Acute Crit Care.
2022 Aug;37(3):363-371. 10.4266/acc.2021.01627.
Ability of a modified Sequential Organ Failure Assessment score to predict mortality among sepsis patients in a resource-limited setting
- Affiliations
-
- 1Division of Critical Care Medicine, Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Thailand
- KMID: 2535300
- DOI: http://doi.org/10.4266/acc.2021.01627
Abstract
- Copyright © 2022 The Korean Society of
Critical Care Medicine
This is an Open Access article distributed
under the terms of Creative Attributions Non-
Commercial License (https://creativecommons.
org/li-censes/by-nc/4.0/) which permits
unrestricted noncommercial use, distribution,
and reproduction in any medium, provided the
original work is properly cited.
https://www.accjournal.org 363
INTRODUCTION
Sepsis is a life-threatening condition and constitutes major health care problems around the world [1,2]. Sepsis was associated with nearly 20% of all global deaths, and the majority of sepsis cases occurred in low- or middle-income countries [1]. In 2017, the World Health Organization recommended actions to reduce the global burden of sepsis [2]. Sepsis has been defined as acute life-threatening organ dysfunction due to dysregulation of host responses to
Background: Some variables of the Sequential Organ Failure Assessment (SOFA) score are not routinely measured in sepsis patients, especially in countries with limited resources. Therefore, this study was conducted to evaluate the accuracy of the modified SOFA (mSOFA) and compared its ability to predict mortality in sepsis patients to that of the original SOFA score.
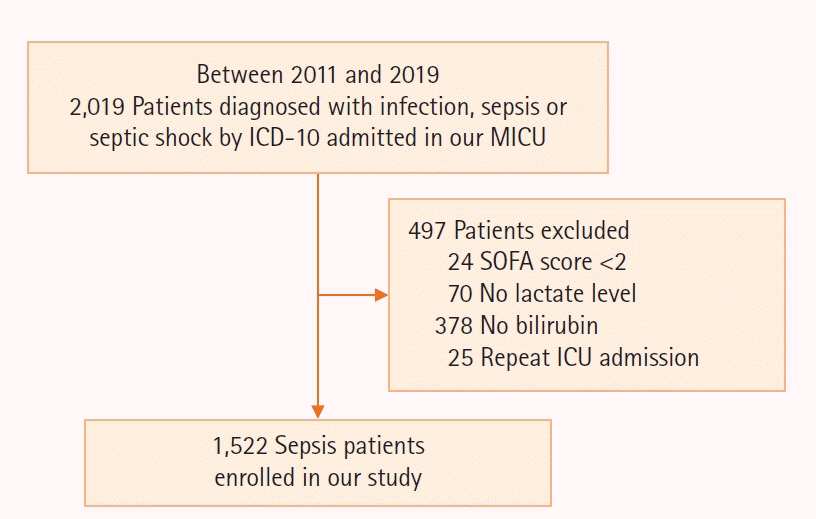
Methods
Sepsis patients admitted to the medical intensive care unit of Songklanagarind Hospital between 2011 and 2018 were retrospectively analyzed. The primary outcome was all-cause in-hospital mortality.
