Endocrinol Metab.
2020 Sep;35(3):552-561. 10.3803/EnM.2020.653.
The Prevalence and Risk of Type 2 Diabetes in Adults with Disabilities in Korea
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 3Department of Biostatistics, Biomedicine & Health Sciences, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2508004
- DOI: http://doi.org/10.3803/EnM.2020.653
Abstract
- Background
People with disabilities are at risk of secondary conditions such as diabetes. The aim of this study was to evaluate the prevalence and risk of type 2 diabetes in South Korea, especially among people with all types of disabilities.
Methods
We conducted a cross-sectional study using data from the Korean National Health Insurance Service, with two disabilityfree controls matched for each participant with disabilities by age and sex. Information regarding the type, severity and grade of disabilities was obtained based on the National Disability Registry. Diagnosis of type 2 diabetes was defined according to the following criteria: presence of International Classification of Diseases, Tenth Revision, Clinical Modification codes E11, E12, E13, or E14 and claims for at least one oral anti-diabetic agent or insulin at baseline, or fasting glucose level ≥126 mg/dL.
Results
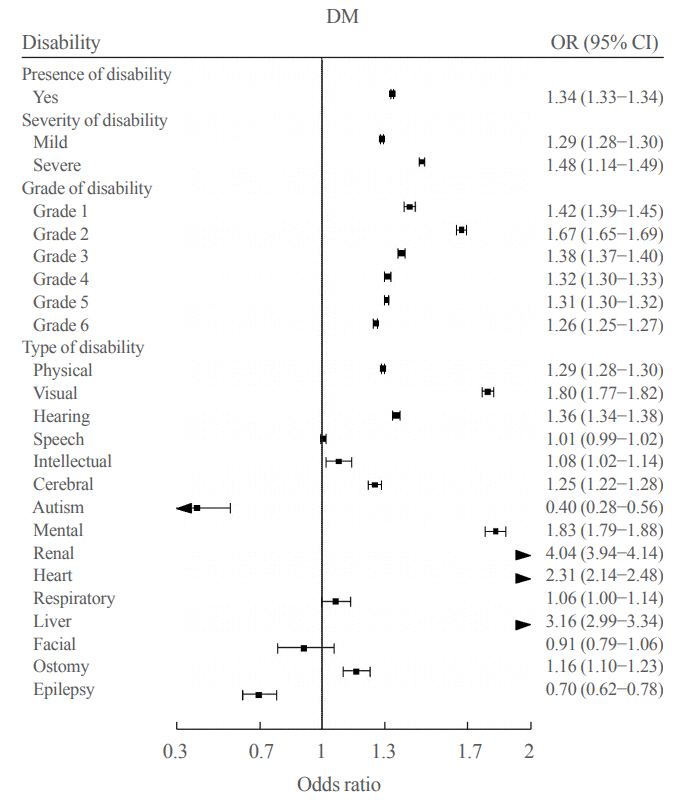
We included 1,297,806 participants with disabilities and 2,943,719 control. Out of 4,241,525 participants, 841,990 (19.9%) were diagnosed with diabetes. The prevalence of diabetes was higher in the disability group compared with individuals without disabilities (23.1% vs. 18.4%). The odds of having diabetes was higher in the disability group compared with the control group (adjusted odds ratio, 1.34; 95% confidence interval, 1.33 to 1.34). The results showed higher prevalence of diabetes in the mildly disabled group (23.2%) than in the severely disabled group (22.7%).
Conclusion
The prevalence and risk of diabetes were higher in people with disabilities compared with the general population. Physicians and public health authorities should focus on people with disabilities for proper diabetes management.
Keyword
Figure
Cited by 1 articles
-
Diabetes in People with Disabilities: a Call for Action
Inha Jung, Eun-Jung Rhee, Won-Young Lee
Cardiovasc Prev Pharmacother. 2021;3(4):82-85. doi: 10.36011/cpp.2021.3.e13.
Reference
-
1. World Health Organization. International classification of impairments, disabilities, and handicaps: a manual of classification relating to the consequences of disease. Geneva: World Health Organization;1980.2. Kim SH, Byun YC, Son CG, Lee YH, Lee MK, Lee SH, et al. National survey on persons with disabilities [Internet]. Sejong: Korea Ministry of Health and Welfare;2011. [cited 2020 Jul 1]. Available from: https://www.kihasa.re.kr/web/publication/research/view.do?menuId=44&tid=71&bid=12&division=002&ano=1328.3. World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization;2001.4. Jeon B, Kwon S, Kim H. Health care utilization by people with disabilities: a longitudinal analysis of the Korea Welfare Panel Study (KoWePS). Disabil Health J. 2015; 8:353–62.
Article5. Lee JE, Kim HR, Shin HI. Accessibility of medical services for persons with disabilities: comparison with the general population in Korea. Disabil Rehabil. 2014; 36:1728–34.
Article6. Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health. 2004; 94:443–5.
Article7. Jones LM, Legge M, Goulding A. Factor analysis of the metabolic syndrome in spinal cord-injured men. Metabolism. 2004; 53:1372–7.
