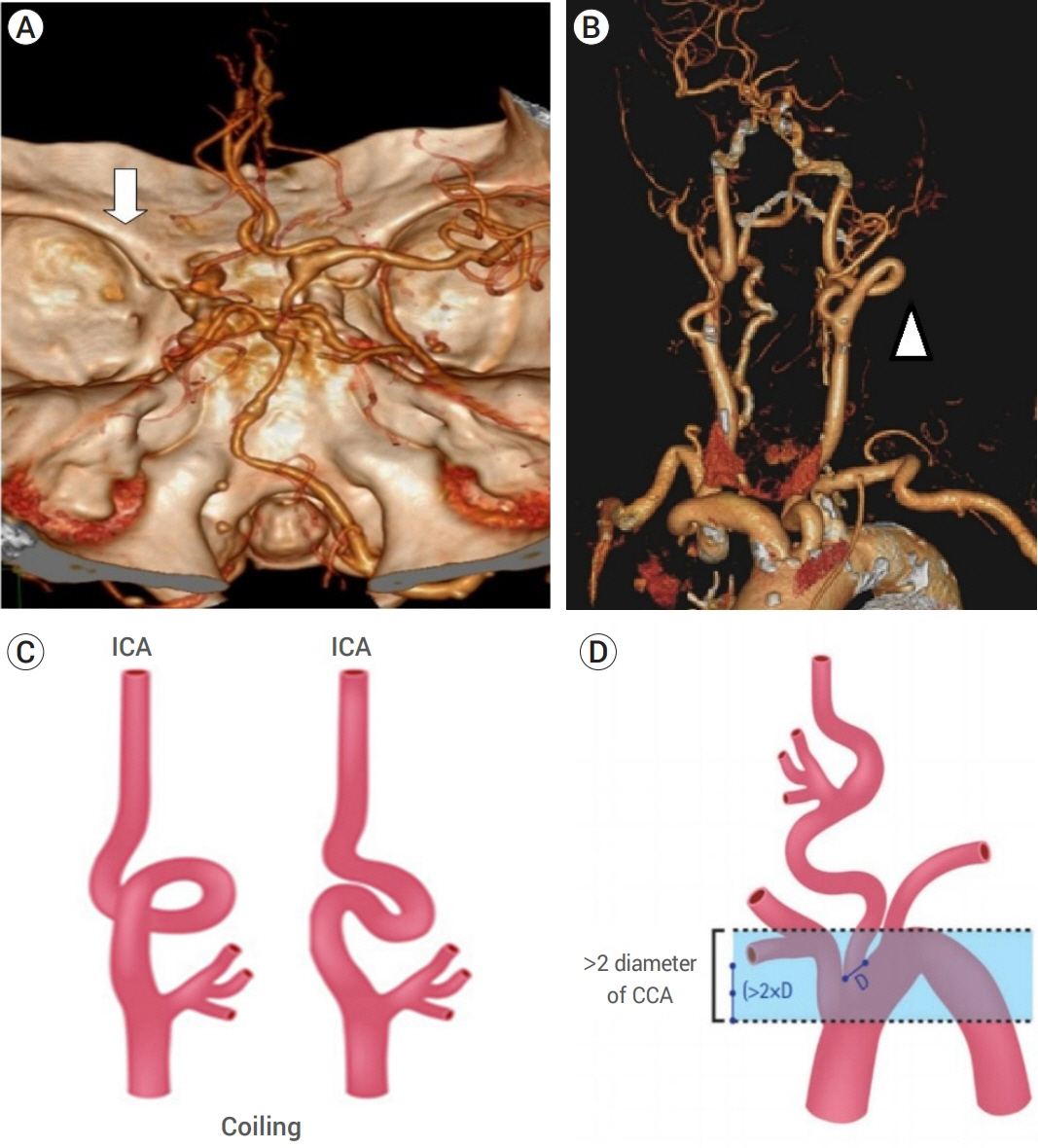
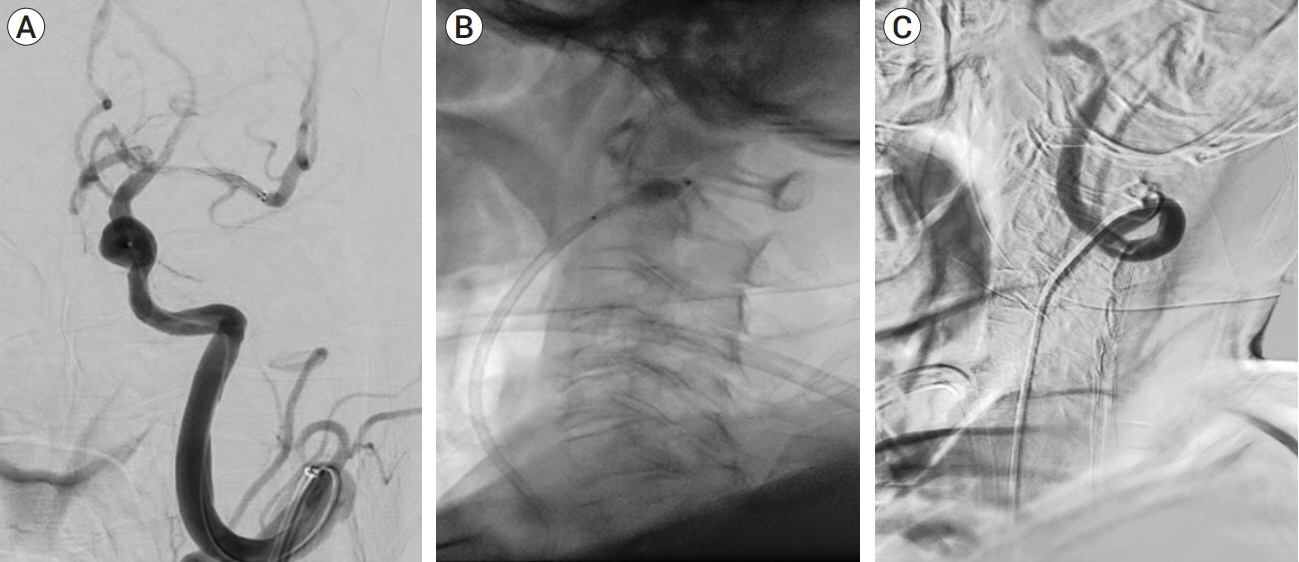
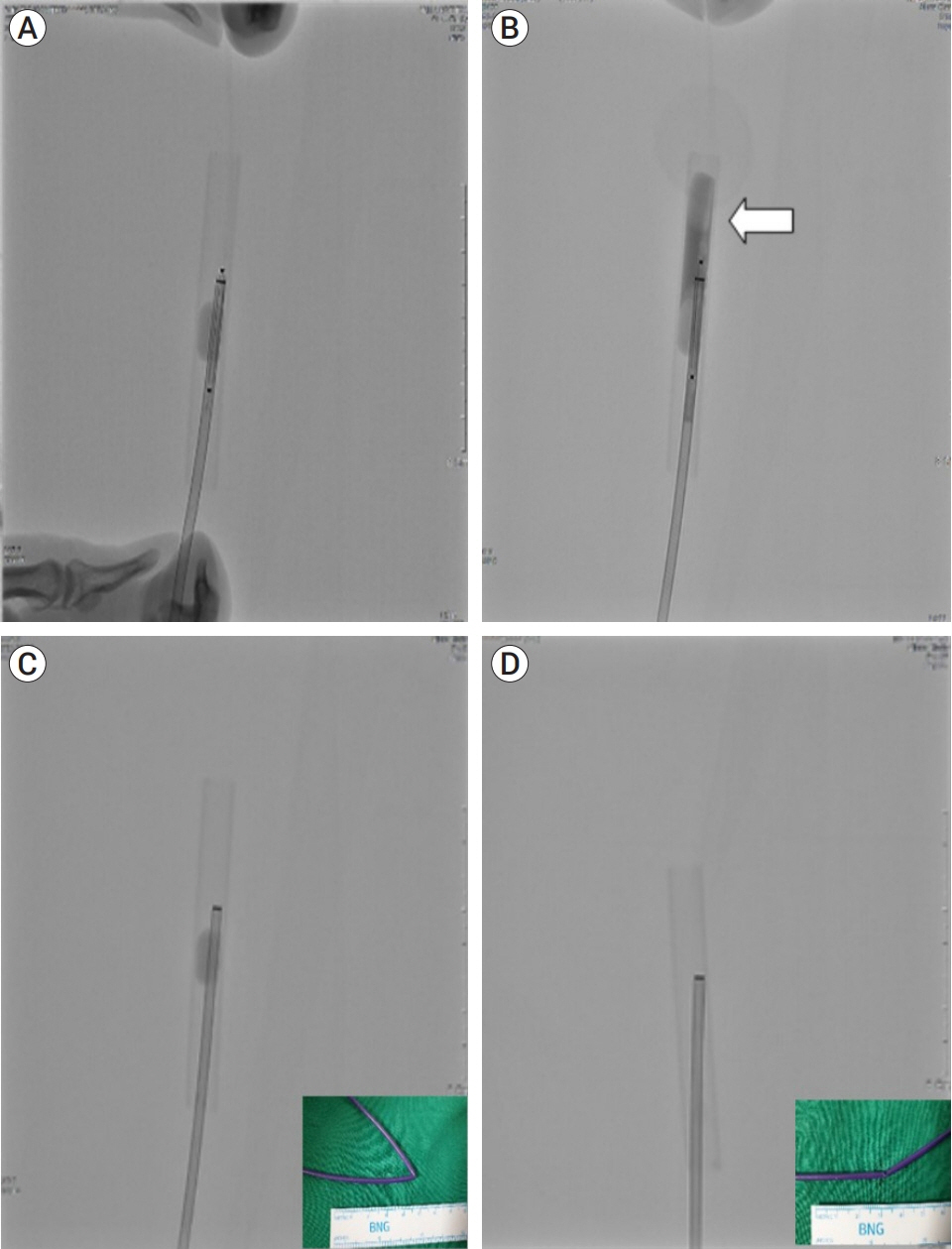
- The use of a balloon guide catheter (BGC) in the endovascular management of acute ischemic stroke is known to improve the efficacy and efficiency of the procedure by reducing the risk of distal embolization. During the procedure, the balloon of the catheter causes a temporary arrest of cerebral blood flow. However, failure of the balloon to deflate during the BGC procedure can result in catastrophic complications, including aggravated hypoxic damage.
This paper aims to share the resolution and methodological analysis of our experience with BGC balloon deflation failure, which was confirmed by a reproducible experiment under similar conditions.
Keyword
Figure
Reference
-
1. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; Feb. 378(8):708–18.
Article2. Alverne FJAM, Lima FO, Rocha FA, Bandeira DA, Lucena AFP, Silva HC, et al. Unfavorable vascular anatomy during endovascular treatment of stroke: challenges and bailout strategies. J Stroke. 2020; May. 22(2):185–202.
