Ann Pediatr Endocrinol Metab.
2022 Dec;27(4):320-324. 10.6065/apem.2142204.102.
Pituitary apoplexy in an adolescent male with macroprolactinoma presenting as middle cerebral artery territory infarction
- Affiliations
-
- 1Department of Paediatric Endocrinology, Variety Children Hospital, King’s College Hospital NHS Foundation Trust, London, UK
- 2Department of Neuroradiology, King’s College Hospital NHS Foundation Trust, London, UK
- 3Faculty of Medicine and Life Science, King’s College London, London, UK
- 4Department of Neurosurgery, King’s College Hospital NHS Foundation Trust, London, UK
- 5Department of Endocrinology, King’s College Hospital NHS Foundation Trust, London, UK
- KMID: 2537245
- DOI: http://doi.org/10.6065/apem.2142204.102
Abstract
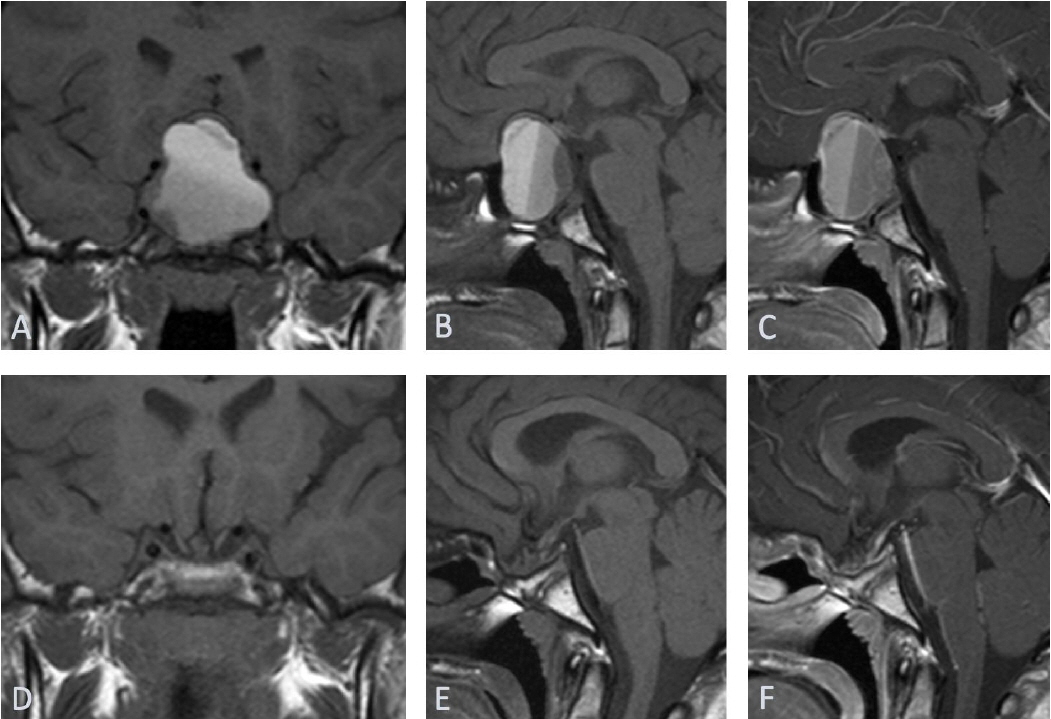
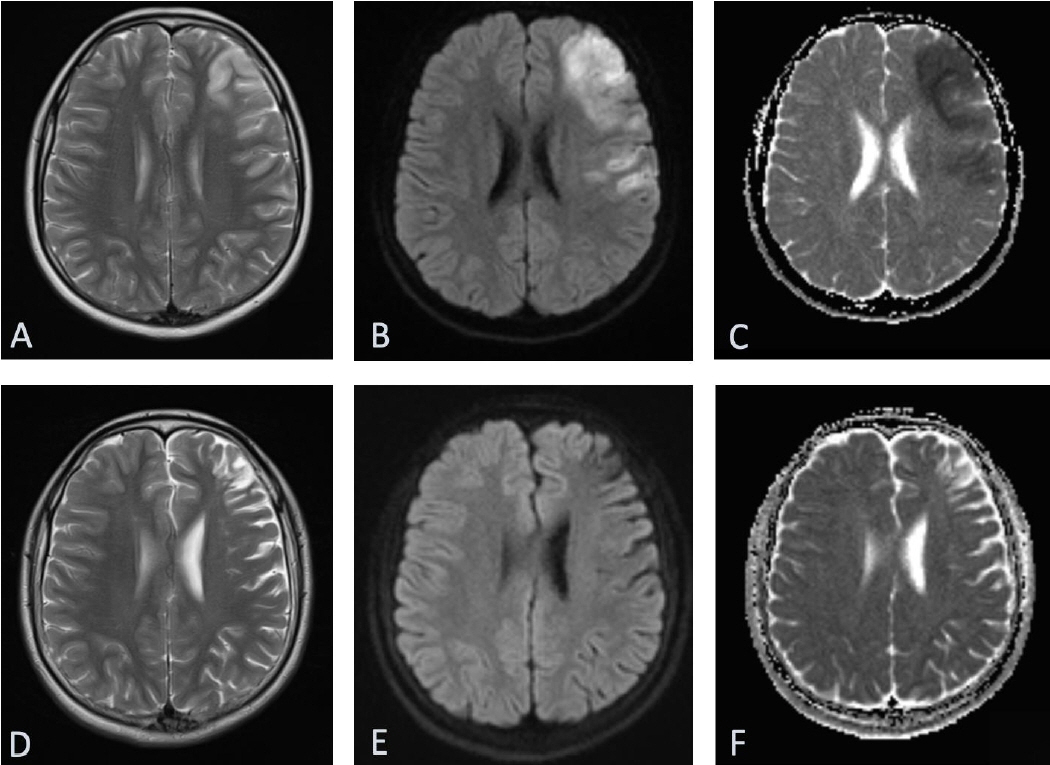
- Pituitary apoplexy typically presents with acute headache, vomiting, visual disturbance, and confusion. Herein, we report a rare presentation of ischemic stroke due to pituitary apoplexy. A 16.5-year-old male presented with reduced Glasgow Coma Scale (GCS) score, slurred speech, right-sided hemiparesis, and bitemporal hemianopia. Magnetic resonance imaging of the brain showed a large hemorrhagic sellar/suprasellar mass and an area of cortical T2/FLAIR hyperintensity with corresponding diffusion restriction in the middle cerebral artery territory. Computed tomography (CT) intracranial angiogram showed luminal occlusion of the clinoid and ophthalmic segments of both internal carotid arteries (ICAs, left>right) due to mass pressure effect. Biochemical investigations confirmed hyperprolactinemia and multiple pituitary hormone deficiencies. Stress-dose hydrocortisone was commenced with cabergoline, followed by urgent endoscopic transsphenoidal debulking of the tumor (subsequent histology showing prolactinoma). Postoperative CT angiogram showed improved caliber of ICAs. Intensive neurorehabilitation was implemented and resulted in complete recovery of motor and cognitive deficits. At the last assessment (18.8 years), the patient remained on complete anterior pituitary hormone replacement without cabergoline. Pituitary apoplexy is a medical emergency requiring prompt recognition and treatment and should be suspected in patients presenting with sudden, severe headache; nausea; or visual disturbance and meningism. Ischemic stroke is a rare manifestation of pituitary apoplexy in the pediatric population.
