J Korean Med Sci.
2022 Oct;37(41):e294. 10.3346/jkms.2022.37.e294.
Outcomes of Patients on the Lung Transplantation Waitlist in Korea: A Korean Network for Organ Sharing Data Analysis
- Affiliations
-
- 1Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Division of Allergy, Pulmonary and Critical Care Medicine, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea
- 3Department of Pulmonary and Critical Care Medicine, Asan Medical Center, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Ajou University School of Medicine, Suwon, Korea
- 5Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 6Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Interdisciplinary Program of Genomic Science, Pusan National University, Yangsan, Korea
- 8Department of Nuclear Medicine and Pusan National University Medical Research Institute, Pusan National University Hospital, Busan, Korea
- 9Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea
- 10Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2534459
- DOI: http://doi.org/10.3346/jkms.2022.37.e294
Abstract
- Background
The demand for lung transplants continues to increase in Korea, and donor shortages and waitlist mortality are critical issues. This study aimed to evaluate the factors that affect waitlist outcomes from the time of registration for lung transplantation in Korea.
Methods
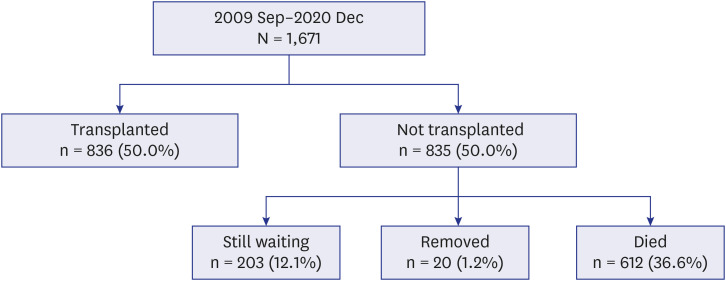
Data were obtained from the Korean Network for Organ Sharing for lung-only registrations between September 7, 2009, and December 31, 2020. Post-registration outcomes were evaluated according to the lung disease category, blood group, and age.
Results
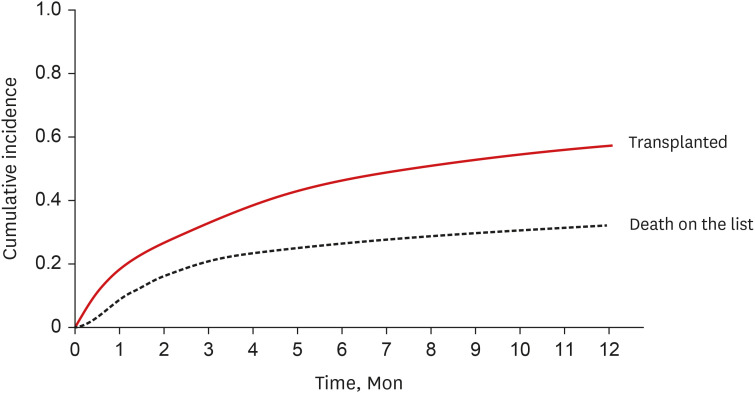
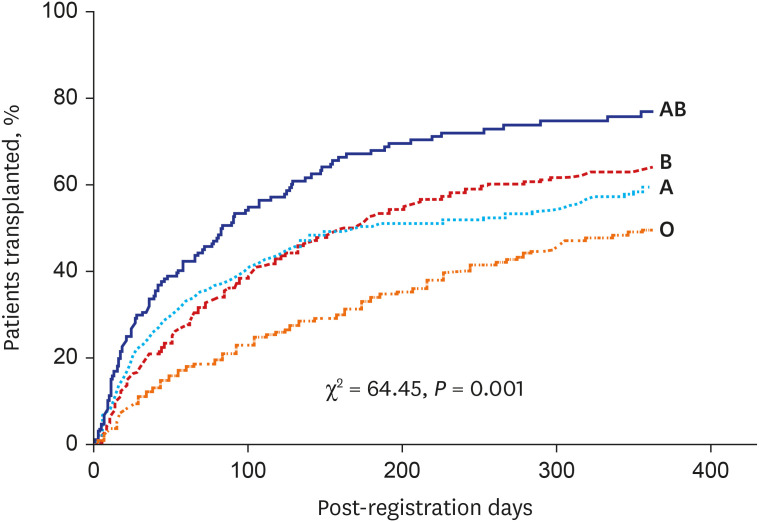
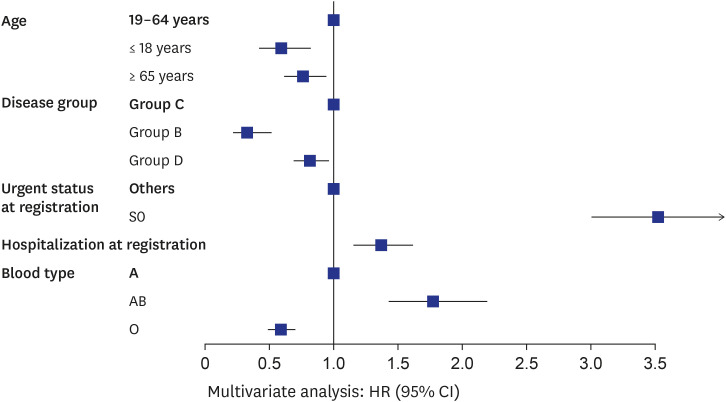
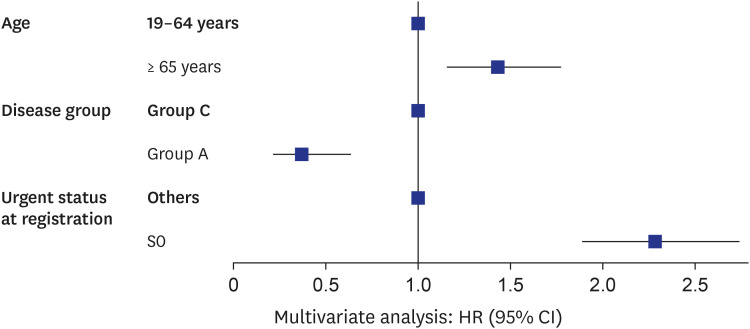
Among the 1,671 registered patients, 49.1% had idiopathic pulmonary fibrosis (group C), 37.0% had acute respiratory distress syndrome and other interstitial lung diseases (group D), 7.2% had chronic obstructive pulmonary disease (group A), and 6.6% had primary pulmonary hypertension (group B). Approximately half of the patients (46.1%) were transplanted within 1 year of registration, while 31.8% died without receiving a lung transplant