Ann Rehabil Med.
2022 Dec;46(6):312-319. 10.5535/arm.22118.
Can a Biomechanical Foot Orthosis Affect Gait in Patients With Hallux Valgus? A Pilot Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, Chungnam National University, Daejeon, Korea
- KMID: 2537162
- DOI: http://doi.org/10.5535/arm.22118
Abstract
Objective
To investigate the effects of customized biomechanical foot orthosis (BFO) on kinematic data during gait in patients with hallux valgus (HV) deformities and compare the results with those of a normal control group.
Methods
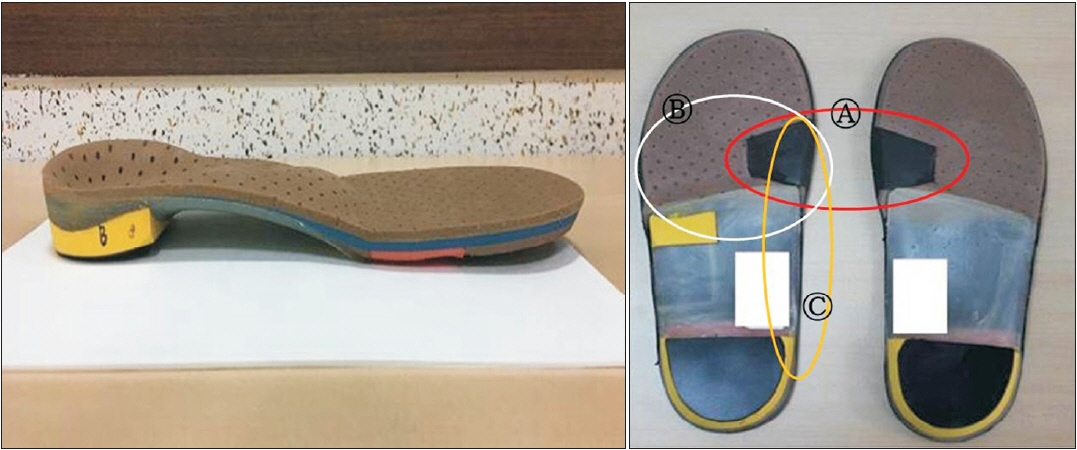
Ten patients with HV deformities and 10 healthy volunteers were enrolled in this study. HV deformity was diagnosed using biomechanical and radiological assessments by a rehabilitation physician. Patients received the customized BFO manufactured at a commercial orthosis laboratory (Biomechanics, Goyang, South Korea) according to the strictly defined procedure by a single experienced technician. The spatiotemporal and kinematic data acquired by the Vicon 3D motion capture system (Oxford Metrics, Oxford, UK) were compared between the intervention groups (control vs. HV without orthosis) and between the HV groups (with vs. without orthosis).
Results
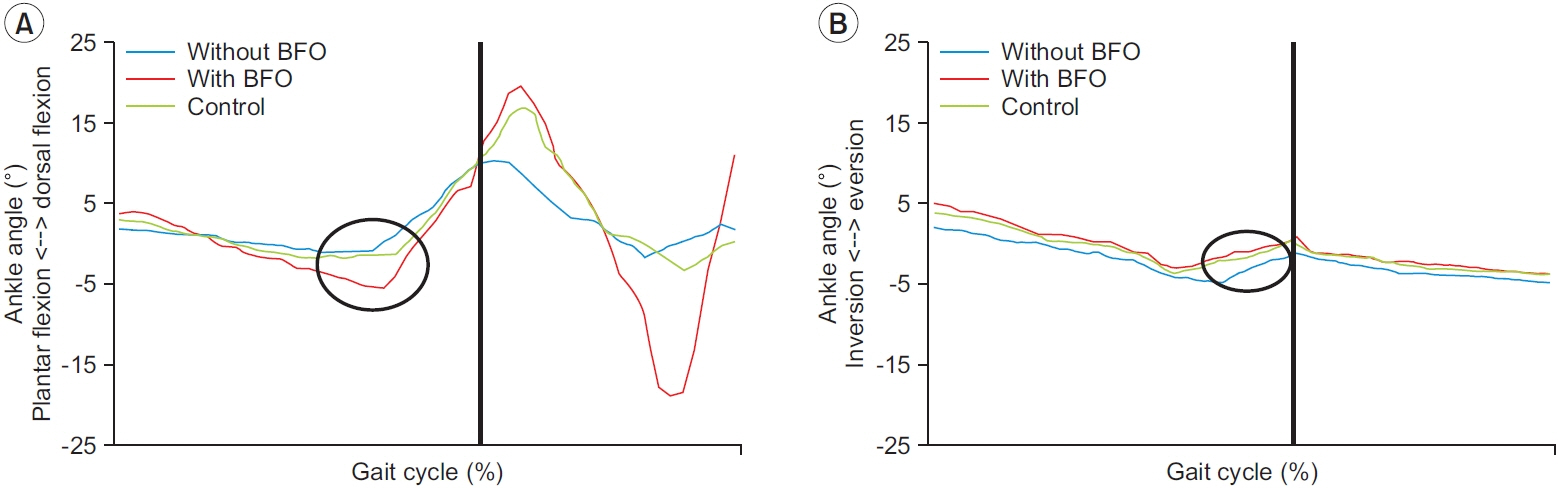
The temporal-spatial and kinematic parameters of the HV group were significantly different from those of the control group. After applying BFO to the HV group, significantly increased ranges of plantar flexion motion and hindfoot inversion were observed. Furthermore, the HV group with BFO showed improved gait cadence, walking speed, and stride length, although the results were not statistically significant.