Results
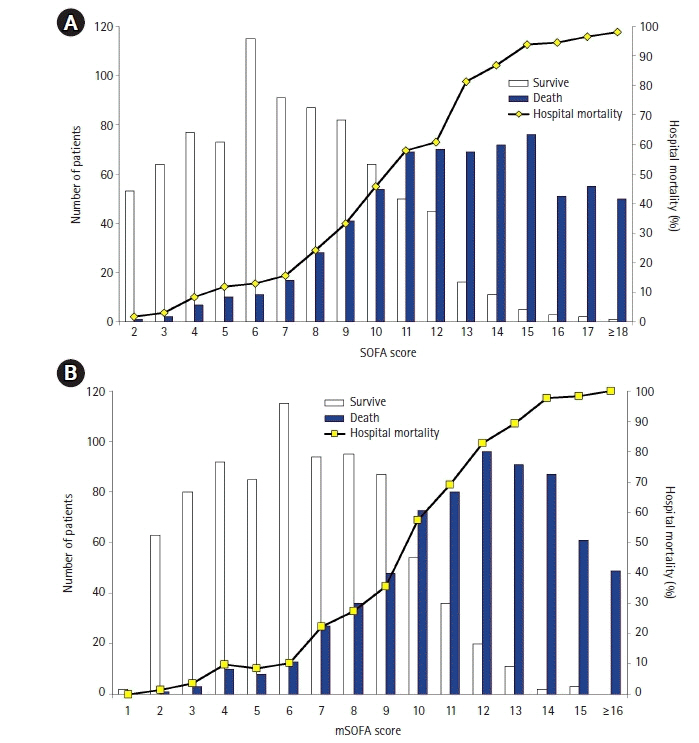
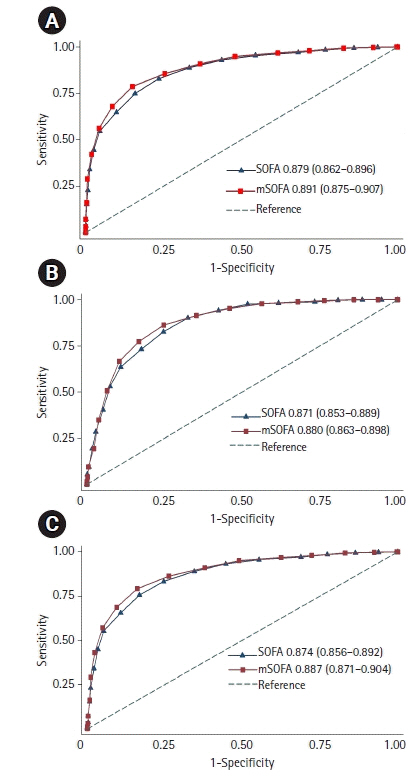
A total of 1,522 sepsis patients were enrolled. The mean SOFA and mSOFA scores were 9.7±4.3 and 8.8±3.9, respectively. The discrimination of the mSOFA score was significantly higher than that of the SOFA score for all-cause in-hospital mortality (area under the receiver operating characteristic curve, 0.891 [95% confidence interval, 0.875–0.907] vs. 0.879 [0.862–0.896]; P<0.001), all-cause intensive care unit (ICU) mortality (0.880 [0.863–0.898] vs. 0.871 [0.853–0.889], P=0.01) and all-cause 28-day mortality (0.887 [0.871–0.904] vs. 0.874 [0.856–0.892], P<0.001). The ability of mSOFA score to predict all-cause in-hospital and 28-day mortality was higher than that of the SOFA score within the subgroups of sepsis according to age, sepsis severity and serum lactate levels. The mSOFA score was demonstrated to have a performance similar to the original SOFA score regarding the prediction of mortality in sepsis patients with cirrhosis or hepatic dysfunction.
Conclusions
The mSOFA score was a good alternative to the original SOFA core in predicting mortality among sepsis patients admitted to the ICU.
Figure
Reference
-
1. Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet. 2020; 395:200–11.
Article2. Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing sepsis as a global health priority: a WHO resolution. N Engl J Med. 2017; 377:414–7.
Article3. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–10.
Article4. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.
Article5. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001; 286:1754–8.
Article6. Khwannimit B. A comparison of three organ dysfunction scores: MODS, SOFA and LOD for predicting ICU mortality in critically ill patients. J Med Assoc Thai. 2007; 90:1074–81.7. Khwannimit B, Bhurayanontachai R, Vattanavanit V. Comparison of the performance of SOFA, qSOFA and SIRS for predicting mortality and organ failure among sepsis patients admitted to the intensive care unit in a middle-income country. J Crit Care. 2018; 44:156–60.
Article8. Safari S, Shojaee M, Rahmati F, Barartloo A, Hahshemi B, Forouzanfar MM, et al. Accuracy of SOFA score in prediction of 30-day outcome of critically ill patients. Turk J Emerg Med. 2016; 16:146–50.
Article9. Williams JM, Greenslade JH, McKenzie JV, Chu K, Brown A, Lipman J. Systemic inflammatory response syndrome, quick sequential organ function assessment, and organ dysfunction: insights from a prospective database of ED patients with infection. Chest. 2017; 151:586–96.
Article10. Raymond NJ, Nguyen M, Allmark S, Woods L, Peckler B. Modified Sequential Organ Failure Assessment sepsis score in an emergency department setting: retrospective assessment of prognostic value. Emerg Med Australas. 2019; 31:339–46.
Article11. Sendagire C, Lipnick MS, Kizito S, Kruisselbrink R, Obua D, Ejoku J, et al. Feasibility of the modified sequential organ function assessment score in a resource-constrained setting: a prospective observational study. BMC Anesthesiol. 2017; 17:12.
