J Korean Med Sci.
2022 Oct;37(43):e316. 10.3346/jkms.2022.37.e316.
Production and Provision of ContextBased Patient-Specific Educational Resources
- Affiliations
-
- 1Department of Information Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Big Data Research Center, Asan Institute for Life Science, Asan Medical Center, Seoul, Korea
- KMID: 2534826
- DOI: http://doi.org/10.3346/jkms.2022.37.e316
Abstract
- Background
Patient education is generally accompanied by instructive materials. The Korean government has recommended the provision of patient-specific educational materials (PEMs) via an electronic medical record (EMR) certification system. However, there are currently no clear standards or guidelines for including PEMs in current domestic educational materials. We investigated the benefits of integrating PEMs with the EMR certification system and the methods by which this integration can be achieved.
Methods
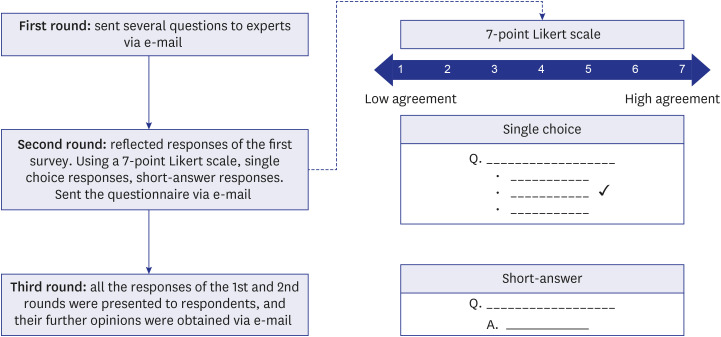
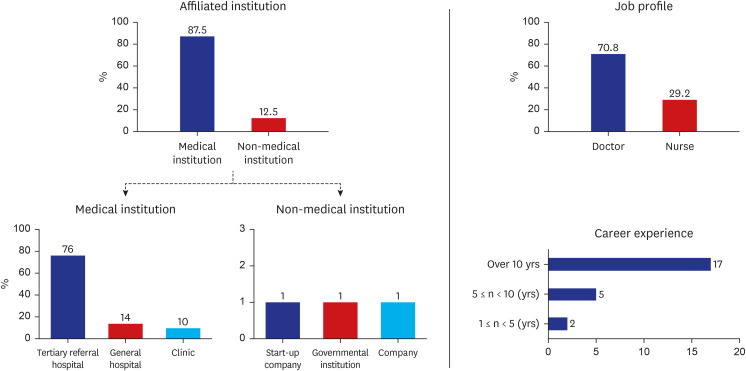
We developed and administered three structured Delphi surveys to 26 healthcare providers in clinical settings based on data collected from separate semi-structured advisory interviews with five experts. The surveys included the following topics: 1) expected effects of patient-specific education and health-related notifications/alarms, 2) desirable methods for providing PEMs, and 3) appropriate fee-setting and government support. We distributed the Delphi surveys via e-mail and calculated the average and standard deviation of the survey responses.
Results
PEMs are expected to have significant educational effects, such as the provision of surgery/intervention-related information, and will improve the understanding of various treatment processes/procedures. The preferred method for providing PEMs was via automatic request after receiving confirmation from healthcare providers. The provision of these materials was based on set fees and government support. The average fee per session was set at approximately USD 23 (as of October 2021, USD 1 = KRW 1,196).
Conclusion
In this study, we investigated the prerequisites, contents, methods, and fees related to the provision of effective and efficient PEMs. The study findings can facilitate the production and provision of PEMs.
