Korean J Crit Care Med.
2017 May;32(2):218-222. 10.4266/kjccm.2016.00416.
Aortic Dissection in a Survivor after Cardiopulmonary Resuscitation
- Affiliations
-
- 1Division of Trauma and Surgical Critical Care, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. skhong94@amc.seoul.kr
- KMID: 2384048
- DOI: http://doi.org/10.4266/kjccm.2016.00416
Abstract
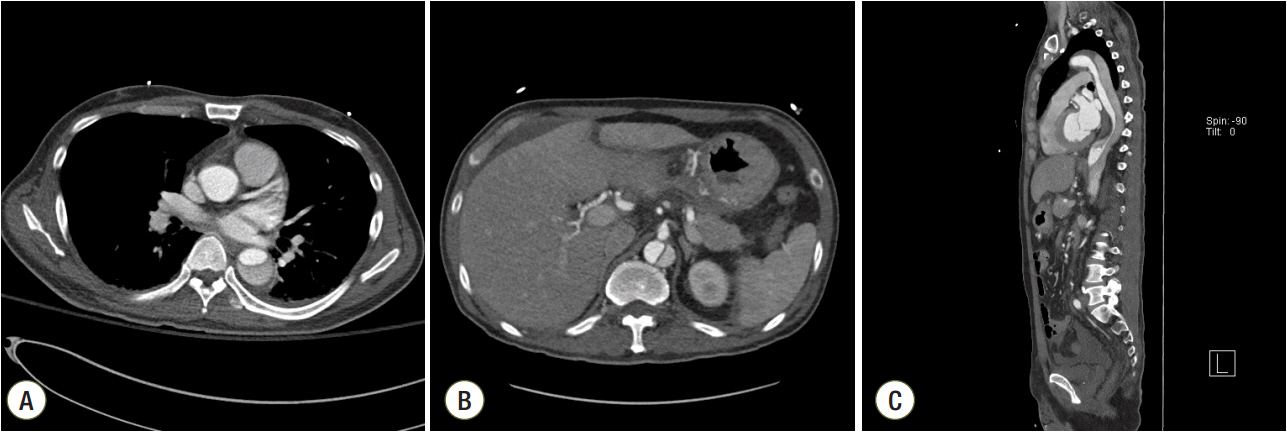
- We describe a case of traumatic aortic dissection associated with cardiac compression in a patient with anaphylactic cardiac arrest who underwent cardiopulmonary resuscitation (CPR). A 54-year-old man who was scheduled to undergo surgery for gastric cancer went into cardiac arrest caused by an anaphylactic reaction to prophylactic antibiotics in the operating room. Veno-arterial extracorporeal membrane oxygenation (ECMO) was performed. CPR, including chest compressions, was performed for 35 minutes, and the patient was transferred to the intensive care unit (ICU) after spontaneous circulation returned. The patient received ECMO for 9 hours until confirmation of normal cardiac function on transthoracic echocardiography. Twenty days after cardiac arrest, an aortic dissection and fractures in the left fourth and fifth ribs due to chest compression were detected by abdominal computed tomography. The DeBakey type III aortic dissection extended from the distal arch of the thoracic aorta to the proximal level of the renal artery, involving the celiac trunk. It was considered an uncomplicated type B aortic dissection with no sign of malperfusion of the major vessels. This case demonstrates the potential traumatic injuries that can occur after CPR and encourages proper management of mechanical complications in cardiac arrest survivors.
MeSH Terms
Figure
Reference
-
References
1. Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960; 173:1064–7.
Article2. Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nivhol G, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011; 39:2401–6.
Article3. Sandroni C, Nolan J, Cavallaro F, Antonelli M. Inhospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007; 33:237–45.
Article4. Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS, et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012; 367:1912–20.
Article5. Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008; 372:554–61.
Article6. Chung SY, Sheu JJ, Lin YJ, Sun CK, Chang LT, Chen YL, et al. Outcome of patients with profound cardiogenic shock after cardiopulmonary resuscitation and prompt extracorporeal membrane oxygenation support. A single-center observational study. Circ J. 2012; 76:1385–92.7. Wu MY, Lee MY, Lin CC, Chang YS, Tsai FC, Lin PJ. Resuscitation of non-postcardiotomy cardiogenic shock or cardiac arrest with extracorporeal life support: the role of bridging to intervention. Resuscitation. 2012; 83:976–81.
Article8. Buschmann CT, Tsokos M. Frequent and rare complications of resuscitation attempts. Intensive Care Med. 2009; 35:397–404.
Article9. Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. 2004; 63:327–38.
Article10. Sokolove PE, Willis-Shore J, Panacek EA. Exsanguination due to right ventricular rupture during closed-chest cardiopulmonary resuscitation. J Emerg Med. 2002; 23:161–4.
Article11. Herpain A, Vincent JL, De Backer D. Aortic luminal thrombus and intramural hematoma after cardiopulmonary resuscitation. Rev Bras Ter Intensiva. 2013; 25:345–7.
Article12. Oren-Grinberg A, Shahul S, Sarge T. Dissection of the thoracic aorta following cardiopulmonary resuscitation. Crit Ultrasound J. 2011; 3:25–7.
Article13. Univers J, Stevens S, Daley B. Aortic dissection after cardiopulmonary resuscitation. Am Surg. 2015; 81:E218–9.
Article14. Parmley LF, Mattinglly TW, Manion WC, Jahnke EJ Jr. Nonpenetrating traumatic injury of the aorta. Circulation. 1958; 17:1086–101.
Article15. Fabian TC, Davis KA, Gavant ML, Croce MA, Melton SM, Patton JH Jr, et al. Prospective study of blunt aortic injury: Multicenter Trial of the American Association for the Surgery of Trauma. J Trauma. 1997; 42:374–80.16. Fabian TC, Davis KA, Gavant ML, Croce MA, Melton SM, Patton JH Jr, et al. Prospective study of blunt aortic injury: helical CT is diagnostic and antihypertensive therapy reduces rupture. Ann Surg. 1998; 227:666–76.17. Konstadt SN, Reich DL, Quintana C, Levy M. The ascending aorta: how much does transesophageal echocardiography see? Anesth Analg. 1994; 78:240–4.18. Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122(18 Suppl 3):S685–705.19. Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest. 1987; 92:287–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aortic Dissection Following Cardiopulmonary Resuscitation
- Acute aortic dissection developed after cardiopulmonary resuscitation: transesophageal echocardiographic observations and proposed mechanism of injury
- Aortic dissection accompanied by preeclampsia in a postpartum young woman
- Retrograde Aortic Dissection during Ascending Aortic Aneurysm Surgery : A case report
- Perimortem Cesarean Delivery Following Severe Maternal Penetrating Injury