Ann Hepatobiliary Pancreat Surg.
2022 Nov;26(4):333-338. 10.14701/ahbps.22-001.
The single-stage management of bile duct stones is underutilised: A prospective multicentre cohort study with a literature review
- Affiliations
-
- 1Department of HPB Surgery, University Hospitals Plymouth NHS Trust, Plymouth, United Kingdom
- 2Department of Upper GI Surgery, Torbay Hospital, Torquay, United Kingdom
- 3Department of HPB Surgery, Queen Elizabeth Hospital, Birmingham, United Kingdom
- KMID: 2536383
- DOI: http://doi.org/10.14701/ahbps.22-001
Abstract
- Backgrounds/Aims
Bile duct stones (BDS) can be managed either prior to laparoscopic cholecystectomy (LC) using endoscopic retrograde cholangiopancreatography (ERCP) or with laparoscopic bile duct exploration (LBDE) at the time of LC. The latter is underutilised. The aim of this study was to use the dataset of the previously performed CholeS study to investigate LBDE hospital volumes, LBDE-to-LC rates, and LBDE outcomes.
Methods
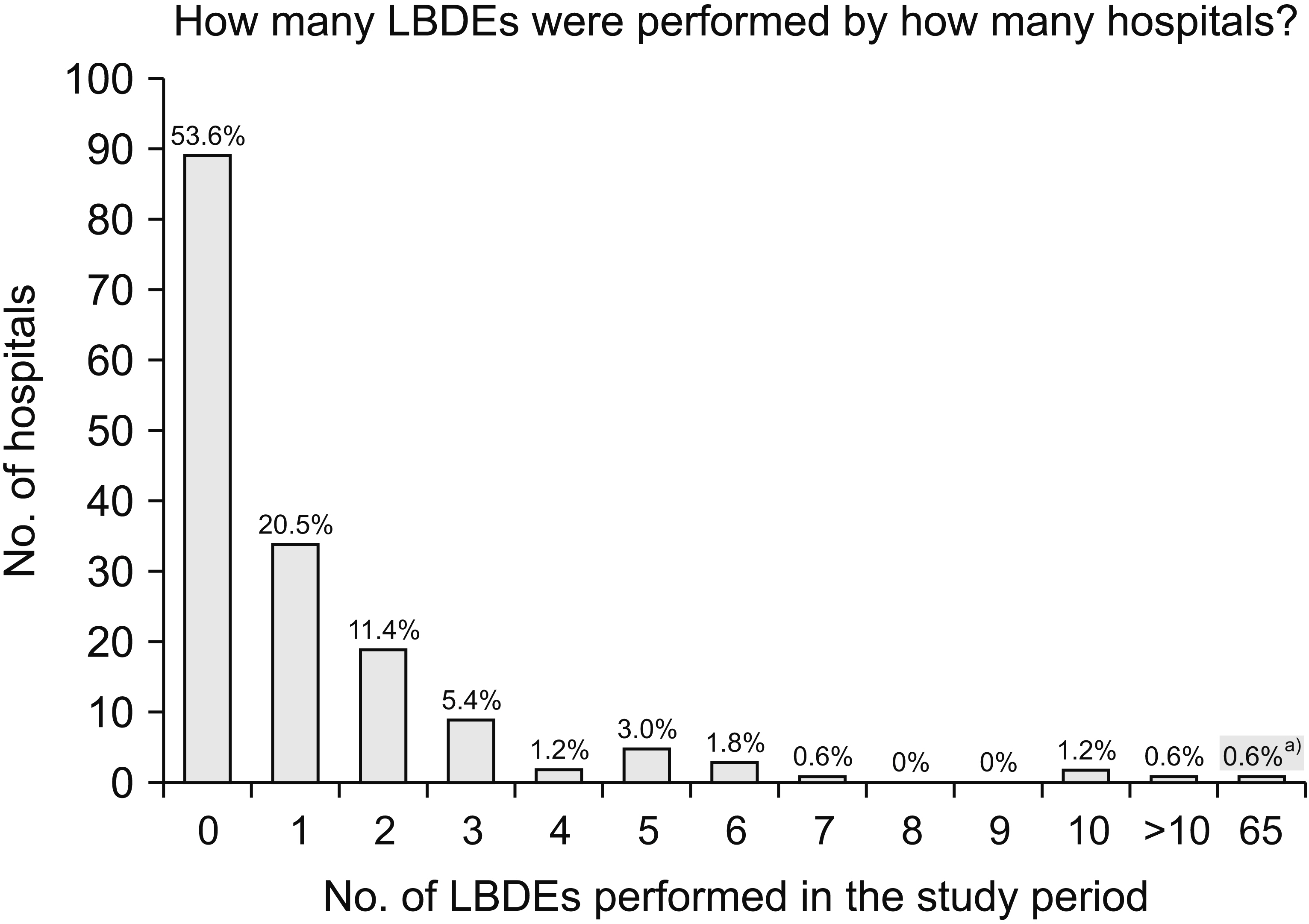
Data from 166 United Kingdom/Republic of Ireland hospitals were used to study the utilisation of LBDE in LC patients.