Conclusion
Our results suggest that it is imperative to understand the pathophysiology of HV, and the application of customized BFO can be useful for improving kinematics in HV deformities.
Keyword
Figure
Reference
-
1. Nix SE, Vicenzino BT, Collins NJ, Smith MD. Gait parameters associated with hallux valgus: a systematic review. J Foot Ankle Res. 2013; 6:9.2. Adams PF, Hendershot GE, Marano MA; Centers for Disease Control and Prevention/National Center for Health Statistics. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10. 1999; (200):1–203.3. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010; 3:21.4. Jang KS, Kim TW, Kim HJ. Diagnosis and Pathophysiology of hallux valgus. J Korean Foot Ankle Soc. 2014; 18:43–7.5. Shih KS, Chien HL, Lu TW, Chang CF, Kuo CC. Gait changes in individuals with bilateral hallux valgus reduce first metatarsophalangeal loading but increase knee abductor moments. Gait Posture. 2014; 40:38–42.6. Menz HB, Lord SR. Gait instability in older people with hallux valgus. Foot Ankle Int. 2005; 26:483–9.7. Torkki M, Malmivaara A, Seitsalo S, Hoikka V, Laippala P, Paavolainen P. Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA. 2001; 285:2474–80.8. Klugarova J, Janura M, Svoboda Z, Sos Z, Stergiou N, Klugar M. Hallux valgus surgery affects kinematic parameters during gait. Clin Biomech (Bristol, Avon). 2016; 40:20–6.9. Lee SH, Lee YC. Approach for the treatment on hallux valgus. J Korean Foot Ankle Soc. 2019; 23:143–8.10. Charrette M. Bunion formation and orthotic support. Dyn Chiropr. 2009; 27:1–3.11. Kwan MY, Yick KL, Yip J, Tse CY. Hallux valgus orthosis characteristics and effectiveness: a systematic review with meta-analysis. BMJ Open. 2021; 11:e047273.12. Deschamps K, Birch I, Desloovere K, Matricali GA. The impact of hallux valgus on foot kinematics: a cross-sectional, comparative study. Gait Posture. 2010; 32:102–6.13. Stebbins J, Harrington M, Thompson N, Zavatsky A, Theologis T. Repeatability of a model for measuring multi-segment foot kinematics in children. Gait Posture. 2006; 23:401–10.14. Root ML, Weed JH, Orien WP. Neutral position casting techniques. Los Angeles: Clinical Biomechanics Corporation;1971.15. Hamacher D, Singh NB, Van Dieen JH, Heller MO, Taylor WR. Kinematic measures for assessing gait stability in elderly individuals: a systematic review. J R Soc Interface. 2011; 8:1682–98.16. Canseco K, Long J, Marks R, Khazzam M, Harris G. Quantitative characterization of gait kinematics in patients with hallux rigidus using the Milwaukee foot model. J Orthop Res. 2008; 26:419–27.17. Canseco K, Rankine L, Long J, Smedberg T, Marks RM, Harris GF. Motion of the multisegmental foot in hallux valgus. Foot Ankle Int. 2010; 31:146–52.18. Chopra S, Moerenhout K, Crevoisier X. Characterization of gait in female patients with moderate to severe hallux valgus deformity. Clin Biomech (Bristol, Avon). 2015; 30:629–35.19. Becerro de Bengoa Vallejo R, Sanchez Gomez R, Losa Iglesias ME. Clinical improvement in functional hallux limitus using a cut-out orthosis. Prosthet Orthot Int. 2016; 40:215–23.20. Callisaya ML, Blizzard L, Schmidt MD, McGinley JL, Srikanth VK. Ageing and gait variability: a population-based study of older people. Age Ageing. 2010; 39:191–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forefoot disorders and conservative treatment
- Incidence of Hallux Valgus Interphalangeus in the Normal and Hallux Valgus Feet and its Correlations with Hallux Valgus Angle and Intermetatarsal Angle
- Technique Tip: A Simple Method to Treat Hallux Valgus with Severe Metatarsus Adductus
- Relationship between Foot Width Reduction and Clinical Outcomes after Chevron Osteotomy for Hallux Valgus Deformity
- Consideration of Various Medial Capsulorrhaphy Methods in Hallux Valgus Surgery