Endocrinol Metab.
2022 Oct;37(5):759-769. 10.3803/EnM.2022.1515.
Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 2Research Institute of The Way Healthcare, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Daegu Fatima Hospital, Daegu, Korea
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2534628
- DOI: http://doi.org/10.3803/EnM.2022.1515
Abstract
- Background
This study aimed to investigate the long-term effects of diabetes drug costs on cardiovascular (CV) events and death.
Methods
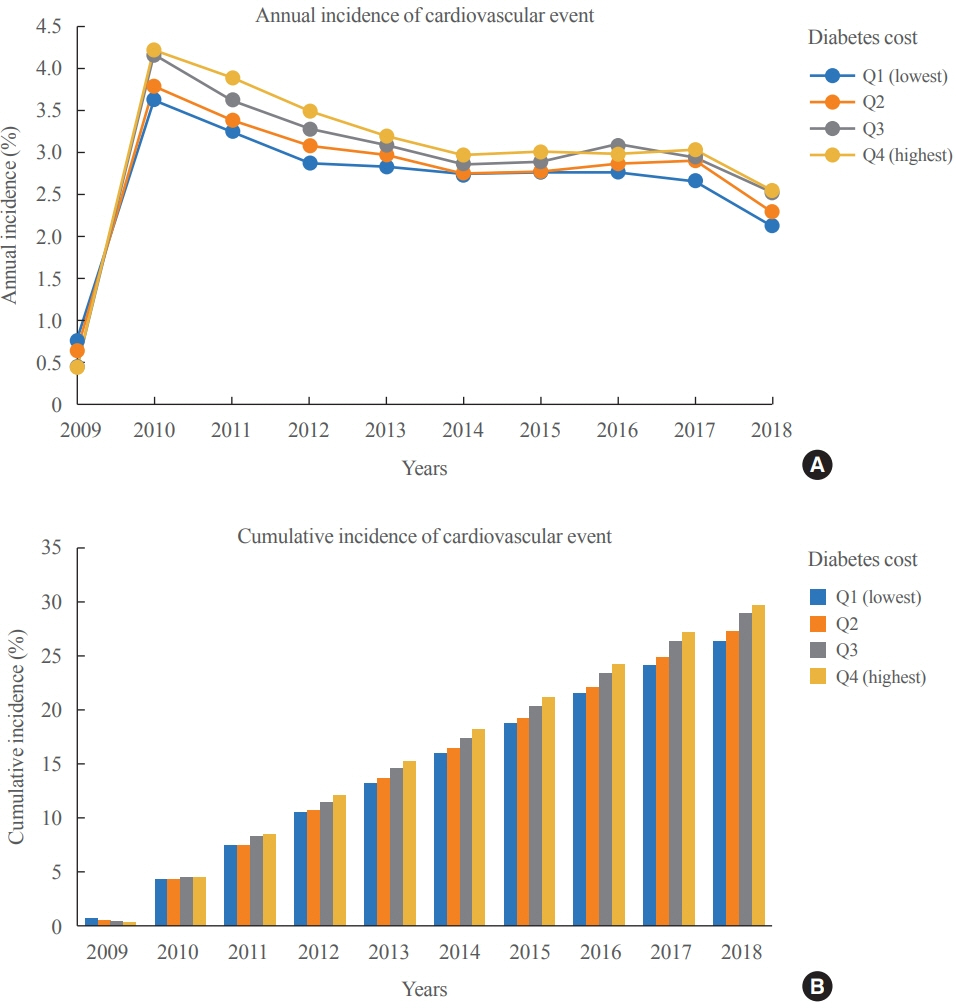
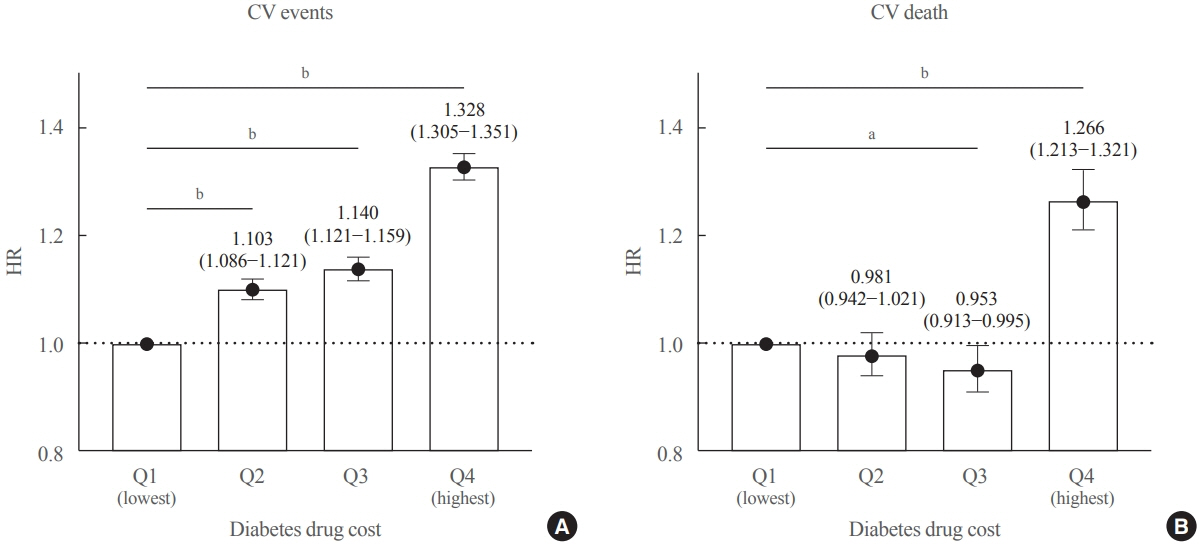
This retrospective observational study used data from 2009 to 2018 from the National Health Insurance in Korea. Among the patients with type 2 diabetes, those taking antidiabetic drugs and who did not have CV events until 2009 were included. Patients were divided into quartiles (Q1 [lowest]–4 [highest]) according to the 2009 diabetes drug cost. In addition, the 10-year incidences of CV events (non-fatal myocardial infarction, stroke, hospitalization for heart failure, and coronary revascularization) and CV death (death due to CV events) were analyzed.
