Blood Res.
2022 Sep;57(3):216-222. 10.5045/br.2022.2022085.
Chest multidetector computed tomography imaging of COVID-19 pneumonia patients with hematologic malignancies
- Affiliations
-
- 1Department of Radiology, Faculty of Medicine, Mansoura University, Mansoura, Egypt
- 2Faculty of Oral and Dental Medicine, Delta University for Science and Technology, Gamasa, Dakahlya, Egypt
- KMID: 2533249
- DOI: http://doi.org/10.5045/br.2022.2022085
Abstract
- Background
Data on the association between coronavirus disease 2019 (COVID-19) and the epidemiology and outcomes of hematological malignancies are limited. Hence, the present study aimed to assess the imaging findings using chest multidetector computed tomography (MDCT) in patients with hematologic malignancies who developed COVID-19 pneumonia.
Methods
This retrospective study included two groups, the first group consisted of COVID-19 infected patients with hematologic malignancies (100 patients), while the second group consisted of COVID-19 infected patients without hematologic malignancies or other comorbidities (100 patients). The hematological malignancies included in this study were non-Hodgkin’s lymphoma (40 patients), acute myeloid leukemia (25 patients), chronic lymphocytic leukemia (15 patients), multiple myeloma (10 patients), Hodgkin’s lymphoma (8 patients), and myelodysplastic syndrome (2 patients). Chest multidetector CT imaging was performed in all patients to assess for ground-glass opacity, consolidation, pleural effusion, and airway abnormalities.
Results
More than one CT finding was reported in each patient. No significant difference was observed in the ground-glass opacities (P =0.0594), nodule formation (P =0.2278), or airway thickening/dilatation (P =0.0566) between the two groups; meanwhile, a significant difference was observed in the degree of consolidation, the number of lobes affected, and pleural effusion (P =0.0001) as well as in the total lung severity (P =0.0001); minimal, mild, and severe affection rates; and (P =0.0047) moderate affection rates.
Conclusion
Early and reliable diagnosis of lung disease in COVID-19-infected patients may be achieved through multidetector CT imaging. Patients with hematological malignancies are more likely to have severe COVID-19 pneumonia, and radiologists should recognize the CT characteristics of this infection.
