Cardiovasc Prev Pharmacother.
2021 Oct;3(4):82-85. 10.36011/cpp.2021.3.e13.
Diabetes in People with Disabilities: a Call for Action
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2536934
- DOI: http://doi.org/10.36011/cpp.2021.3.e13
Abstract
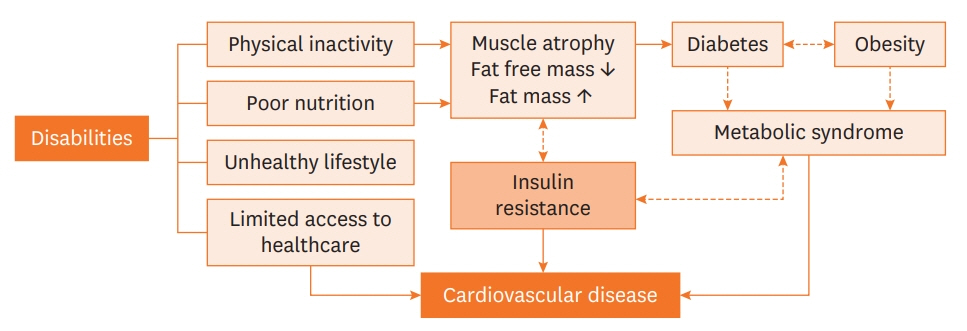
- Previous researchers have suggested that people with disabilities have a higher prevalence and risk of type 2 diabetes mellitus than the general population. As diabetes is a well-known risk factor for cardiovascular disease (CVD), developing strategies to prevent and delay its occurrence in people with disabilities is important to reduce the burden of CVD. However, people with disabilities are often excluded from studies and have received little attention from public health authorities and researchers. These unmet needs for health care and being left out of research may affect the progression of diabetes in people with disabilities. Herein, we would like to briefly discuss the increased risk of diabetes and related conditions in people with disabilities and suggest that more attention should be given to this population.
Figure
Reference
-
1. World Health Organization. International Classification of Functioning, Disability and Health: Children & Youth Version: ICF-CY. Geneva: World Health Organization;2007.2. Sabatello M, Landes SD, McDonald KE. People with disabilities in COVID-19: Fixing our priorities. Am J Bioeth. 2020; 20:187–90.
Article3. Lee JE, Kim HR, Shin HI. Accessibility of medical services for persons with disabilities: comparison with the general population in Korea. Disabil Rehabil. 2014; 36:1728–34.
Article4. Khavjou OA, Anderson WL, Honeycutt AA, Bates LG, Razzaghi H, Hollis ND, Grosse SD. National health care expenditures associated with disability. Med Care. 2020; 58:826–32.
Article5. Cooper SA, Hughes-McCormack L, Greenlaw N, McConnachie A, Allan L, Baltzer M, McArthur L, Henderson A, Melville C, McSkimming P, Morrison J. Management and prevalence of long-term conditions in primary health care for adults with intellectual disabilities compared with the general population: a population-based cohort study. J Appl Res Intellect Disabil. 2018; 31 Suppl 1:68–81.
Article6. Son KY, Kim SH, Sunwoo S, Lee JY, Lim S, Kim YS. Association between disability and cardiovascular event and mortality: a nationwide representative longitudinal study in Korea. PLoS One. 2020; 15:e0236665.
Article7. National Institute for Health and Care Excellence (NICE). Type 2 Diabetes. Full Guidance, 26 January 2011. London: NICE;2013.8. Jung I, Kwon H, Park SE, Han KD, Park YG, Rhee EJ, Lee WY. The prevalence and risk of type 2 diabetes in adults with disabilities in Korea. Endocrinol Metab (Seoul). 2020; 35:552–61.
Article9. Axmon A, Ahlström G, Höglund P. Prevalence and treatment of diabetes mellitus and hypertension among older adults with intellectual disability in comparison with the general population. BMC Geriatr. 2017; 17:272.
Article10. MacRae S, Brown M, Karatzias T, Taggart L, Truesdale-Kennedy M, Walley R, Sierka A, Northway R, Carey M, Davies M. Diabetes in people with intellectual disabilities: a systematic review of the literature. Res Dev Disabil. 2015; 47:352–74.
Article11. Anderson WL, Wiener JM, Khatutsky G, Armour BS. Obesity and people with disabilities: the implications for health care expenditures. Obesity (Silver Spring). 2013; 21:E798–804.
Article12. Liou TH, Pi-Sunyer FX, Laferrère B. Physical disability and obesity. Nutr Rev. 2005; 63:321–31.
Article13. Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health. 2004; 94:443–5.
Article14. Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G. Body composition assessment in spinal cord injury subjects. Acta Diabetol. 2003; 40 Suppl 1:S183–6.
Article15. Jones LM, Legge M, Goulding A. Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil. 2003; 84:1068–71.16. Hoey E, Staines A, Walsh D, Corby D, Bowers K, Belton S, Meegan S, McVeigh T, McKeon M, Trépel D, Griffin P, Sweeney MR. An examination of the nutritional intake and anthropometric status of individuals with intellectual disabilities: results from the SOPHIE study. J Intellect Disabil. 2017; 21:346–65.
Article17. Bartlo P, Klein PJ. Physical activity benefits and needs in adults with intellectual disabilities: systematic review of the literature. Am J Intellect Dev Disabil. 2011; 116:220–32.
Article18. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003; 289:76–9.
Article19. Hwang B, Chun SM, Park JH, Shin HI. Unmet healthcare needs in people with disabilities: comparison with the general population in Korea. Ann Rehabil Med. 2011; 35:627–35.
Article20. McColl MA, Jarzynowska A, Shortt S. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc. 2010; 25:205–18.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Why Fast COVID-19 Vaccination Needed for People with Disabilities and Autistics in Korea?
- Qualitative Research to Build a Nutrition Education Program Operation Model at Social Welfare Facilities for People with Disabilities: One-On-One In-Depth Interview
- The Prevalence and Risk of Type 2 Diabetes in Adults with Disabilities in Korea
- Literature Review about Sexual Adjustment for Chronic Illness and Disabilities
- Years of Life Lost due to Premature Death in People with Disabilities in Korea: the Korean National Burden of Disease Study Framework