Anesth Pain Med.
2022 Oct;17(4):386-396. 10.17085/apm.22164.
Critical incidents associated with pediatric anesthesia: changes over 6 years at a tertiary children’s hospital
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2535337
- DOI: http://doi.org/10.17085/apm.22164
Abstract
- Background
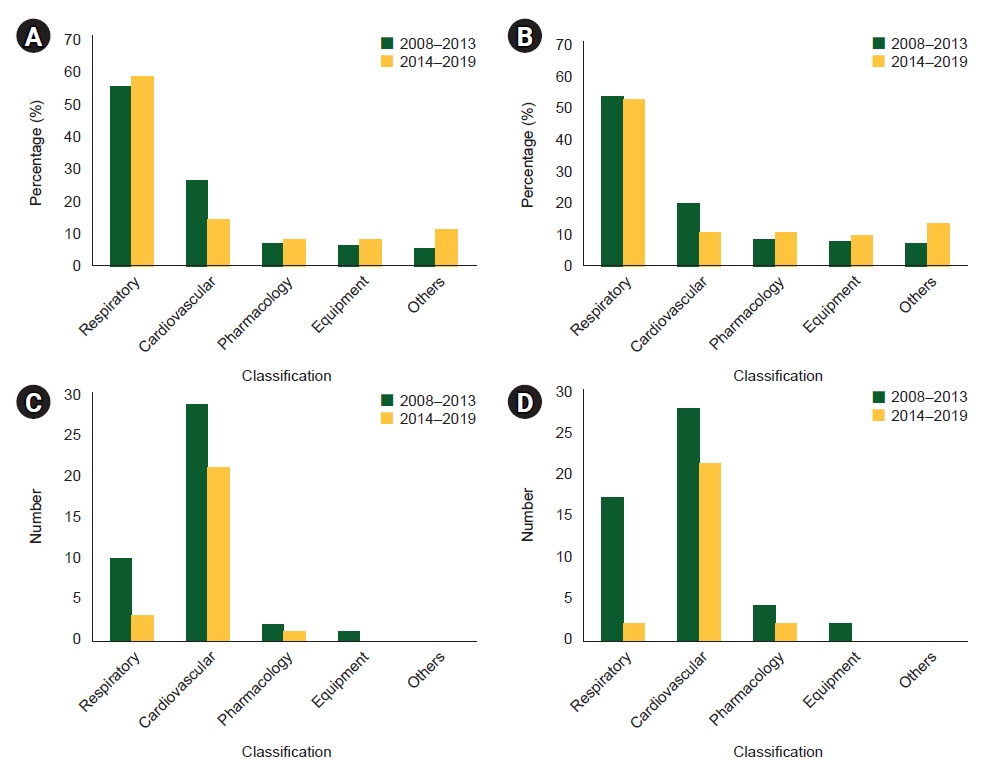
Sustained interest is needed in the characteristics of critical incidents in pediatric anesthesia and related changes, for determining the causes and degree of potential harm; this will also improve the quality of medical care. This study aimed to analyze the incidence of critical incidents recorded in 2014–2019, and to compare them with those in 2008–2013.
Methods
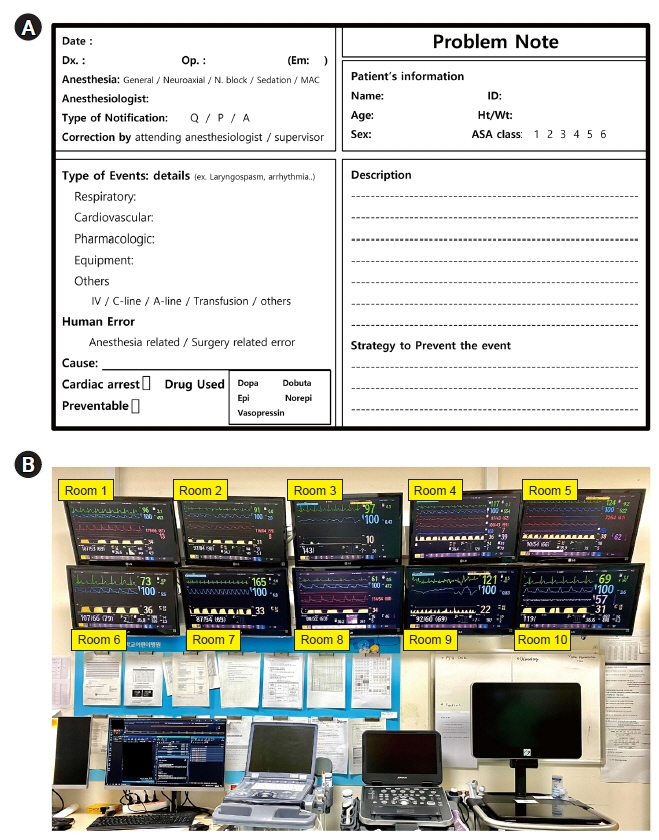
Critical incidents associated with pediatric anesthesia, including cardiac arrest, recorded in a voluntary departmental reporting system between January 2014 and December 2019 were compared with those reported between January 2008 and August 2013 using chi-square test.