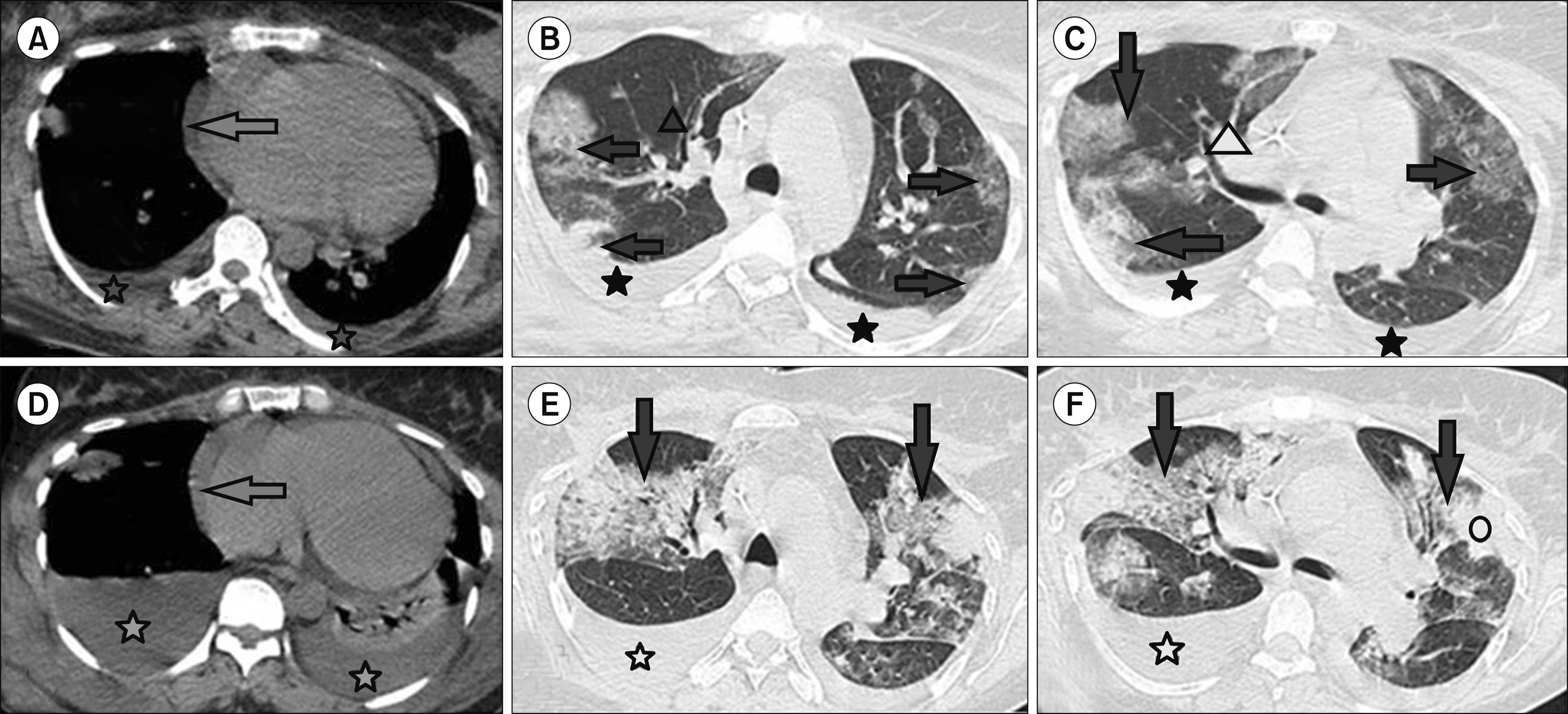
Figure
Reference
-
1. Zhu N, Zhang D, Wang W, et al. 2020; A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 382:727–33. DOI: 10.1056/NEJMoa2001017. PMID: 31978945. PMCID: PMC7092803.
Article2. Mahase E. 2020; China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 368:m408. DOI: 10.1136/bmj.m408. PMID: 32005727.
Article3. Wang W, Tang J, Wei F. 2020; Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 92:441–7. DOI: 10.1002/jmv.25689. PMID: 31994742. PMCID: PMC7167192.
Article4. Fang Y, Zhang H, Xie J, et al. 2020; Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 296:E115–7. DOI: 10.1148/radiol.2020200432. PMID: 32073353. PMCID: PMC7233365.5. Wang Y, Hou H, Wang W, Wang W. 2020; Combination of CT and RT-PCR in the screening or diagnosis of COVID-19. J Glob Health. 10:010347. DOI: 10.7189/jogh.10.010347. PMID: 32373325. PMCID: PMC7183249.
Article6. Ai T, Yang Z, Hou H, et al. 2020; Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 296:E32–40. DOI: 10.1148/radiol.2020200642. PMID: 32101510. PMCID: PMC7233399.7. Bernheim A, Mei X, Huang M, et al. 2020; Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 295:200463. DOI: 10.1148/radiol.2020200463. PMID: 32077789. PMCID: PMC7233369.
Article8. Zhou S, Wang Y, Zhu T, Xia L. 2020; CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. AJR Am J Roentgenol. 214:1287–94. DOI: 10.2214/AJR.20.22975. PMID: 32134681.
Article9. Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. 2018; Radiographic and CT features of viral pneumonia. Radiographics. 38:719–39. DOI: 10.1148/rg.2018170048. PMID: 29757717. PMCID: PMC7336757.
Article10. Zu ZY, Jiang MD, Xu PP, et al. 2020; Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 296:E15–25. DOI: 10.1148/radiol.2020200490. PMID: 32083985. PMCID: PMC7233368.
Article11. Li Y, Xia L. 2020; Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 214:1280–6. DOI: 10.2214/AJR.20.22954. PMID: 32130038.
Article12. Cheng Z, Lu Y, Cao Q, et al. 2020; Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am J Roentgenol. 215:121–6. DOI: 10.2214/AJR.20.22959. PMID: 32174128.