Results
A total of 441,914 participants were enrolled (median age, 60 years; men, 57%). CV events and death occurred in 28.1% and 8.36% of the patients, respectively. The 10-year incidences of CV events and deaths increased from Q1 to 4. After adjusting for sex, age, income, type of diabetes drugs, comorbidities, and smoking and drinking status, the risk of CV events significantly increased according to the sequential order of the cost quartiles. In contrast, the risk of CV death showed a U-shaped pattern, which was the lowest in Q3 (hazard ratio [HR], 0.953; 95% confidence interval [CI], 0.913 to 0.995) and the highest in Q4 (HR, 1.266; 95% CI, 1.213 to 1.321).
Conclusion
Diabetes drug expenditure affects 10-year CV events and mortality. Therefore, affording an appropriate diabetes drug cost at a similar risk of CV is an independent protective factor against CV death.
Figure
Reference
-
1. International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: IDF;2019.2. International Diabetes Federation. IDF Diabetes Atlas. 4th ed. Brussels: IDF;2009.3. Saeedi P, Salpea P, Karuranga S, Petersohn I, Malanda B, Gregg EW, et al. Mortality attributable to diabetes in 20-79 years old adults, 2019 estimates: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2020; 162:108086.4. Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Barnighausen T, et al. The global economic burden of diabetes in adults aged 20-79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017; 5:423–30.
Article5. Sytkowski PA, Kannel WB, D’Agostino RB. Changes in risk factors and the decline in mortality from cardiovascular disease: the Framingham Heart Study. N Engl J Med. 1990; 322:1635–41.
Article6. Fitch K, Engel T, Sander S, Kuti E, Blumen H. Cardiovascular event incidence and cost in type 2 diabetes mellitus: a Medicare claims-based actuarial analysis. Curr Med Res Opin. 2017; 33:1795–801.
Article7. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020; 76:2982–3021.8. Riddle MC, Herman WH. The cost of diabetes care: an elephant in the room. Diabetes Care. 2018; 41:929–32.9. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.10. Hicks KA, Mahaffey KW, Mehran R, Nissen SE, Wiviott SD, Dunn B, et al. 2017 Cardiovascular and stroke endpoint definitions for clinical trials. Circulation. 2018; 137:961–72.
Article11. Jung CH, Chung JO, Han K, Ko SH, Ko KS, Park JY, et al. Improved trends in cardiovascular complications among subjects with type 2 diabetes in Korea: a nationwide study (2006-2013). Cardiovasc Diabetol. 2017; 16:1.
Article12. Rawshani A, Rawshani A, Franzen S, Eliasson B, Svensson AM, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017; 376:1407–18.
Article13. Park JH, Ha KH, Kim BY, Lee JH, Kim DJ. Trends in cardiovascular complications and mortality among patients with diabetes in South Korea. Diabetes Metab J. 2021; 45:120–4.
Article14. Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee SJ, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015; 30:251–77.
Article15. Williams R, Van Gaal L, Lucioni C; CODE-2 Advisory Board. Assessing the impact of complications on the costs of type II diabetes. Diabetologia. 2002; 45:S13–7.
Article16. Li R, Zhang P, Barker LE, Chowdhury FM, Zhang X. Costeffectiveness of interventions to prevent and control diabetes mellitus: a systematic review. Diabetes Care. 2010; 33:1872–94.
Article17. Alzaid A, Ladron de Guevara P, Beillat M, Lehner Martin V, Atanasov P. Burden of disease and costs associated with type 2 diabetes in emerging and established markets: systematic review analyses. Expert Rev Pharmacoecon Outcomes Res. 2021; 21:785–98.