Results
We identified 295 (0.55%) critical incidents from 53,541 cases of pediatric anesthesia (3,471 cardiothoracic surgeries); this is consistent with the previously reported incidence of 0.46%. Among the critical incidents, the incidences of adverse events, sentinel event, near miss case and no-harm events were 93.9%, 1.7%, 0%, and 6.1% in 2014–2019, whereas those were 98.3%, 2.6%, 1.7%, and 0% in 2008–2013 (P = 0.023, 0.686, 0.080, and < 0.001, respectively). Cardiac arrest accounted for 25 (8.5%) cases of the 295 critical events, which significantly lower than that previously reported (18.3%; P = 0.020). Human factor-related events accounted for 61.0% of all critical incidences; this was similar to the previous data (58.5%).
Conclusions
Over six years, there has been no significant difference in the total incidence of critical events. Despite the decrease in the incidence of serious critical events, perioperative care in pediatric anesthesia can be further improved.
Keyword
Figure
Reference
-
1. Morray JP, Geiduschek JM, Ramamoorthy C, Haberkern CM, Hackel A, Caplan RA, et al. Anesthesia-related cardiac arrest in children: initial findings of the Pediatric Perioperative Cardiac Arrest (POCA) registry. Anesthesiology. 2000; 93:6–14.2. Dias R, Dave N, Chiluveru S, Garasia M. Critical incidents in paediatric anaesthesia: a prospective analysis over a 1 year period. Indian J Anaesth. 2016; 60:801–6.
Article3. MacLennan AI, Smith AF. An analysis of critical incidents relevant to pediatric anesthesia reported to the UK National Reporting and Learning System, 2006-2008. Paediatr Anaesth. 2011; 21:841–7.
Article4. Lim CW, Lee JH, Im SM, Song IK, Park HP, Kim HS, et al. Characteristics of 1-day postoperative mortality: a comparison with 2- to 7-day postoperative mortality. Acta Anaesthesiol Scand. 2016; 60:432–40.
Article5. Lee JH, Kim EK, Song IK, Kim EH, Kim HS, Kim CS, et al. Critical incidents, including cardiac arrest, associated with pediatric anesthesia at a tertiary teaching children's hospital. Paediatr Anaesth. 2016; 26:409–17.
Article6. Bhananker SM, Ramamoorthy C, Geiduschek JM, Posner KL, Domino KB, Haberkern CM, et al. Anesthesia-related cardiac arrest in children: update from the pediatric perioperative cardiac arrest registry. Anesth Analg. 2007; 105:344–50.
Article7. Abbasi S, Khan FA, Khan S. Pediatric critical incidents reported over 15 years at a tertiary care teaching hospital of a developing country. J Anaesthesiol Clin Pharmacol. 2018; 34:78–83.
Article8. Habre W, Disma N, Virag K, Becke K, Hansen TG, Jöhr M; APRICOT Group of the European Society of Anaesthesiology Clinical Trial Network, et al. Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir Med 2017; 5: 412-425. Erratum in:. Lancet Respir Med. 2017; 5:e19. e22.9. Wan S, Siow YN, Lee SM, Ng A. Audits and critical incident reporting in paediatric anaesthesia: lessons from 75,331 anaesthetics. Singapore Med J. 2013; 54:69–74.10. Neale G, Chapman EJ, Hoare J, Olsen S. Recognising adverse events and critical incidents in medical practice in a district general hospital. Clin Med (Lond). 2006; 6:157–62.
Article11. Habre W. Pediatric anesthesia after APRICOT (Anaesthesia PRactice In Children Observational Trial): who should do it? Curr Opin Anaesthesiol. 2018; 31:292–6.12. Kumar RK. Teamwork in pediatric heart care. Ann Pediatr Cardiol. 2009; 2:140–5.
Article13. Leahy IC, Lavoie M, Zurakowski D, Baier AW, Brustowicz RM. Medication errors in a pediatric anesthesia setting: Incidence, etiologies, and error reduction strategies. J Clin Anesth. 2018; 49:107–11.
Article14. Lobaugh LMY, Martin LD, Schleelein LE, Tyler DC, Litman RS. Medication errors in pediatric anesthesia: a report from the wake up safe quality improvement initiative. Anesth Analg. 2017; 125:936–42.15. Jones CPL, Fawker-Corbett J, Groom P, Morton B, Lister C, Mercer SJ. Human factors in preventing complications in anaesthesia: a systematic review. Anaesthesia. 2018; 73 Suppl 1:12–24.
Article16. Llewellyn RL, Gordon PC, Wheatcroft D, Lines D, Reed A, Butt AD, et al. Drug administration errors: a prospective survey from three South African teaching hospitals. Anaesth Intensive Care. 2009; 37:93–8.17. Billstein-Leber M, Carrillo CJD, Cassano AT, Moline K, Robertson JJ. ASHP guidelines on preventing medication errors in hospitals. Am J Health Syst Pharm. 2018; 75:1493–517.
Article18. Cho HY, Shin S, Lee S, Yoon S, Lee HJ. Analysis of endotracheal intubation-related judicial precedents in South Korea. Korean J Anesthesiol. 2021; 74:506–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How do You Select an Anesthesia Method Prior to Tympanostomy Tube Insertion for a Child?
- Intraoperative pediatric electroencephalography monitoring: an updated review
- Developing brain in children and anesthesia
- Low-flow anesthesia in children: theory and clinical practice
- Influence of Patient Safety Culture, Ethical Nursing Competence, and Nursing Professionalism on the Perception of Disclosure of Patient Safety Incidents among Nurses in Tertiary Hospitals