Article13. Kanne JP. 2020; Chest CT findings in 2019 novel coronavirus (2019- nCoV) infections from Wuhan, China: key points for the radiologist. Radiology. 295:16–7. DOI: 10.1148/radiol.2020200241. PMID: 32017662. PMCID: PMC7233362.
Article14. Pan F, Ye T, Sun P, et al. 2020; Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 295:715–21. DOI: 10.1148/radiol.2020200370. PMID: 32053470. PMCID: PMC7233367.
Article15. Chung M, Bernheim A, Mei X, et al. 2020; CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 295:202–7. DOI: 10.1148/radiol.2020200230. PMID: 32017661. PMCID: PMC7194022.
Article16. Song F, Shi N, Shan F, et al. 2020; Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 295:210–7. DOI: 10.1148/radiol.2020200274. PMID: 32027573. PMCID: PMC7233366.
Article17. Pan Y, Guan H, Zhou S, et al. 2020; Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 30:3306–9. DOI: 10.1007/s00330-020-06731-x. PMID: 32055945. PMCID: PMC7087663.
Article18. Liu T, Huang P, Liu H, et al. 2020; Spectrum of chest CT findings in a familial cluster of COVID-19 infection. Radiol Cardiothorac Imaging. 2:e200025. DOI: 10.1148/ryct.2020200025. PMID: 33778542. PMCID: PMC7233390.19. Kong W, Agarwal PP. 2020; Chest imaging appearance of COVID-19 infection. Radiol Cardiothorac Imaging. 2:e200028. DOI: 10.1148/ryct.2020200028. PMID: 33778544. PMCID: PMC7233424.
Article20. Li X, Zeng X, Liu B, Yu Y. 2020; COVID-19 infection presenting with CT halo sign. Radiol Cardiothorac Imaging. 2:e200026. DOI: 10.1148/ryct.2020200026. PMID: 33778543. PMCID: PMC7194018.
Article21. Zu ZY, Jiang MD, Xu PP. 2020; Radiological diagnosis of new coronavirus infected pneumonitis: expert recommendation from the Chinese Society of Radiology. Chin J Radiol. 54:E001.22. El-Badrawy A, Zeidan A, Ebrahim MA. 2012; 64 multidetector CT findings of influenza A (H1N1) virus in patients with hematologic malignancies. Acta Radiol. 53:662–7. DOI: 10.1258/ar.2012.120038. PMID: 22734081.
Article23. Malainou C, Herold S. 2019; Influenza. Internist (Berl). 60:1127–35. DOI: 10.1007/s00108-019-00670-6. PMID: 31478058.
Article24. de Wit E, van Doremalen N, Falzarano D, Munster VJ. 2016; SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 14:523–34. DOI: 10.1038/nrmicro.2016.81. PMID: 27344959. PMCID: PMC7097822.
Article25. Hui DSC, Zumla A. 2019; Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am. 33:869–89. DOI: 10.1016/j.idc.2019.07.001. PMID: 31668196. PMCID: PMC7127569.26. Chan JF, Lau SK, To KK, Cheng VC, Woo PC, Yuen KY. 2015; Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like disease. Clin Microbiol Rev. 28:465–522. DOI: 10.1128/CMR.00102-14. PMID: 25810418. PMCID: PMC4402954.
Article27. Gosain R, Abdou Y, Singh A, Rana N, Puzanov I, Ernstoff MS. 2020; COVID-19 and cancer: a comprehensive review. Curr Oncol Rep. 22:53. DOI: 10.1007/s11912-020-00934-7. PMID: 32385672. PMCID: PMC7206576.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Contusion Similar to COVID-19 Pneumonia
- Role of chest imaging in the diagnosis and treatment of COVID-19
- Clinical and Radiologic Findings of COVID-19 Pneumonia: South Korean Experience from Three Cases
- Immune Response to COVID-19 Vaccination in Hematologic Malignancies: A Mini-Review
- Mediastinal Emphysema, Giant Bulla, and PneumothoraxDeveloped during the Course of COVID-19 Pneumonia