Korean J Transplant.
2022 Sep;36(3):226-230. 10.4285/kjt.22.0021.
Primary non-function in a deceased donor kidney transplant even with a Kidney Donor Risk Index less than 1.0: a case report
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Surgery, Seoul Medical Center, Seoul, Korea
- KMID: 2533961
- DOI: http://doi.org/10.4285/kjt.22.0021
Abstract
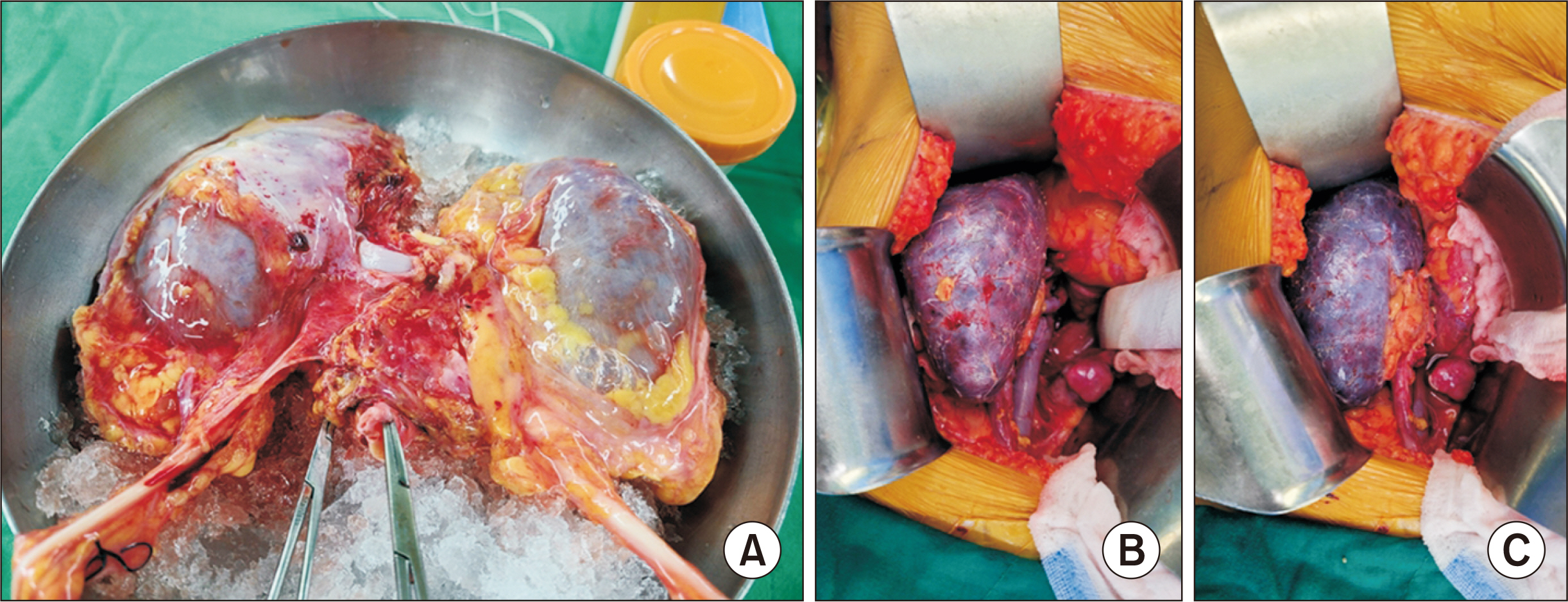
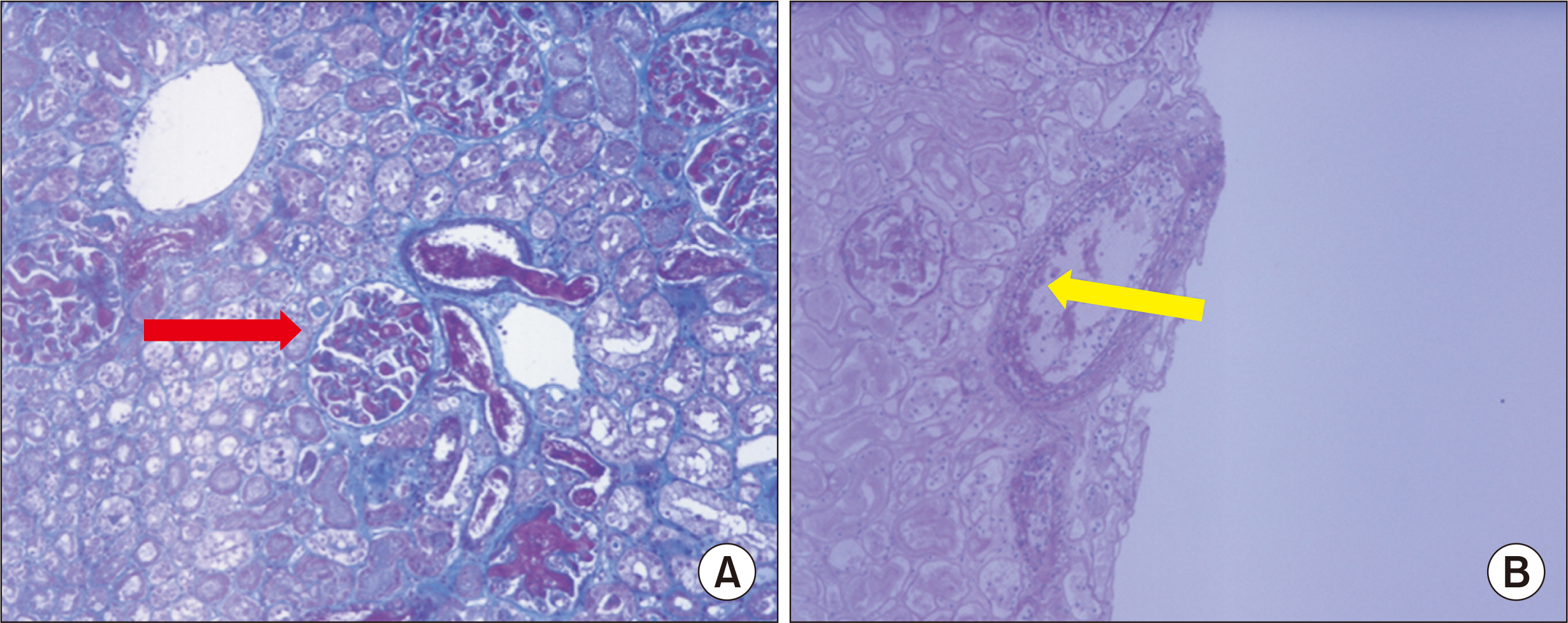
- Donations from deceased donors have been increasing since the introduction of ex- panded criteria for donor kidney selection. Several studies have shown that patients receiving deceased donor kidneys using these expanded criteria have improved survival compared to those remaining on the waiting list during hemodialysis. It is important, however, to consider that some of the kidneys classed as usable under the expanded criteria may in fact be unacceptable. To address this concern, preoperative biopsy and imaging of deceased donor kidneys are increasingly being used to assess candidate kidneys. We present the case of a 44-year-old female patient who underwent deceased donor kidney transplantation with negative complement-dependent cytotoxicity and flow cytometry crossmatch. Hours after graft reperfusion, given clinical evidence of primary nonfunction in the kidney, the patient underwent nephrectomy. Despite negative tests for blood type difference and crossmatch, and although the main artery and vein were well perfused, the kidney graft was never functional, and pathologic findings showed thrombotic microangiopathy and diffuse acute tubular necrosis. We conclude that further work on ideal criteria for identifying acceptable donor kidneys is needed.
