Korean J Gastroenterol.
2015 Nov;66(5):251-254. 10.4166/kjg.2015.66.5.251.
Recent Advances in the Management of Recurrent Bile Duct Stones
- Affiliations
-
- 1Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea. gidrdong@daum.net
- KMID: 2373352
- DOI: http://doi.org/10.4166/kjg.2015.66.5.251
Abstract
- Approximately 3-15% of patients who have undergone removal of bile duct stones with endoscopic sphincterotomy have recurrence of stones which often presents as acute cholangitis. Despite better understanding on the factors and mechanisms underlying the recurrence of bile duct stones achieved during the past few decades, endoscopic removal still remains the mainstay of management for recurrent bile duct stones. Recently investigated and suggested management of recurrent bile duct stones are highlighted in this review.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc. 2006; 20:1594–1599.
Article2. Hawes RH, Cotton PB, Vallon AG. Follow-up 6 to 11 years after duodenoscopic sphincterotomy for stones in patients with prior cholecystectomy. Gastroenterology. 1990; 98:1008–1012.
Article3. Prat F, Malak NA, Pelletier G, et al. Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology. 1996; 110:894–899.
Article4. Ando T, Tsuyuguchi T, Okugawa T, et al. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003; 52:116–121.
Article5. Pereira-Lima JC, Jakobs R, Winter UH, et al. Longterm results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998; 48:457–464.
Article6. Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V. Longterm follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002; 34:273–279.
Article7. Shin D, Moon D, Kim S, Hwang Y, Yun Y. The factors influencing the treatment results of residual & recurrent biliary stones. Korean J Hepatobiliary Pancreat Surg. 2002; 6:59–66.8. Kim TH, Hwang JC, Kim JH, Kim YS, Kim DU, Seo DW. Clinical practice guidelines for common bile duct stones: purpose and process of guideline development. Korean J Pancreas Biliary Tract. 2013; 18:1–5.
Article9. Kim DI, Kim MH, Lee SK, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001; 54:42–48.
Article10. Cheon YK, Lehman GA. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006; 18:461–464.
Article11. Lai KH, Peng NJ, Lo GH, et al. Prediction of recurrent choledocholithiasis by quantitative cholescintigraphy in patients after endoscopic sphincterotomy. Gut. 1997; 41:399–403.
Article12. Ohashi A, Tamada K, Wada S, et al. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009; 21:73–77.
Article13. Hammarstrom LE, Holmin T, Stridbeck H. Endoscopic treatment of bile duct calculi in patients with gallbladder in situ: long-term outcome and factors. Scand J Gastroenterol. 1996; 31:294–301.14. Cetta F. The role of bacteria in pigment gallstone disease. Ann Surg. 1991; 213:315–326.
Article15. Bowser L, Schutz SM. The role of surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Gastrointest Endosc. 2000; 51:247–248.16. Maple JT, Ikenberry SO, Anderson MA, et al. ASGE Standards of Practice Committee. The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc. 2011; 74:731–744.
Article17. Geenen DJ, Geenen JE, Jafri FM, et al. The role of surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Endoscopy. 1998; 30:18–20.
