J Korean Assoc Oral Maxillofac Surg.
2022 Aug;48(4):225-231. 10.5125/jkaoms.2022.48.4.225.
Randomized clinical trial to evaluate the efficacy and safety of two types of sandblasted with large-grit and acid-etched surface implants with different surface roughness
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Dentistry and Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea
- 3Department of Prosthodontics, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2532826
- DOI: http://doi.org/10.5125/jkaoms.2022.48.4.225
Abstract
Objectives
This study aims to evaluate the efficacy and safety of two types of sandblasted with large-grit and acid-etched (SLA) surface implants with different surface roughness.
Patients and Methods
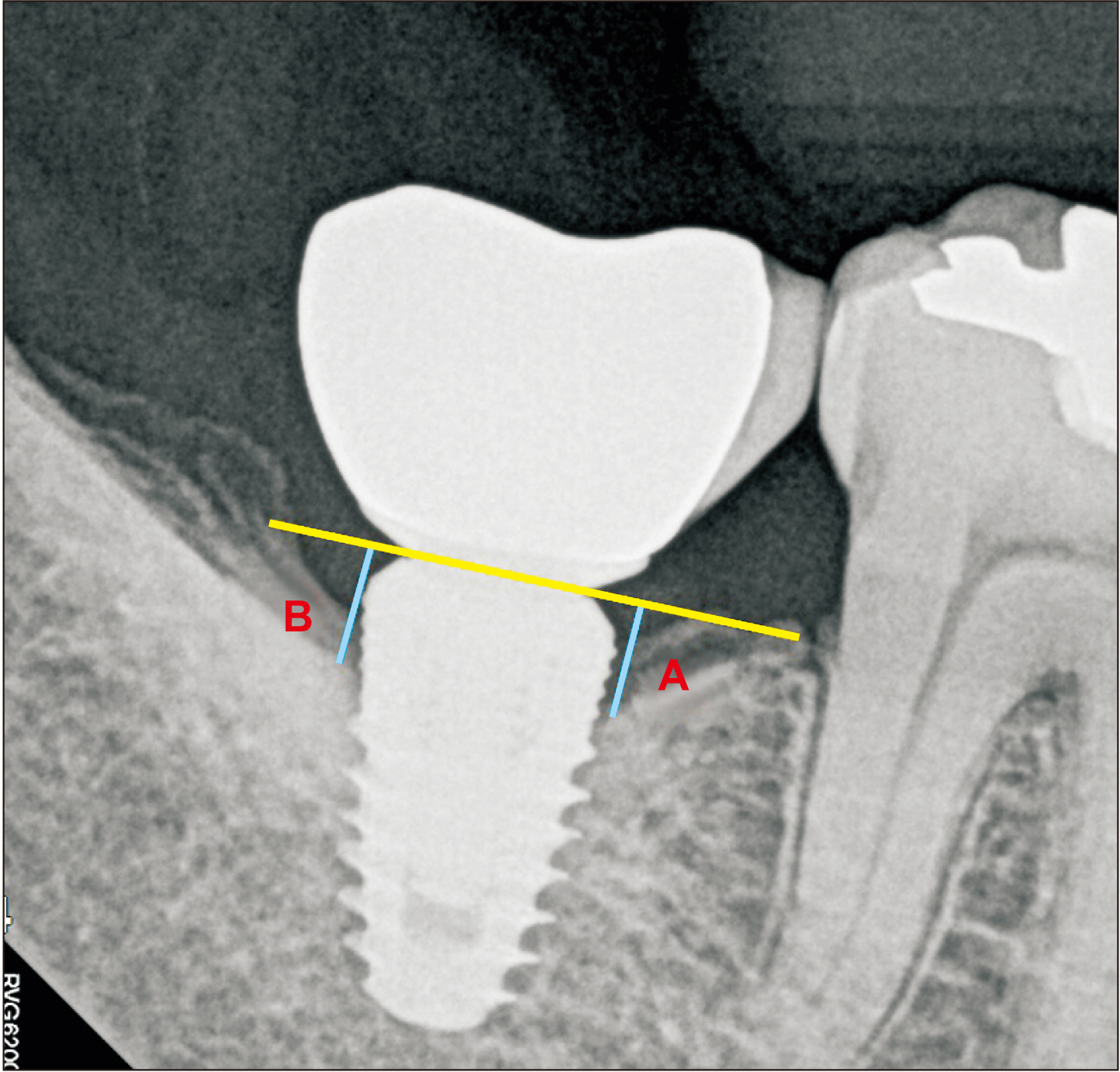
This study was conducted based on a clinical record review of 55 patients (mean age, 53.00 years). A total of 80 SLA surface implants was placed. Among the 80 implants, 38 implants placed in 29 subjects had surface roughness (Ra) of 3.09 µm (test group, TG), while the other 42 implants placed in 31 subjects had a surface roughness (Ra) of 2.50 µm (control group, CG). A comparison was made of implant primary/ secondary stability; success and survival rates; marginal bone loss; and soft tissue assessment including probing pocket depth (PPD), plaque index (PI), gingival index (GI), and bleeding on probing (BOP) between the groups at 1 year after implant placement.