Article3. Baek JH, Kim BM, Kang DH, Heo JH, Nam HS, Kim YD, et al. Balloon guide catheter is beneficial in endovascular treatment regardless of mechanical recanalization modality. Stroke. 2019; Jun. 50(6):1490–6.
Article4. Barath P, Fishbein MC, Vari S, Forrester JS. Cutting balloon: a novel approach to percutaneous angioplasty. The American Journal of Cardiology. 1991; 68(11):1249–52.
Article5. Bosiers M, Deloose K, Verbist J, Peeters P. Scoring and cutting balloons for SFA disease treatment. Endovascular Today. 2008; 34–7.6. Brinjikji W, Starke RM, Murad MH, Fiorella D, Pereira VM, Goyal M, et al. Impact of balloon guide catheter on technical and clinical outcomes: a systematic review and meta-analysis. J Neurointerv Surg. 2018; Apr. 10(4):335–9.
Article7. Chueh JY, Kang DH, Kim BM, Gounis MJ. Role of balloon guide catheter in modern endovascular thrombectomy. J Korean Neurosurg Soc. 2020; Jan. 63(1):14–25.
Article8. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the Korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2016; Jan. 18(1):102–13.
Article9. Jeong DE, Kim JW, Kim BM, Hwang W, Kim DJ. Impact of balloon-guiding catheter location on recanalization in patients with acute stroke treated by mechanical thrombectomy. AJNR Am J Neuroradiol. 2019; May. 40(5):840–4.
Article10. Kang DH, Kim BM, Heo JH, Nam HS, Kim YD, Hwang YH, et al. Effect of balloon guide catheter utilization on contact aspiration thrombectomy. J Neurosurg. 2018; Nov. 1–7.
Article11. Kim MT, Park JH, Shin JH, Kim N, Kim SD, Tsauo J, et al. Influence of contrast agent dilution on ballon deflation time and visibility during tracheal balloon dilation: a 3D printed phantom study. Cardiovasc Intervent Radiol. 2017; Feb. 40(2):285–90.
Article12. Lapergue B, Blanc R, Guedin P, Decroix JP, Labreuche J, Preda C, et al. A direct aspiration, first pass technique (ADAPT) versus stent retrievers for acute stroke therapy: an observational comparative study. AJNR Am J Neuroradiol. 2016; Oct. 37(10):1860–5.
Article13. Leibundgut G, Degen C, Riede F. Transcutaneous puncture of an undeflatable coronary angioplasty balloon catheter. Case Rep Cardiol. 2018; Sep. 2018:6252809.
