J Korean Diabetes.
2022 Sep;23(3):157-164. 10.4093/jkd.2022.23.3.157.
Maturity-Onset Diabetes of the Young (MODY)
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2534301
- DOI: http://doi.org/10.4093/jkd.2022.23.3.157
Abstract
- Precision medicine, which optimizes diagnosis and treatment of diseases according to individualized characteristics, is becoming a reality in the field of diabetes, especially for monogenic diabetes. Maturityonset diabetes of the young (MODY) is a type of monogenic diabetes characterized by early onset, relative non-obesity, non-insulin dependence, and autosomal dominant inheritance. With the trend toward precision medicine and improvement in genetic testing, there have been advances in the classification, diagnosis, and treatment of MODY. MODY accounts for about 1% of diabetes in Korea, with GCK (glucokinase)-MODY, HNF1α (hepatocyte nuclear factor-1 alpha)-MODY, and HNF4α (hepatocyte nuclear factor-4 alpha)-MODY being most common. In the diagnosis of MODY, applying guidelines for interpretation of variant pathogenicity is important. For the treatment of MODY, individualized treatment strategies according to the causative gene of MODY should be applied when available. Still, the majority of MODY is misdiagnosed and more genetic testing is required in Korea. We review updates regarding the classification, diagnosis, and treatment of MODY.
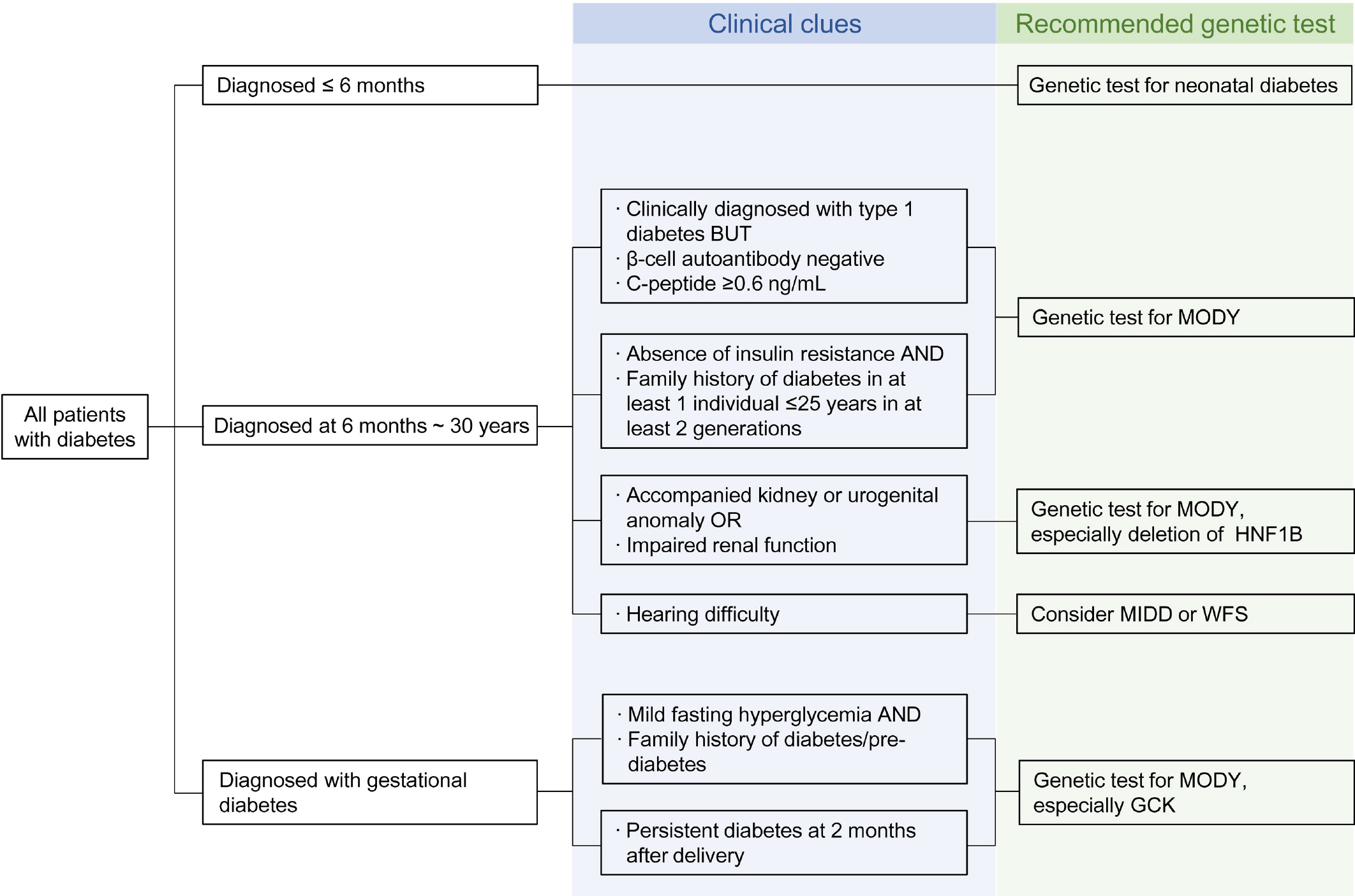
Figure
Reference
-
1.Shepherd M., Shields B., Hammersley S., Hudson M., McDonald TJ., Colclough K, et al. Systematic population screening, using biomarkers and genetic testing, identi-fies 2.5% of the U.K. pediatric diabetes population with monogenic diabetes. Diabetes Care. 2016. 39:1879–88.
Article2.Tattersall RB., Fajans SS. A difference between the inheritance of classical juvenile-onset and maturity-onset type diabetes of young people. Diabetes. 1975. 24:44–53.
Article3.Laver TW., Wakeling MN., Knox O., Colclough K., Wright CF., Ellard S, et al. Evaluation of evidence for pathogenicity demonstrates that BLK, KLF11, and PAX4 should not be included in diagnostic testing for MODY. Diabetes. 2022. 71:1128–36.