Figure
Reference
-
1. Hill J. A practical guide to patient education and information giving. Baillieres Clin Rheumatol. 1997; 11(1):109–127. PMID: 9088528.2. Kitching JB. Patient information leaflets--the state of the art. J R Soc Med. 1990; 83(5):298–300. PMID: 2380944.3. Redman BK. The Practice of Patient Education. Maryland Heights, MS, USA: Mosby Inc.;2001.4. Ivnik M, Jett MY. Creating written patient education materials. Chest. 2008; 133(4):1038–1040. PMID: 18398128.5. Vignos PJ, Parker WT, Thompson HM. Evaluation of a clinic education program for patients with rheumatoid arthritis. J Rheumatol. 1976; 3(2):155–165. PMID: 950632.6. Boyd MD. A guide to writing effective patient education materials. Nurs Manage. 1987; 18(7):56–57.7. Jabbour J, Milross C, Sundaresan P, Ebrahimi A, Shepherd HL, Dhillon HM, et al. Education and support needs in patients with head and neck cancer: a multi-institutional survey. Cancer. 2017; 123(11):1949–1957. PMID: 28081302.8. Korea Health Information Service. Certification of EMR. Updated 2021. Accessed January 20, 2022. https://www.k-his.or.kr/menu.es?mid=a10201010100 .9. Korea Health Information Service. Guidance on the certification criteria for the electronic medical record system certification system (v1.1). Updated 2021. Accessed February 24, 2022. https://emrcert.mohw.go.kr/board.es?mid=a10606000000&bid=0005&list_no=403&act=view .10. Park HW, Min KU, Kim YY, Cho SH. Assessing the quality and contents of asthma-related information on the Korean internet as an educational material for patients. J Korean Med Sci. 2004; 19(3):364–368. PMID: 15201501.11. Office of the National Coordinator for Health Information Technology (US). §170.315 (a)(13) patient-specific education resources. Updated 2022. Accessed February 16, 2022. https://www.healthit.gov/test-method/patient-specific-education-resources .12. Falvo D. Effective Patient Education: A Guide to Increased Compliance. Burlington, MA, USA: Jones & Bartlett Learning;2004.13. Cohen GI. A practical guide to graphic communication for quality assurance, education, and patient care in echocardiography. Echocardiography. 2019; 36(9):1747–1754. PMID: 31541574.14. Gagnon JH, Greenblat CS. Health care planning and education via gaming-simulation: a two-stage experiment. Health Educ Monogr. 1977; 5(suppl 1):42–52. PMID: 858672.15. Marshall WR, Rothenberger LA, Bunnell SL. The efficacy of personalized audiovisual patient-education materials. J Fam Pract. 1984; 19(5):659–663. PMID: 6208312.16. Dicicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006; 40(4):314–321. PMID: 16573666.17. Sharif N. Utilizing the Delphi survey approach: a review. J Nurs Care. 2015; 4(3):246–251.18. Colton S, Hatcher T. The Web-Based Delphi Research Technique as a Method for Content Validation in HRD and Adult Education Research. In : Proceedings of Academy of Human Resource Development International Conference; 2004 Mar 3–7; Austin, TX, USA. St. Paul, MN, USA: Academy of Human Resource Development;2004. p. 183–189.19. Park HS, Lee SH, Shim JY, Cho JJ, Shin HC, Park JY. The physicians’ recognition and attitude about patient education in practice. J Korean Med Sci. 1996; 11(5):422–428. PMID: 8934398.20. Delbecq AL, Gustason DH, Van de Ven AH. Group Techniques for Program Planning: A Guide to Nominal Groups and Delphi Process. Northbrook, IL, USA: Scott Foresman;1975.21. Witkin BR, Altschuld JW. Planning and Conducting Needs Assessments: A Practical Guide. New York, NY, USA: SAGE Publications;1995.22. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007; 12:10.23. National Health Insurance Service (KR). Health security system. Updated 2015. 2022. https://www.nhis.or.kr/english/wbheaa02300m01.do .24. Hecht J. The future of electronic health records. Nature. 2019; 573(7775):S114–S116. PMID: 31554991.25. Hwang JI. Factors influencing consultation time and waiting time of ambulatory patients in a tertiary teaching hospital. J Korean Soc Qual Assur Health Care. 2006; 12(1):6–16.26. Aharonson-Daniel L, Paul RJ, Hedley AJ. Management of queues in out-patient departments: the use of computer simulation. J Manag Med. 1996; 10(6):50–58. PMID: 10538033.27. Park SH. Analysis of factors delaying on waiting time for medical examination of outpatient on a hospital. J Korean Soc Qual Assur Health Care. 2001; 8(1):56–72.28. Lee CH, Lim H, Kim Y, Park AH, Park EC, Kang JG. Analysis of appropriate outpatient consultation time for clinical departments. Health Policy Manag. 2014; 24(3):254–260.29. Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005; 12(5):505–516. PMID: 15905487.30. Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan WJ, Sinsky CA, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017; 15(5):419–426. PMID: 28893811.31. Gregory ME, Russo E, Singh H. Electronic health record alert-related workload as a predictor of burnout in primary care providers. Appl Clin Inform. 2017; 8(3):686–697. PMID: 28678892.32. Khairat S, Coleman C, Ottmar P, Bice T, Koppel R, Carson SS. Physicians’ gender and their use of electronic health records: findings from a mixed-methods usability study. J Am Med Inform Assoc. 2019; 26(12):1505–1514. PMID: 31504578.33. Muhiyaddin R, Elfadl A, Mohamed E, Shah Z, Alam T, Abd-Alrazaq A, et al. Electronic health records and physician burnout: a scoping review. Stud Health Technol Inform. 2022; 289:481–484. PMID: 35062195.34. Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the I3 population collaborative. J Grad Med Educ. 2017; 9(4):479–484. PMID: 28824762.35. Ministry of Health and Welfare (KR). The Pilot Project for Management Education Counseling Before and After Surgery. Sejong, Korea: Ministry of Health and Welfare;2018.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proposal of a linear rather than hierarchical evaluation of educational initiatives: the 7Is framework
- YouTube videos provide low-quality educational content about rotator cuff disease
- An expert consensus–based checklist for quality appraisal of educational resources on adult basic life support: a Delphi study
- What Education is Most Needed for Psychiatric Unit Nurses? Exploring its Specific Educational Needs: A Mixed Method Study
- Local Production of IgE in Nasal Polyp