Article18. Marcellusi A, Viti R, Sciattella P, Aimaretti G, De Cosmo S, Provenzano V, et al. Economic aspects in the management of diabetes in Italy. BMJ Open Diabetes Res Care. 2016; 4:e000197.
Article19. Jiao FF, Fung CS, Wan EY, Chan AK, McGhee SM, Kwok RL, et al. Five-year cost-effectiveness of the multidisciplinary risk assessment and management programme-diabetes mellitus (RAMP-DM). Diabetes Care. 2018; 41:250–7.
Article20. Herman ME, O’Keefe JH, Bell DS, Schwartz SS. Insulin therapy increases cardiovascular risk in type 2 diabetes. Prog Cardiovasc Dis. 2017; 60:422–34.
Article21. Funamizu T, Iwata H, Nishida Y, Miyosawa K, Doi S, Chikata Y, et al. Increased risk of cardiovascular mortality by strict glycemic control (pre-procedural HbA1c < 6.5%) in Japanese medically-treated diabetic patients following percutaneous coronary intervention: a 10-year follow-up study. Cardiovasc Diabetol. 2020; 19:21.22. Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, et al. Survival as a function of HbA(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010; 375:481–9.
Article23. Beran D, Ewen M, Lipska K, Hirsch IB, Yudkin JS. Availability and affordability of essential medicines: implications for global diabetes treatment. Curr Diab Rep. 2018; 18:48.
Article24. Afroz A, Alramadan MJ, Hossain MN, Romero L, Alam K, Magliano DJ, et al. Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: a systematic review. BMC Health Serv Res. 2018; 18:972.
Article25. Chow CK, Ramasundarahettige C, Hu W, AlHabib KF, Avezum A Jr, Cheng X, et al. Availability and affordability of essential medicines for diabetes across high-income, middle-income, and low-income countries: a prospective epidemiological study. Lancet Diabetes Endocrinol. 2018; 6:798–808.
Article26. Khatib R, McKee M, Shannon H, Chow C, Rangarajan S, Teo K, et al. Availability and affordability of cardiovascular disease medicines and their effect on use in high-income, middle-income, and low-income countries: an analysis of the PURE study data. Lancet. 2016; 387:61–9.
Article27. Baek JH, Yang YS, Ko SH, Han KD, Kim JH, Moon MK, et al. Real-world prescription patterns and barriers related to the use of sodium-glucose cotransporter 2 inhibitors among Korean patients with type 2 diabetes mellitus and cardiovascular disease. Diabetes Metab J. 2022; 46:701–12.
Article28. von Ferber L, Koster I, Hauner H. Medical costs of diabetic complications total costs and excess costs by age and type of treatment results of the German CoDiM Study. Exp Clin Endocrinol Diabetes. 2007; 115:97–104.
Article29. Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013; 45:253–61.
Article30. Nathan D. Results of the Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness (GRADE) Study [Internet]. Arlington: American Diabetes Association;2021. [cited 2022 Sep 7]. Available from: https://www.adameetingnews.org/live-updates/session-coverage/results-fromfirst-head-to-head-trial-of-four-type-2-diabetes-agents-tobe-presented/.31. Korean Diabetes Association. Diabetes Fact Sheet in Korea 2018 [Internet]. Seoul: Korean Diabetes Association;2018. [cited 2022 Sep 7]. Available from: https://www.diabetes.or.kr/bbs/?code=fact_sheet&mode=view&number=1666&page=1&code=fact_sheet.32. Park SJ, Ha KH, Kim DJ. Body mass index and cardiovascular outcomes in patients with acute coronary syndrome by diabetes status: the obesity paradox in a Korean national cohort study. Cardiovasc Diabetol. 2020; 19:191.
Article33. Pagidipati NJ, Zheng Y, Green JB, McGuire DK, Mentz RJ, Shah S, et al. Association of obesity with cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease: insights from TECOS. Am Heart J. 2020; 219:47–57.
Article34. Velavan P, Huan Loh P, Clark A, Cleland JG. The cholesterol paradox in heart failure. Congest Heart Fail. 2007; 13:336–41.
Article35. Lee YB, Koo M, Noh E, Hwang SY, Kim JA, Roh E, et al. Myocardial infarction, stroke, and all-cause mortality according to low-density lipoprotein cholesterol level in the elderly, a nationwide study. Diabetes Metab J. 2022; 46:722–32.
Article36. Ko SH, Han K, Lee YH, Noh J, Park CY, Kim DJ, et al. Past and current status of adult type 2 diabetes mellitus management in Korea: a National Health Insurance Service database analysis. Diabetes Metab J. 2018; 42:93–100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Study Using Healthcare Claims Database
- Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
- Introducing big data analysis using data from National Health Insurance Service
- Data Analytic Process of a Nationwide Population-Based Study Using National Health Information Database Established by National Health Insurance Service
- Uric Acid and Risk of Cardiovascular Disease and Mortality: A Longitudinal Cohort Study