Article4.Zhang H., Colclough K., Gloyn AL., Pollin TI. Monogenic diabetes: a gateway to precision medicine in diabetes. J Clin Invest. 2021. 131:e142244.
Article5.Galler A., Stange T., Müller G., Näke A., Vogel C., Kapellen T, et al. Incidence of childhood diabetes in children aged less than 15 years and its clinical and metabolic characteristics at the time of diagnosis: data from the Childhood Diabetes Registry of Saxony, Germany. Horm Res Paediatr. 2010. 74:285–91.
Article6.Pihoker C., Gilliam LK., Ellard S., Dabelea D., Davis C., Dolan LM, et al. Prevalence, characteristics and clinical diagnosis of maturity onset diabetes of the young due to mutations in HNF1A, HNF4A, and glucokinase: results from the SEARCH for Diabetes in Youth. J Clin Endocrinol Metab. 2013. 98:4055–62.
Article7.Kleinberger JW., Pollin TI. Undiagnosed MODY: time for action. Curr Diab Rep. 2015. 15:110.
Article8.Park SS., Jang SS., Ahn CH., Kim JH., Jung HS., Cho YM, et al. Identifying pathogenic variants of monogenic diabetes using targeted panel sequencing in an East Asian population. J Clin Endocrinol Metab. 2019. 104:4188–98.
Article9.Shields BM., Hicks S., Shepherd MH., Colclough K., Hattersley AT., Ellard S. Maturity-onset diabetes of the young (MODY): how many cases are we missing? Diabetologia. 2010. 53:2504–8.
Article10.Sagen JV., Odili S., Bjørkhaug L., Zelent D., Buettger C., Kwagh J, et al. From clinicogenetic studies of maturity-on-set diabetes of the young to unraveling complex mecha-nisms of glucokinase regulation. Diabetes. 2006. 55:1713–22.
Article11.Edghill EL., Stals K., Oram RA., Shepherd MH., Hattersley AT., Ellard S. HNF1B deletions in patients with young-on-set diabetes but no known renal disease. Diabet Med. 2013. 30:114–7.12.Rafiq M., Flanagan SE., Patch AM., Shields BM., Ellard S., Hattersley AT. Effective treatment with oral sulfonylureas in patients with diabetes due to sulfonylurea receptor 1 (SUR1) mutations. Diabetes Care. 2008. 31:204–9.