Keyword
Figure
Reference
-
References
1. Capatina C, Inder W, Karavitaki N, Wass JA. Management of endocrine disease: pituitary tumour apoplexy. Eur J Endocrinol. 2015; 172:R179–90.2. Banerjee C, Snelling B, Hanft S, Komotar RJ. Bilateral cerebral infarction in the setting of pituitary apoplexy: a case presentation and literature review. Pituitary. 2015; 18:352–8.3. Pozzati E, Frank G, Nasi MT, Giuliani G. Pituitary apoplexy, bilateral carotid vasospasm, and cerebral infarction in a 15-year-old boy. Neurosurgery. 1987; 20:56–9.4. Kasl RA, Hughes J, Burrows AM, Meyer FB. Pediatric ischemic stroke from an apoplectic prolactinoma. Childs Nerv Syst. 2015; 31:1387–92.5. Sibal L, Ball SG, Connolly V, James RA, Kane P, Kelly WF, et al. Pituitary apoplexy: a review of clinical presentation, management and outcome in 45 cases. Pituitary. 2004; 7:157–63.6. Oh T, Amara D, Gupta N, Clerkin P. A middle cerebral artery ischemic stroke occurring in a child with a large prolactinoma. Childs Nerv Syst. 2020; 36:853–6.7. Molitch ME, Cowen L, Stadiem R, Uihlein A, Naidich M, Russell E. Tumors invading the cavernous sinus that cause internal carotid artery compression are rarely pituitary adenomas. Pituitary. 2012; 15:598–600.8. Ayuk J, McGregor EJ, Mitchell RD, Gittoes NJ. Acute management of pituitary apoplexy--surgery or conservative management? Clin Endocrinol (Oxf). 2004; 61:747–52.9. Randeva HS, Schoebel J, Byrne J, Esiri M, Adams CB, Wass JA. Classical pituitary apoplexy: clinical features, management and outcome. Clin Endocrinol (Oxf ). 1999; 51:181–8.10. Reddy NL, Rajasekaran S, Han TS, Theodoraki A, Drake W, Vanderpump M, et al. An objective scoring tool in the management of patients with pituitary apoplexy. Clin Endocrinol (Oxf). 2011; 75:723.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reply to Commentary on "Pituitary apoplexy in an adolescent male with macroprolactinoma presenting as middle cerebral artery territory infarction"
- Pituitary Apoplexy due to Pituitary Adenoma Infarction
- Computed tomography of pituitary apoplexy: report of 2 cases
- Clinical Analysis of Pituitary Apoplexy
- Pituitary Apoplexy Presenting as Meningitis