Results
Of 8,820 LCs performed, 932 patients (10.6%) underwent preoperative ERCP and 256 patients (2.9%) underwent LBDE. Of the 256 patients who underwent LBDE, 73 patients (28.5%) had undergone prior ERCP and 112 patients (43.8%) had undergone prior magnetic resonance cholangiopancreatography. Fifteen (9.0%) of the 166 included hospitals performed less than five LBDEs in the two-month study period. LBDEs were mainly performed by upper gastrointestinal surgeons (84.4%) and colorectal surgeons (10.0%). Eighty-seven percent of the LBDEs were performed by consultants and 13.0% were performed by trainees. The laparoscopic-to-open conversion rate was 12.5%. The median operation time was 111 minutes (range: 75–155 minutes). Median hospital stay was 6 days (range: 4–11 days) for emergency LBDEs and 1 day (range: 1–4 days) for elective LBDEs. Overall morbidity was 21.5%. Bile leak rate was 5.3%. Thirty-day readmission and mortality rates were 12.1% and 0.4%, respectively.
Conclusions
The single-stage approach to managing BDS was underutilised. An additional prospective study with a longer study period is needed to verify this finding.
Keyword
Figure
Reference
-
1. Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, et al. 2017; Updated guideline on the management of common bile duct stones (CBDS). Gut. 66:765–782. DOI: 10.1136/gutjnl-2016-312317. PMID: 28122906.2. Lyu Y, Cheng Y, Li T, Cheng B, Jin X. 2019; Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc. 33:3275–3286. DOI: 10.1007/s00464-018-06613-w. PMID: 30511313.3. Vohra RS, Spreadborough P, Johnstone M, Marriott P, Bhangu A, Alderson D, et al. 2015; Protocol for a multicentre, prospective, population-based cohort study of variation in practice of cholecystectomy and surgical outcomes (The CholeS study). BMJ Open. 5:e006399. DOI: 10.1136/bmjopen-2014-006399. PMID: 25582453. PMCID: PMC4298090.4. CholeS Study Group, West Midlands Research Collaborative. 2016; Population-based cohort study of variation in the use of emergency cholecystectomy for benign gallbladder diseases. Br J Surg. 103:1716–1726. DOI: 10.1002/bjs.10288. PMID: 27748962.5. Griffiths EA, Hodson J, Vohra RS, Marriott P, Katbeh T, Zino S, et al. 2019; Utilisation of an operative difficulty grading scale for laparoscopic cholecystectomy. Surg Endosc. 33:110–121. DOI: 10.1007/s00464-018-6281-2. PMID: 29956029. PMCID: PMC6336748.6. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. 2007; Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 335:806–808. DOI: 10.1136/bmj.39335.541782.AD. PMID: 17947786. PMCID: PMC2034723.7. Tanase A, Aroori S, Dhanda A, Cramp M, Streeter A. 2021; A UK survey on variation in practice of management of choledocholithiasis and laparoscopic common bile duct exploration (ALiCE Survey). HPB. 23(Suppl 3):S943–S944. DOI: 10.1016/j.hpb.2021.08.590.8. Vannijvel M, Lesurtel M, Bouckaert W, Houben B, Knol J, Vangertruyden G, et al. 2016; A survey of European-African surgeons' management of common bile duct stones. HPB (Oxford). 