Article14. Mogabgab O, Patel VG, Michael TT, Kotsia A, Christopoulos G, Banerjee S, et al. Impact of contrast agent viscosity on coronary balloon deflation times: bench testing results. J Interv Cardiol. 2014; Apr. 27(2):177–81.
Article15. Nagata T, Masumoto K, Hayashi Y, Watanabe Y, Kato Y, Katou F. Three-dimensional computed tomographic analysis of variations of the carotid artery. J Craniomaxillofac Surg. 2016; Jun. 44(6):734–42.16. Nguyen TN, Malisch T, Castonguay AC, Gupta R, Sun CH, Martin CO, et al. Balloon guide catheter improves revascularization and clinical outcomes with the Solitaire device: analysis of the North American Solitaire Acute Stroke Registry. Stroke. 2014; Jan. 45(1):141–5.17. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; Jan. 378(1):11–21.18. Park GS, Ahn TH, Son MS, Shon JW, Ryu ES, Jin DK, et al. Clinical experience of cutting balloon angioplasty for in stent restenosis. Korean Circulation J. 2002; 32(4):317–21.
Article19. Pasamanickam K, Rajadurai J, Choo G-H. A new technique to puncture and remove a PTCA balloon that fails to deflate. Int J Angiol. 2020.
Article20. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; Dec. 50(12):e344–418.
Article21. Schonfeld MH, Kabiri R, Kniep HC, Meyer L, McDonough R, Sedlacik J, et al. Effect of balloon guide catheter utilization on the incidence of sub-angiographic peripheral emboli on high-resolution DWI after thrombectomy: a prospective observational study. Front Neurol. 2020; May. 11:386.22. Song HH, Kim KT, Chung SK, Kim YO, Yoon SA. Cutting balloon angioplasty for resistant venous stenoses of Brescia-Cimino fistulas. J Vasc Interv Radiol. 2004; Dec. 15(12):1463–7.
Article23. Spiotta AM, Fargen KM, Chaudry I, Turner RD, Turk AS. ADAPT: a direct aspiration first pass technique. Endovascular Today. 2016; 15(2):24. Takama T, Ito Y, Ishimori H, Tsukahara R, Muramatsu T. Failure of a balloon to deflate during post dilatation in a coronary artery. Cardiovasc Interv Ther. 2015; Jan. 30(1):57–60.
Article25. Takano Y, Currier JW, Yeatman LA, Kobashigawa JA, Rogers AD, Cianfichi LJ, et al. Cutting balloon angioplasty for cardiac transplant vasculopathy. J Heart Lung Transplant. 2002; Aug. 21(8):910–3.
Article26. Trivedi R. Double jeopardy: failure to deflate stent balloon in rescue angioplasty. Interv Med Appl Sci. 2019; Jun. 11(2):128–30.
Article27. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019; Jun. 11(6):535–8.
Article28. Velasco A, Buerke B, Stracke CP, Berkemeyer S, Mosimann PJ, Schwindt W, et al. Comparison of a balloon guide catheter and a non–balloon guide catheter for mechanical thrombectomy. Radiology. 2016; Jul. 280(1):169–76.
Article29. Wong J, Telischak N, Heit J, Moraff A, Dodd R, Do H, et al. Acute stroke intervention for large vessel occlusion with combined stent retreival and suction thrombectomy (solumbra technique): a retrospective analysis of 85 patients. J Neurointerv Surg. 2016; 8:A86.30. Yi HJ, Sung JH, Lee DH, Song SY. Effectiveness and technical considerations of solitaire platinum 4×40 mm stent retriever in mechanical thrombectomy with solumbra technique. J Korean Neurosurg Soc. 2020; Jan. 64(1):30–8.
Article31. Zaidat OO, Mueller-Kronast NH, Hassan AE, Haussen DC, Jadhav AP, Froehler MT, et al. Impact of balloon guide catheter use on clinical and angiographic outcomes in the STRATIS stroke thrombectomy registry. Stroke. 2019; Mar. 50(3):697–704.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Balloon Guide Catheter in Modern Endovascular Thrombectomy
- Radial artery access with a sheathless 0.087” inner diameter balloon guide catheter (Walrus) for neurointerventional procedures: Technique and clinical outcomes
- Effectiveness of Anchoring with Balloon Guide Catheter and Stent Retriever in Difficult Mechanical Thrombectomy for Large Vessel Occlusion
- Efficacy of Balloon-Guiding Catheter for Mechanical Thrombectomy in Patients with Anterior Circulation Ischemic Stroke
- Endovascular Removal of Entrapped Central Venous Catheter Guide Wire