Neonatal Med.
2022 Nov;29(4):135-140. 10.5385/nm.2022.29.4.135.
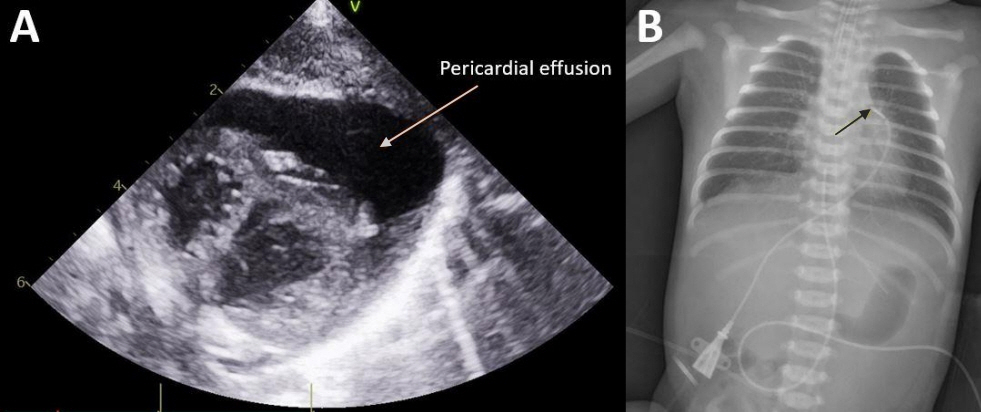
Rapidly Progressive Pericardial Effusion and Cardiac Tamponade in a Term Infant with an Umbilical Venous Catheter: A Case Report
- Affiliations
-
- 1Department of Pediatrics, Hanyang University Hospital, Seoul, Korea
- 2Department of Pediatrics, Hanyang University School of Medicine, Seoul, Korea
- 3Department of Pediatrics, Hanyang University Guri Hospital, Guri, Korea
- KMID: 2536659
- DOI: http://doi.org/10.5385/nm.2022.29.4.135
Abstract
- Pericardial effusion (PCE) in neonates has various clinical presentations depending on the amount and speed of fluid accumulation and can cause cardiac tamponade (CT). We report a case of rapidly accumulating PCE and near-fatal CT with an umbilical venous catheter successfully resolved by emergent echo-guided pericardiocentesis in a term infant who had been hospitalized with meconium aspiration syndrome and persistent pulmonary hypertension. This case report suggests that if a patient with an intracardiac umbilical catheter shows sudden cardiopulmonary instability, the possibility of PCE and CT should be considered. Furthermore, if necessary, emergency drainage of the PCE and removal of the umbilical catheter should be immediately performed.
Figure
Reference
-
1. Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, et al. Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J Am Soc Echocardiogr. 2011; 24:1057–78.2. Kuhn B, Peters J, Marx GR, Breitbart RE. Etiology, management, and outcome of pediatric pericardial effusions. Pediatr Cardiol. 2008; 29:90–4.3. Liz CF, Domingues S, Pinho L, Lopes L, Carvalho C, Magalhaes M, et al. Neonatal pericardial effusion: case report and review of the literature. J Pediatr Neonatal Individ Med. 2020; 9:e090111.4. Warren M, Thompson KS, Popek EJ, Vogel H, Hicks J. Pericardial effusion and cardiac tamponade in neonates: sudden unexpected death associated with total parenteral nutrition via central venous catheterization. Ann Clin Lab Sci. 2013; 43:163–71.5. Nowlen TT, Rosenthal GL, Johnson GL, Tom DJ, Vargo TA. Pericardial effusion and tamponade in infants with central catheters. Pediatrics. 2002; 110(1 Pt 1):137–42.6. Schlapbach LJ, Pfammatter JP, Nelle M, McDougall FJ. Cardiomegaly in a premature neonate after venous umbilical catheterization. Eur J Pediatr. 2009; 168:107–9.7. Unal S, Arifoglu I, Celik IH, Yilmaz O, Bas AY, Demirel N. Pleural and pericardiac effusion as a complication of properly placed umbilical venous catheter. J Neonatal Surg. 2017; 6:34.8. Pettit J. Assessment of infants with peripherally inserted central catheters: part 1. detecting the most frequently occurring complications. Adv Neonatal Care. 2002; 2:304–15.9. Sertic AJ, Connolly BL, Temple MJ, Parra DA, Amaral JG, Lee KS. Perforations associated with peripherally inserted central catheters in a neonatal population. Pediatr Radiol. 2018; 48:10919.10. Weil BR, Ladd AP, Yoder K. Pericardial effusion and cardiac tamponade associated with central venous catheters in children: an uncommon but serious and treatable condition. J Pediatr Surg. 2010; 45:1687–92.11. Nadroo AM, Glass RB, Lin J, Green RS, Holzman IR. Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics. 2002; 110(1 Pt 1):131–6.12. Ohki Y, Maruyama K, Harigaya A, Kohno M, Arakawa H. Complications of peripherally inserted central venous catheter in Japanese neonatal intensive care units. Pediatr Int. 2013; 55:185–9.13. Srinivasan HB, Tjin-A-Tam A, Galang R, Hecht A, Srinivasan G. Migration patterns of peripherally inserted central venous catheters at 24 hours postinsertion in neonates. Am J Perinatol. 2013; 30:871–4.14. Shannon D. Central venous catheter-induced pericardial effusion in a neonate: a case study and recommendations for practice. Neonatal Netw. 2014; 33:341–8.15. Jain A, McNamara PJ, Ng E, El-Khuffash A. The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am J Perinatol. 2012; 29:101–6.16. Fusco FP, De Carolis MP, Costa S, De Rosa G, Zambraro A, Romagnoli C. Cardiac complications in preterm infants with percutaneous long lines: the importance of early diagnosis. Resuscitation. 2008; 79:506–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Treatment of Cardiac Tamponade Associated with Umbilical Venous Catheter by Pericardiocentesis in Two Neonates: Two Case Reports
- Umbilical venous line-related pleural and pericardial effusion causing cardiac tamponade in a premature neonate: A case report
- Umbilical Venous Catheter Related Cardiac Tamponade in an Extremely Low Birth Weight Infant: A Case Report
- A Case of Unilateral Pleural Effusion Due to Percutaneously Inserted Central Venous Catheterization
- Early-onset Pericardial Effusion after Peripherally Inserted Central Venous Catheterization in a Preterm Infant