18:959–964. DOI: 10.1016/j.hpb.2016.10.007. PMID: 27838253. PMCID: PMC5144544.9. Teitelbaum E, Soper N, Patel P, Santos BF, Hungness ES. 2015. A survey to assess surgeon experience with, and barriers to performing, laparoscopic common bile duct exploration for teatment of choledocholithiasis [Internet]. Los Angeles: Society of American Gastrointestinal and Endoscopic Surgeons;Available from: https://www.sages.org/meetings/annual-meeting/abstracts-archive/a-survey-to-assess-surgeon-experience-with-and-barriers-to-performing-laparoscopic-common-bile-duct-exploration-for-teatment-of-choledocholithiasis/. cited 2022 Jan 12.10. Zhu H, Wu L, Yuan R, Wang Y, Liao W, Lei J, et al. 2018; Learning curve for performing choledochotomy bile duct exploration with primary closure after laparoscopic cholecystectomy. Surg Endosc. 32:4263–4270. DOI: 10.1007/s00464-018-6175-3. PMID: 29602995.11. Wandling MW, Hungness ES, Pavey ES, Stulberg JJ, Schwab B, Yang AD, et al. 2016; Nationwide assessment of trends in choledocholithiasis management in the United States from 1998 to 2013. JAMA Surg. 151:1125–1130. DOI: 10.1001/jamasurg.2016.2059. PMID: 27556900.12. Poulose BK, Arbogast PG, Holzman MD. 2006; National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc. 20:186–190. DOI: 10.1007/s00464-005-0235-1. PMID: 16362476.13. Al-Ardah M, Barnett RE, Morris S, Abdelrahman T, Nutt M, Boyce T, et al. 2021; Lessons learnt from the first 200 unselected consecutive cases of laparoscopic exploration of common bile duct stones at a district general hospital. Surg Endosc. 35:6268–6277. DOI: 10.1007/s00464-020-08127-w. PMID: 33140155.14. Aawsaj Y, Light D, Horgan L. 2016; Laparoscopic common bile duct exploration: 15-year experience in a district general hospital. Surg Endosc. 30:2563–2566. DOI: 10.1007/s00464-015-4523-0. PMID: 26307600.15. Navaratne L, Martinez Isla A. 2021; Transductal versus transcystic laparoscopic common bile duct exploration: an institutional review of over four hundred cases. Surg Endosc. 35:437–448. DOI: 10.1007/s00464-020-07522-7. PMID: 32246237.16. Zhang WJ, Xu GF, Huang Q, Luo KL, Dong ZT, Li JM, et al. 2015; Treatment of gallbladder stone with common bile duct stones in the laparoscopic era. BMC Surg. 15:7. DOI: 10.1186/1471-2482-15-7. PMID: 25623774. PMCID: PMC4417333.17. Baucom RB, Feurer ID, Shelton JS, Kummerow K, Holzman MD, Poulose BK. 2016; Surgeons, ERCP, and laparoscopic common bile duct exploration: do we need a standard approach for common bile duct stones? Surg Endosc. 30:414–423. DOI: 10.1007/s00464-015-4273-z. PMID: 26092008.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Advances in the Management of Recurrent Bile Duct Stones
- Concurrent Yellow-to-white and Black Extrahepatic Bile Duct Stones
- Clinical Practice Guideline for Common Bile Duct Stones: Diagnosis and Treatment
- One-stage versus two-stage approach for concomitant gallbladder and common bile duct stones: which one is more proper in patients over 80 years old?
- Application of Electrohydraulic Lithotripsy for Bile Duct Stones Difficult to Remove