J Yeungnam Med Sci.
2022 Oct;39(4):294-299. 10.12701/jyms.2021.01690.
Intensive care unit management of uncomplicated type B aortic dissection in relation to treatment period: a retrospective observational study
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2534656
- DOI: http://doi.org/10.12701/jyms.2021.01690
Abstract
- Background
Medical therapy is the standard treatment for uncomplicated acute type B aortic dissection (ATBAD), but there is little evidence of the need for intensive care unit (ICU) management. Therefore, we aimed to investigate the effects of ICU treatment on uncomplicated ATBAD.
Methods
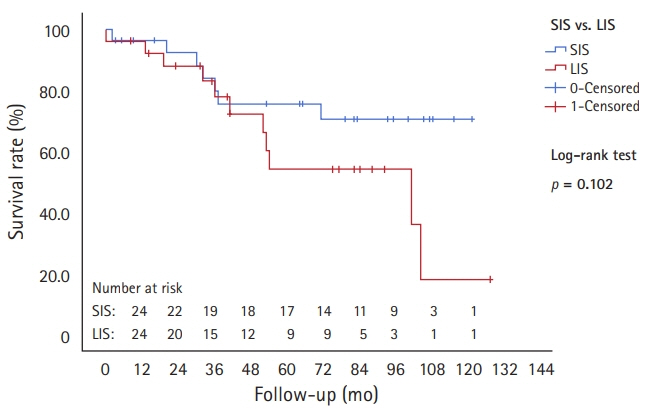
We retrospectively studied patients with uncomplicated ATBAD who were medically treated between January 2010 and July 2020. Patients were divided into long-term ICU stay (LIS) and short-term ICU stay (SIS) groups, according to a 48-hour cutoff of ICU stay duration. The incidence of pneumonia and delirium, rate of aortic events, hospital mortality, and survival rate were compared.
Results
Fifty-five patients were treated for uncomplicated ATBAD (n=26 for LIS and n=29 for SIS). The incidence of pneumonia (7.7% vs. 3.6%) and delirium (34.6% vs. 14.3%) was higher in the LIS group than in the SIS group, but the differences were not statistically significant. The survival rates at 1, 3, and 5 years were not different between the two groups (LIS: 96.2%, 88.0%, and 54.2% vs. SIS: 96.4%, 92.2%, and 75.5%, respectively; p=0.102). Multivariate Cox regression analysis for aortic events showed that using a calcium channel blocker lowered the risk of aortic events.
Conclusion
Long-term ICU treatment is unlikely to be necessary for the treatment of uncomplicated ATBAD. Active use of antihypertensive agents, such as calcium channel blockers, may be needed during the follow-up period.
Figure
Reference
-
References
1. Nienaber CA, Rousseau H, Eggebrecht H, Kische S, Fattori R, Rehders TC, et al. Randomized comparison of strategies for type B aortic dissection: the INvestigation of STEnt Grafts in Aortic Dissection (INSTEAD) trial. Circulation. 2009; 120:2519–28.
Article2. Nienaber CA, Kische S, Rousseau H, Eggebrecht H, Rehders TC, Kundt G, et al. Endovascular repair of type B aortic dissection: long-term results of the randomized investigation of stent grafts in aortic dissection trial. Circ Cardiovasc Interv. 2013; 6:407–16.
Article3. Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014; 35:2873–926.4. Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001; 27:1892–900.
Article5. Pieralli F, Vannucchi V, Mancini A, Grazzini M, Paolacci G, Morettini A, et al. Delirium is a predictor of in-hospital mortality in elderly patients with community acquired pneumonia. Intern Emerg Med. 2014; 9:195–200.
Article6. Lin SM, Huang CD, Liu CY, Lin HC, Wang CH, Huang PY, et al. Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. J Crit Care. 2008; 23:372–9.
Article7. Niino T, Hata M, Sezai A, Yoshitake I, Unosawa S, Shimura K, et al. Optimal clinical pathway for the patient with type B acute aortic dissection. Circ J. 2009; 73:264–8.
Article8. Heimrath OP, Buth KJ, Légaré JF. Long-term outcomes in patients requiring stay of more than 48 hours in the intensive care unit following coronary bypass surgery. J Crit Care. 2007; 22:153–8.
Article9. Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C. Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. Ann Thorac Surg. 2006; 81:880–5.
Article10. Bucerius J, Gummert JF, Walther T, Doll N, Falk V, Schmitt DV, et al. Predictors of prolonged ICU stay after on-pump versus off-pump coronary artery bypass grafting. Intensive Care Med. 2004; 30:88–95.
Article11. Wong DT, Cheng DC, Kustra R, Tibshirani R, Karski J, Carroll-Munro J, et al. Risk factors of delayed extubation, prolonged length of stay in the intensive care unit, and mortality in patients undergoing coronary artery bypass graft with fast-track cardiac anesthesia: a new cardiac risk score. Anesthesiology. 1999; 91:936–44.
Article12. Rossi-Foulkes R, Roman MJ, Rosen SE, Kramer-Fox R, Ehlers KH, O’Loughlin JE, et al. Phenotypic features and impact of beta blocker or calcium antagonist therapy on aortic lumen size in the Marfan syndrome. Am J Cardiol. 1999; 83:1364–8.
Article13. Halpern BL, Char F, Murdoch JL, Horton WB, McKusick VA. A prospectus on the prevention of aortic rupture in the Marfan syndrome with data on survivorship without treatment. Johns Hopkins Med J. 1971; 129:123–9.14. Salim MA, Alpert BS, Ward JC, Pyeritz RE. Effect of beta-adrenergic blockade on aortic root rate of dilation in the Marfan syndrome. Am J Cardiol. 1994; 74:629–33.
Article15. Shores J, Berger KR, Murphy EA, Pyeritz RE. Progression of aortic dilatation and the benefit of long-term beta-adrenergic blockade in Marfan’s syndrome. N Engl J Med. 1994; 330:1335–41.
Article16. Wheat MW Jr, Palmer RF, Bartley TD, Seelman RC. Treatment of dissecting aneurysms of the aorta without surgery. J Thorac Cardiovasc Surg. 1965; 50:364–73.
Article17. Genoni M, Paul M, Jenni R, Graves K, Seifert B, Turina M. Chronic beta-blocker therapy improves outcome and reduces treatment costs in chronic type B aortic dissection. Eur J Cardiothorac Surg. 2001; 19:606–10.18. Jonker FH, Trimarchi S, Rampoldi V, Patel HJ, O’Gara P, Peterson MD, et al. Aortic expansion after acute type B aortic dissection. Ann Thorac Surg. 2012; 94:1223–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aortic Dissection in a Survivor after Cardiopulmonary Resuscitation
- Stanford type A aortic dissection in a patient with Marfan syndrome during pregnancy: a case report
- Rare Cerebral Infarction in Patient with Type B Aortic Dissection
- Endovascular Treatment of Aortic Dissection due to Suture Line Dehiscence after Aortic Graft Replacement for Type A Aortic Dissection: A Report of Two Cases
- Impact of Neurointensivist Co-management on the Clinical Outcomes of Patients Admitted to a Neurosurgical Intensive Care Unit