Article12. Engel JM, Junger A, Bottger S, Benson M, Michel A, Rohrig R, et al. Outcome prediction in a surgical ICU using automatically calculated SAPS II scores. Anaesth Intensive Care. 2003; 31:548–54.
Article13. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–45.
Article14. Ray P, Le Manach Y, Riou B, Houle TT. Statistical evaluation of a biomarker. Anesthesiology. 2010; 112:1023–40.
Article15. Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017; 317:290–300.
Article16. Zhang Y, Luo H, Wang H, Zheng Z, Ooi OC. Validation of prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among cardiac-, thoracic-, and vascular-surgery patients admitted to a cardiothoracic intensive care unit. J Card Surg. 2020; 35:118–27.
Article17. Probst L, Schalk E, Liebregts T, Zeremski V, Tzalavras A, von Bergwelt-Baildon M, et al. Prognostic accuracy of SOFA, qSOFA and SIRS criteria in hematological cancer patients: a retrospective multicenter study. J Intensive Care. 2019; 7:41.
Article18. Basile-Filho A, Lago AF, Menegueti MG, Nicolini EA, Rodrigues L, Nunes RS, et al. The use of APACHE II, SOFA, SAPS 3, C-reactive protein/albumin ratio, and lactate to predict mortality of surgical critically ill patients: a retrospective cohort study. Medicine (Baltimore). 2019; 98:e16204.19. Breslow MJ, Badawi O. Severity scoring in the critically ill: part 1. Interpretation and accuracy of outcome prediction scoring systems. Chest. 2012; 141:245–52.20. Flaatten H, Walther S. Activity- or severity-based scoring in the ICU? Acta Anaesthesiol Scand. 2017; 61:2–4.
Article21. Baker T, Gerdin M. The clinical usefulness of prognostic prediction models in critical illness. Eur J Intern Med. 2017; 45:37–40.
Article22. Yadav H, Harrison AM, Hanson AC, Gajic O, Kor DJ, Cartin-Ceba R. Improving the accuracy of cardiovascular component of the sequential organ failure assessment score. Crit Care Med. 2015; 43:1449–57.
Article23. Vasilevskis EE, Pandharipande PP, Graves AJ, Shintani A, Tsuruta R, Ely EW, et al. Validity of a modified sequential organ failure assessment score using the Richmond Agitation-Sedation Scale. Crit Care Med. 2016; 44:138–46.
Article24. Kotani Y, Fujii T, Uchino S, Doi K; JAKID Study Group. Modification of sequential organ failure assessment score using acute kidney injury classification. J Crit Care. 2019; 51:198–203.
Article25. Grissom CK, Brown SM, Kuttler KG, Boltax JP, Jones J, Jephson AR, et al. A modified sequential organ failure assessment score for critical care triage. Disaster Med Public Health Prep. 2010; 4:277–84.
Article26. Rahmatinejad Z, Reihani H, Tohidinezhad F, Rahmatinejad F, Peyravi S, Pourmand A, et al. Predictive performance of the SOFA and mSOFA scoring systems for predicting in-hospital mortality in the emergency department. Am J Emerg Med. 2019; 37:1237–41.
Article27. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013; 39:165–228.
Article28. Levesque E, Hoti E, Azoulay D, Ichaï P, Habouchi H, Castaing D, et al. Prospective evaluation of the prognostic scores for cirrhotic patients admitted to an intensive care unit. J Hepatol. 2012; 56:95–102.
Article29. Zhao H, Gu X, Zhao R, Shi Y, Sheng J. Evaluation of prognostic scoring systems in liver cirrhosis patients with bloodstream infection. Medicine (Baltimore). 2017; 96:e8844.
Article30. Woźnica EA, Inglot M, Woźnica RK, Łysenko L. Liver dysfunction in sepsis. Adv Clin Exp Med. 2018; 27:547–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison of scoring systems for predicting mortality and sepsis in the emergency department patients with a suspected infection
- Circulating Biologically Active Adrenomedullin Predicts Organ Failure and Mortality in Sepsis
- Assessment of organ failure in sepsis patients in the emergency department: clinical evaluation, Sequential Organ Failure Assessment (SOFA) score, and future perspectives
- Quick Sepsis-related Organ Failure Assessment score is not sensitive enough to predict 28-day mortality in emergency department patients with sepsis: a retrospective review
- Proenkephalin Predicts Organ Failure, Renal Replacement Therapy, and Mortality in Patients With Sepsis