Article13.Yahaya TO., Ufuoma SB. Genetics and pathophysiology of maturity-onset diabetes of the young (MODY): a review of current trends. Oman Med J. 2020. 35:e126.
Article14.Flanagan SE., Patch AM., Mackay DJ., Edghill EL., Gloyn AL., Robinson D, et al. Mutations in ATP-sensitive K+ channel genes cause transient neonatal diabetes and permanent diabetes in childhood or adulthood. Diabetes. 2007. 56:1930–7. Erratum in: Diabetes 2008;57):523.
Article15.Urano F. Wolfram syndrome: diagnosis, management, and treatment. Curr Diab Rep. 2016. 16:6.
Article16.Vaxillaire M., Froguel P. Monogenic diabetes in the young, pharmacogenetics and relevance to multifactorial forms of type 2 diabetes. Endocr Rev. 2008. 29:254–64.
Article17.Shields BM., McDonald TJ., Ellard S., Campbell MJ., Hyde C., Hattersley AT. The development and validation of a clinical prediction model to determine the probability of MODY in patients with young-onset diabetes. Diabetologia. 2012. 55:1265–72.
Article18.Yang YS., Kwak SH., Park KS. Update on monogenic diabetes in Korea. Diabetes Metab J. 2020. 44:627–39.
Article19.Li MM., Datto M., Duncavage EJ., Kulkarni S., Lindeman NI., Roy S, et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017. 19:4–23.
Article20.Zhang H., Maloney KA., Barbetti F., Greeley SAW., Ket-tunen JLT., Miranda JP, et al. 1453-P: Adaption of the ACMG/AMP variant interpretation guidelines for GCK, HNF1A, HNF4A-MODY: recommendations from the ClinGen Monogenic Diabetes Expert Panel. Diabetes. 2020. 69(Supplement_1):1453–P.
Article21.Santana LS., Caetano LA., Costa-Riquetto AD., Quedas EPS., Nery M., Collett-Solberg P, et al. Clinical application of ACMG-AMP guidelines in HNF1A and GCK variants in a cohort of MODY families. Clin Genet. 2017. 92:388–96.
Article22.Stride A., Vaxillaire M., Tuomi T., Barbetti F., Njølstad PR., Hansen T, et al. The genetic abnormality in the beta cell determines the response to an oral glucose load. Diabetologia. 2002. 45:427–35.
Article23.Pearson ER., Starkey BJ., Powell RJ., Gribble FM., Clark PM., Hattersley AT. Genetic cause of hyperglycaemia and response to treatment in diabetes. Lancet. 2003. 362:1275–81.
Article24.Østoft SH., Bagger JI., Hansen T., Pedersen O., Faber J., Holst JJ, et al. Glucose-lowering effects and low risk of hypoglycemia in patients with maturity-onset diabetes of the young when treated with a GLP-1 receptor agonist: a double-blind, randomized, crossover trial. Diabetes Care. 2014. 37:1797–805.
Article25.Ellard S., Beards F., Allen LI., Shepherd M., Ballantyne E., Harvey R, et al. A high prevalence of glucokinase mutations in gestational diabetic subjects selected by clinical criteria. Diabetologia. 2000. 43:250–3.
Article26.Spyer G., Macleod KM., Shepherd M., Ellard S., Hattersley AT. Pregnancy outcome in patients with raised blood glucose due to a heterozygous glucokinase gene mutation. Diabet Med. 2009. 26:14–8.
Article27.Kwak SH., Powe CE., Jang SS., Callahan MJ., Bernstein SN., Lee SM, et al. Sequencing cell-free fetal DNA in pregnant women with GCK-MODY: a proof-of-concept study. J Clin Endocrinol Metab. 2021. 106:2678–89.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maturity-onset diabetes of the young: update and perspectives on diagnosis and treatment
- MODY Syndrome
- Maturity-Onset Diabetes of the Young: What Do Clinicians Need to Know?
- A rare, likely pathogenic GCK variant related to maturity-onset diabetes of the young type 2: A case report
- Identification of Maturity-Onset Diabetes of the Young Caused by Glucokinase Mutations Detected Using Whole-Exome Sequencing