within 1 year of registration. Data from 1,611 patients were used to analyze 1-year postregistration outcomes, which were classified as transplanted (46.1%, n = 743), still awaiting (21.1%, n = 340), removed (0.9%, n = 15), and death on waitlist (31.8%, n = 513). No significant difference was found in the transplantation rate according to the year of registration. However, significant differences occurred between the waitlist mortality rates (P = 0.008) and the still awaiting rates (P = 0.009). The chance of transplantation after listing varies depending on the disease category, blood type, age, and urgency status. Waitlist mortality within 1 year was significantly associated with non-group A disease (hazard ratio [HR], 2.76, P < 0.001), age ≥ 65 years (HR, 1.48, P < 0.001), and status 0 at registration (HR, 2.10, P < 0.001).
Conclusion
Waitlist mortality is still higher in Korea than in other countries. Future revisions to the lung allocation system should take into consideration the high waitlist mortality and donor shortages.
Keyword
Figure
Cited by 1 articles
-
Patient management for thoracic organ donor candidates: the lung transplantation team’s view
Hye Ju Yeo
Clin Transplant Res. 2024;38(1):18-22. doi: 10.4285/kjt.23.0062.
Reference
-
1. Lee JG, Park MS, Jeong SJ, Kim SY, Na S, Kim J, et al. Critical care before lung transplantation. Acute Crit Care. 2018; 33(4):197–205. PMID: 31723886.2. Korean Network for Organ Sharing. Annual report of the transplant 2019. Updated 2020. Accessed February 2022. https://www.konos.go.kr/board/boardListPage.do?page=sub4_2_1&boardId=30 .3. Yeo HJ, Yoon SH, Lee SE, Jeon D, Kim YS, Cho WH, et al. Current status and future of lung donation in Korea. J Korean Med Sci. 2017; 32(12):1953–1958. PMID: 29115076.
Article4. Egan TM, Murray S, Bustami RT, Shearon TH, McCullough KP, Edwards LB, et al. Development of the new lung allocation system in the United States. Am J Transplant. 2006; 6(5 Pt 2):1212–1227. PMID: 16613597.
Article5. Yeung JC, Keshavjee S. Overview of clinical lung transplantation. Cold Spring Harb Perspect Med. 2014; 4(1):a015628. PMID: 24384816.
Article6. Kotloff RM, Thabut G. Lung transplantation. Am J Respir Crit Care Med. 2011; 184(2):159–171. PMID: 21471083.