Figure
Reference
-
1. Dahmen M, Becker F, Pavenstädt H, Suwelack B, Schütte-Nütgen K, Reuter S. 2019; Validation of the Kidney Donor Profile Index (KDPI) to assess a deceased donor's kidneys' outcome in a European cohort. Sci Rep. 9:11234. DOI: 10.1038/s41598-019-47772-7. PMID: 31375750. PMCID: PMC6677881.2. Heldal K, Hartmann A, Grootendorst DC, de Jager DJ, Leivestad T, Foss A, et al. 2010; Benefit of kidney transplantation beyond 70 years of age. Nephrol Dial Transplant. 25:1680–7. DOI: 10.1093/ndt/gfp681. PMID: 20038521. PMCID: PMC2856560.3. Swinarska JT, Stratta RJ, Rogers J, Chang A, Farney AC, Orlando G, et al. 2021; Early graft loss after deceased-donor kidney transplantation: what are the consequences? J Am Coll Surg. 232:493–502. DOI: 10.1016/j.jamcollsurg.2020.12.005. PMID: 33348013.4. Stenberg B, Talbot D, Khurram M, Kanwar A, Ray C, Mownah O, et al. 2011; A new technique for assessing renal transplant perfusion preoperatively using contrast-enhanced ultrasound (CEUS) and three-dimensional ultrasound (3DUS): a porcine model pilot study. Ultraschall Med. 32 Suppl 2:E8–13. DOI: 10.1055/s-0031-1281650. PMID: 22179806.5. Kerr H, Richards A. 2012; Complement-mediated injury and protection of endothelium: lessons from atypical haemolytic uraemic syndrome. Immunobiology. 217:195–203. DOI: 10.1016/j.imbio.2011.07.028. PMID: 21855165. PMCID: PMC4083254.6. de Kok MJ, Schaapherder AF, Mensink JW, de Vries AP, Reinders ME, Konijn C, et al. 2020; A nationwide evaluation of deceased donor kidney transplantation indicates detrimental consequences of early graft loss. Kidney Int. 97:1243–52. DOI: 10.1016/j.kint.2020.01.043. PMID: 32359810.7. Juluru K, Rotman JA, Masi P, Spandorfer R, Ceraolo CA, Giambrone AE, et al. 2015; Semiautomated CT-based quantification of donor kidney volume applied to a predictive model of outcomes in renal transplantation. AJR Am J Roentgenol. 204:W566–72. DOI: 10.2214/AJR.14.13454. PMID: 25905963.8. Sikora MB, Shaaban A, Beddhu S, Bourija H, Wei G, Baird B, et al. 2012; Effect of donor kidney volume on recipient outcome: does the "dose" matter? Transplantation. 94:1124–30. DOI: 10.1097/TP.0b013e31826f135e. PMID: 23060282.9. Beland MD, Walle NL, Machan JT, Cronan JJ. 2010; Renal cortical thickness measured at ultrasound: is it better than renal length as an indicator of renal function in chronic kidney disease? AJR Am J Roentgenol. 195:W146–9. DOI: 10.2214/AJR.09.4104. PMID: 20651174.10. Fung A, Zhao H, Yang B, Lian Q, Ma D. 2016; Ischaemic and inflammatory injury in renal graft from brain death donation: an update review. J Anesth. 30:307–16. DOI: 10.1007/s00540-015-2120-y. PMID: 26746399.11. De Vusser K, Lerut E, Kuypers D, Vanrenterghem Y, Jochmans I, Monbaliu D, et al. 2013; The predictive value of kidney allograft baseline biopsies for long-term graft survival. J Am Soc Nephrol. 24:1913–23. DOI: 10.1681/ASN.2012111081. PMID: 23949799. PMCID: PMC3810080.12. Gaber LW, Moore LW, Alloway RR, Amiri MH, Vera SR, Gaber AO. 1995; Glomerulosclerosis as a determinant of posttransplant function of older donor renal allografts. Transplantation. 60:334–9. DOI: 10.1097/00007890-199508270-00006. PMID: 7652761.13. Dare AJ, Pettigrew GJ, Saeb-Parsy K. 2014; Preoperative assessment of the deceased-donor kidney: from macroscopic appearance to molecular biomarkers. Transplantation. 97:797–807. DOI: 10.1097/01.TP.0000441361.34103.53. PMID: 24553618.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation and Utilization of Expanded Criteria Dornor
- A Preliminary Study to Revise the Marginal Donor Criteria of KONOS in Deceased Donor Kidney Transplantation
- Thrombotic microangiopathy, rare cause of deceased donor acute kidney injury: is a donor biopsy necessary before donation?
- Evaluation of the Recipient and Donor in Living Kidney Transplantation
- Validation of the KDRI in Korean Deceased Donor Kidney Transplantation