Article8. Bauman WA, Spungen AM, Adkins RH, Kemp BJ. Metabolic and endocrine changes in persons aging with spinal cord injury. Assist Technol. 1999; 11:88–96.
Article9. MacRae S, Brown M, Karatzias T, Taggart L, TruesdaleKennedy M, Walley R, et al. Diabetes in people with intellectual disabilities: a systematic review of the literature. Res Dev Disabil. 2015; 47:352–74.
Article10. Lee KS, Won JU, Kim SY, Sohn MS, Youm YS, Lee YS, et al. Development of the Korean Academy of Medical Sciences Guideline for rating physical impairment. J Korean Med Sci. 2009; 24 Suppl 2(Suppl 2):S221–6.
Article11. Kim WH, Park YG, Shin HI, Im SH. The world report on disability and recent developments in South Korea. Am J Phys Med Rehabil. 2014; 93(1 Suppl 1):S58–62.
Article12. Lunsky Y, Lin E, Balogh R, Klein-Geltink J. Datapoints: diabetes prevalence among persons with serious mental illness and developmental disability. Psychiatr Serv. 2011; 62:830.
Article13. Kocina P. Body composition of spinal cord injured adults. Sports Med. 1997; 23:48–60.
Article14. Bauman WA, Adkins RH, Spungen AM, Waters RL. The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord. 1999; 37:765–71.
Article15. Karlsson AK. Insulin resistance and sympathetic function in high spinal cord injury. Spinal Cord. 1999; 37:494–500.
Article16. Myllynen P, Koivisto VA, Nikkila EA. Glucose intolerance and insulin resistance accompany immobilization. Acta Med Scand. 1987; 222:75–81.
Article17. International Diabetes Federation. IDF diabetes atlas. 8th ed. Brussels: International Diabetes Federation;2017.18. Gregg EW, Engelgau MM, Narayan V. Complications of diabetes in elderly people. BMJ. 2002; 325:916–7.
Article19. Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G. Body composition assessment in spinal cord injury subjects. Acta Diabetol. 2003; 40 Suppl 1:S183–6.
Article20. Bandini LG, Schoeller DA, Fukagawa NK, Wykes LJ, Dietz WH. Body composition and energy expenditure in adolescents with cerebral palsy or myelodysplasia. Pediatr Res. 1991; 29:70–7.
Article21. Liou TH, Pi-Sunyer FX, Laferrere B. Physical disability and obesity. Nutr Rev. 2005; 63:321–31.
Article22. Bartlo P, Klein PJ. Physical activity benefits and needs in adults with intellectual disabilities: systematic review of the literature. Am J Intellect Dev Disabil. 2011; 116:220–32.
Article23. Ewing G, McDermott S, Thomas-Koger M, Whitner W, Pierce K. Evaluation of a cardiovascular health program for participants with mental retardation and normal learners. Health Educ Behav. 2004; 31:77–87.
Article24. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesityrelated health risk factors, 2001. JAMA. 2003; 289:76–9.
Article25. Freemantle N, Holmes J, Hockey A, Kumar S. How strong is the association between abdominal obesity and the incidence of type 2 diabetes? Int J Clin Pract. 2008; 62:1391–6.
Article26. Emerson E, Baines S. Health inequalities and people with learning disabilities in the UK: 2010 [Internet]. Glasgow: Centre for Excellence for Children’s Care and Protection (CELCIS);2011. [cited 2020 Jul 1]. Available from: https://strathprints.strath.ac.uk/34862/.
Article27. Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Rep. 2004; 119:418–26.
Article28. McColl MA, Jarzynowska A, Shortt SE. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc. 2010; 25:205–18.
Article29. Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Rep. 2004; 119:418–26.
Article30. Lee SY, Jung KY, Lee IK, Yi SD, Cho YW, Kim DW, et al. Prevalence of treated epilepsy in Korea based on national health insurance data. J Korean Med Sci. 2012; 27:285–90.
Article31. Eyman RK, Grossman HJ, Chaney RH, Call TL. The life expectancy of profoundly handicapped people with mental retardation. N Engl J Med. 1990; 323:584–9.
Article32. Melville CA, Cooper SA, McGrother CW, Thorp CF, Collacott R. Obesity in adults with Down syndrome: a case-control study. J Intellect Disabil Res. 2005; 49(Pt 2):125–33.
Article33. Klein R, Klein BE, Moss SE. Visual impairment in diabetes. Ophthalmology. 1984; 91:1–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diabetes in People with Disabilities: a Call for Action
- Diabetes Risk Score for Korean Adults
- A Comparison of the Prevalence of Cardiovascular Disease and Lifestyle Habits by Disability Status and Type of Disability in Korean Adults: A Propensity Score Matching Analysis
- Response: Projection of Diabetes Prevalence in Korean Adults for the Year 2030 Using Risk Factors Identified from National Data (Diabetes Metab J 2019;43:90–6)
- Management of Type 2 Diabetes Mellitus in Adolescents and Young Adults