Article7. Ladin K, Hanto DW. Rationing lung transplants--procedural fairness in allocation and appeals. N Engl J Med. 2013; 369(7):599–601. PMID: 23883330.
Article8. Benvenuto LJ, Arcasoy SM. The new allocation era and policy. J Thorac Dis. 2021; 13(11):6504–6513. PMID: 34992830.9. Yu WS, Kim SY, Kim YT, Lee HJ, Park S, Choi SM, et al. Characteristics of lung allocation and outcomes of lung transplant according to the Korean urgency status. Yonsei Med J. 2019; 60(10):992–997. PMID: 31538435.10. Yeo HJ, Kim DH, Kim YS, Jeon D, Cho WH. Performance changes following the revision of organ allocation system of lung transplant: analysis of Korean Network for Organ Sharing data. J Korean Med Sci. 2021; 36(12):e79. PMID: 33783144.11. Keeshan BC, Rossano JW, Beck N, Hammond R, Kreindler J, Spray TL, et al. Lung transplant waitlist mortality: height as a predictor of poor outcomes. Pediatr Transplant. 2015; 19(3):294–300. PMID: 25406495.12. Kourliouros A, Hogg R, Mehew J, Al-Aloul M, Carby M, Lordan JL, et al. Patient outcomes from time of listing for lung transplantation in the UK: are there disease-specific differences? Thorax. 2019; 74(1):60–68. PMID: 30282722.13. Hirama T, Akiba M, Watanabe T, Watanabe Y, Notsuda H, Oishi H, et al. Waiting time and mortality rate on lung transplant candidates in Japan: a single-center retrospective cohort study. BMC Pulm Med. 2021; 21(1):390. PMID: 34844592.
Article14. Nie JB, Jones DG. Confucianism and organ donation: moral duties from xiao (filial piety) to ren (humaneness). Med Health Care Philos. 2019; 22(4):583–591. PMID: 30903406.
Article15. Antoine C. Organ allocation system: between efficiency and equity. Rev Prat. 2007; 57(3):262–268. PMID: 17578026.16. Ainge-Allen HW, Glanville AR. Timing it right: the challenge of recipient selection for lung transplantation. Ann Transl Med. 2020; 8(6):408. PMID: 32355852.
Article17. Christie JD, Edwards LB, Kucheryavaya AY, Aurora P, Dobbels F, Kirk R, et al. The registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult lung and heart-lung transplant report--2010. J Heart Lung Transplant. 2010; 29(10):1104–1118. PMID: 20870165.18. Cardiothoracic Advisory Group (CTAG) on behalf of NHSBT. Donor lung distribution and allocation. Updated 2017. Accessed February 24, 2022. http://odt.nhs.uk/pdf/lung_allocation_policy.pdf .19. Valapour M, Lehr CJ, Skeans MA, Smith JM, Miller E, Goff R, et al. OPTN/SRTR 2019 annual data report: lung. Am J Transplant. 2021; 21(Suppl 2):441–520. PMID: 33595190.20. Lee SH, Yeo Y, Kim TH, Lee HL, Lee JH, Park YB, et al. Korean guidelines for diagnosis and management of interstitial lung diseases: part 2. idiopathic pulmonary fibrosis. Tuberc Respir Dis. 2019; 82(2):102–117.21. Jegal Y, Park JS, Kim SY, Yoo H, Jeong SH, Song JW, et al. Clinical features, diagnosis, management, and outcomes of idiopathic pulmonary fibrosis in Korea: analysis of the Korea IPF Cohort (KICO) registry. Tuberc Respir Dis. 2022; 85(2):185–194.22. Rhee CK. It is time to consider human leukocyte antigen compatibility in lung transplantation. J Korean Med Sci. 2022; 37(22):e187. PMID: 35668691.23. Kim HE, Yang YH, Paik HC, Jeong SJ, Kim SY, Park MS, et al. The assessment and outcomes of crossmatching in lung transplantation in Korean patients. J Korean Med Sci. 2022; 37(22):e177. PMID: 35668687.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predicted Impact of the Model for End-Stage Liver Disease 3.0 in a Region Suffering Severe Organ Shortage
- Performance changes following the revision of organ allocation system of lung transplant: analysis of Korean Network for Organ Sharing (KONOS) data
- Current Status of Deceased Donor Organ Recovery and Sharing in Korea
- Current status and characteristics of lung transplantation for elderly people in Korea: analysis of Korean Network for Organ Sharing Data
- Development of Korean lung allocation system using machine learning