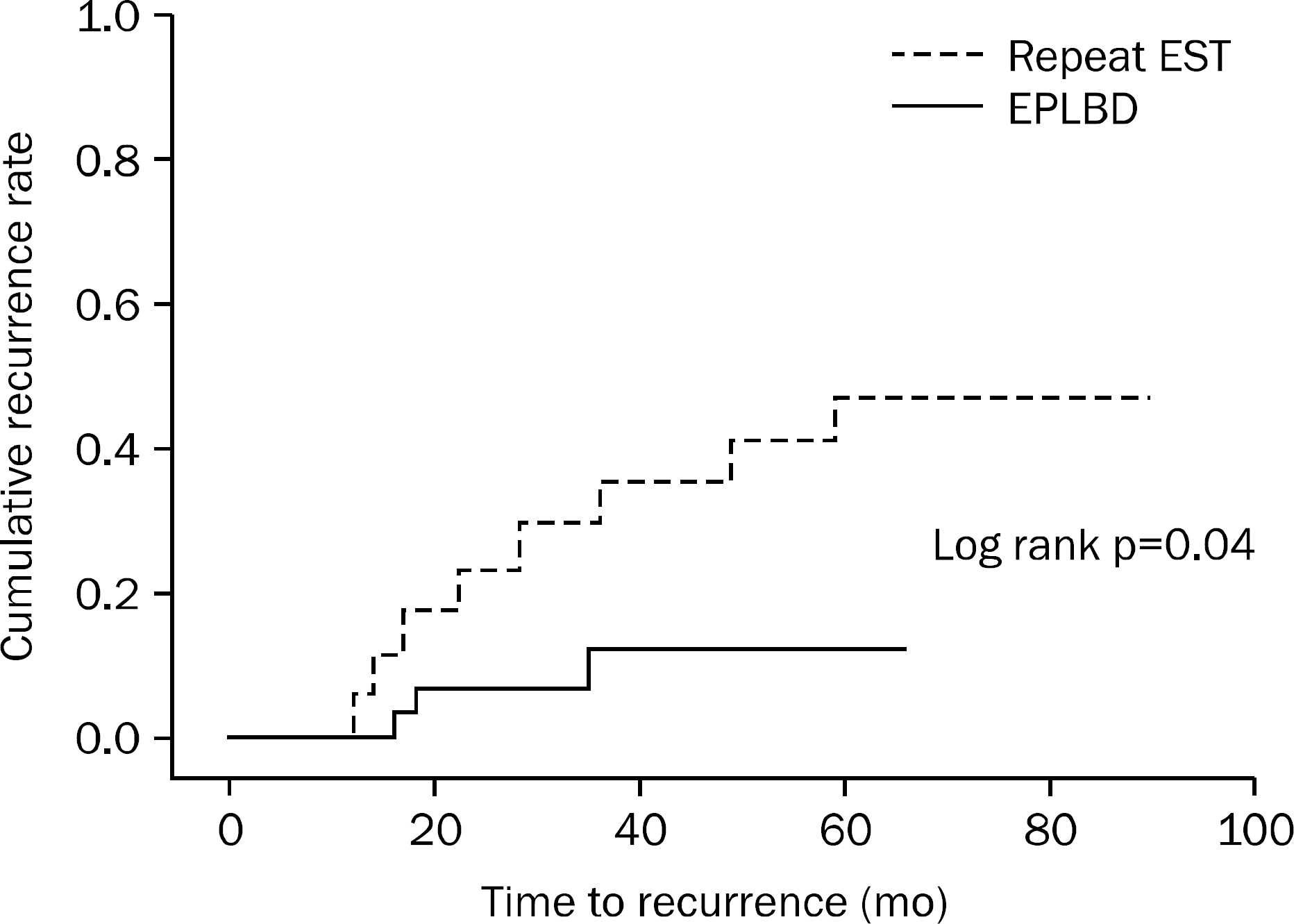
Article18. Harada R, Maguchi H, Takahashi K, et al. Large balloon dilation for the treatment of recurrent bile duct stones prevents short-term recurrence in patients with previous endoscopic sphincterotomy. J Hepatobiliary Pancreat Sci. 2013; 20:498–503.
Article19. Miller K, Hell E, Lang B, Lengauer E. Gallstone formation prophylaxis after gastric restrictive procedures for weight loss: a randomized double-blind placebo-controlled trial. Ann Surg. 2003; 238:697–702.20. Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. British Society of Gastroenterology. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008; 57:1004–1021.
Article21. Swobodnik W, Janowitz P, Kratzer W, et al. Preventing the recurrence of common bile duct calculi following endoscopic papillotomy with ursodeoxycholic acid. Z Gastroenterol. 1990; 28:621–625.22. Baek YH, Kim HJ, Park JH, et al. Risk factors for recurrent bile duct stones after endoscopic clearance of common bile duct stones. Korean J Gastroenterol. 2009; 54:36–41.
Article23. Sugiyama M, Suzuki Y, Abe N, Masaki T, Mori T, Atomi Y. Endoscopic retreatment of recurrent choledocholithiasis after sphincterotomy. Gut. 2004; 53:1856–1859.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Practice Guideline for Common Bile Duct Stones: Diagnosis and Treatment
- Non-Operative Management in Residual and Recurrent Bile Duct Stones
- The Surgical Treatments for the Hepatolithiasis
- Need to identify the risk factor for stone recurrence after common bile duct exploration
- Concurrent Yellow-to-white and Black Extrahepatic Bile Duct Stones