Results
Among the implants that were initially registered, 1 from the TG and 4 from the CG dropped out, leaving 37 implants in the TG and 38 implants in the CG to be traced and analyzed. Although 1 TG case showed unstable primary stability, all cases showed stable secondary stability. Success and survival rates at 1 year after implant placement were 100% in both groups. Marginal bone loss was 0.07 mm and 0.00 mm for the TG and CG, respectively, but the difference was not significant. Among the several parameters for evaluation of soft tissue, the TG showed lower PI at 1 year after implant placement (TG=0.00, CG=0.29; P=0.0004), while the remaining categories showed no significant difference between the groups.
Conclusion
This study shows that the two types of SLA implants with different surface roughness have no difference in efficacy or safety. Therefore, both of the implants can be used safely and with promising outcomes.
Keyword
Figure
Reference
-
References
1. Kim HK, Lee EY, Kim JJ. 2015; Five-year retrospective radiographic follow-up study of dental implants with sandblasting with large grit, and acid etching-treated surfaces. J Korean Assoc Oral Maxillofac Surg. 41:317–21. https://doi.org/10.5125/jkaoms.2015.41.6.317. DOI: 10.5125/jkaoms.2015.41.6.317. PMID: 26734558. PMCID: PMC4699932.
Article2. Rosales-Leal JI, Rodríguez-Valverde MA, Mazzaglia G, Ramón-Torregrosa PJ, Díaz-Rodríguez L, García-Martínez O, et al. 2010; Effect of roughness, wettability and morphology of engineered titanium surfaces on osteoblast-like cell adhesion. Colloids Surf A Physicochem Eng Asp. 365:222–9. https://doi.org/10.1016/j.colsurfa.2009.12.017. DOI: 10.1016/j.colsurfa.2009.12.017.
Article3. Elkhaweldi A, Lee DH, Wang WCW, Cho SC. 2014; The survival rate of RBM surface versus SLA surface in geometrically identical implant design. J Oral Biol. 1:8. DOI: 10.13188/2377-987x.1000004.4. Smeets R, Stadlinger B, Schwarz F, Beck-Broichsitter B, Jung O, Precht C, et al. 2016; Impact of dental implant surface modifications on osseointegration. Biomed Res Int. 2016:6285620. https://doi.org/10.1155/2016/6285620. DOI: 10.1155/2016/6285620. PMID: 27478833. PMCID: PMC4958483.
Article5. Buser D, Janner SF, Wittneben JG, Brägger U, Ramseier CA, Salvi GE. 2012; 10-Year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 14:839–51. https://doi.org/10.1111/j.1708-8208.2012.00456.x. DOI: 10.1111/j.1708-8208.2012.00456.x. PMID: 22897683.
Article6. Kim SB, Yun PY, Kim SY, Yi YJ, Kim JY, Kim YK. 2016; Prospective randomized clinical trial of hydrophilic tapered implant placement at maxillary posterior area: 6 weeks and 12 weeks loading. J Adv Prosthodont. 8:396–403. https://doi.org/10.4047/jap.2016.8.5.396. DOI: 10.4047/jap.2016.8.5.396. PMID: 27826390. PMCID: PMC5099132.
Article7. Kim MJ, Yun PY, Chang NH, Kim YK. 2020; The long-term evaluation of the prognosis of implants with acid-etched surfaces sandblasted with alumina: a retrospective clinical study. Maxillofac Plast Reconstr Surg. 42:10. https://doi.org/10.1186/s40902-020-00255-6. DOI: 10.1186/s40902-020-00255-6. PMID: 32296662. PMCID: PMC7142172.
Article8. Goyal N, Kaur R. 2012; Effect of various implant surface treatments on osseointegration - a literature review. Indian J Dent Sci. 4:154–7.9. Jemat A, Ghazali MJ, Razali M, Otsuka Y. 2015; Surface modifications and their effects on titanium dental implants. Biomed Res Int. 2015:791725. https://doi.org/10.1155/2015/791725. DOI: 10.1155/2015/791725. PMID: 26436097. PMCID: PMC4575991.
Article10. Knabe C, Klar F, Fitzner R, Radlanski RJ, Gross U. 2002; In vitro investigation of titanium and hydroxyapatite dental implant surfaces using a rat bone marrow stromal cell culture system. Biomaterials. 23:3235–45. https://doi.org/10.1016/s0142-9612(02)00078-9. DOI: 10.1016/S0142-9612(02)00078-9. PMID: 12102195.
Article11. Rodrigo D, Aracil L, Martin C, Sanz M. 2010; Diagnosis of implant stability and its impact on implant survival: a prospective case series study. Clin Oral Implants Res. 21:255–61. https://doi.org/10.1111/j.1600-0501.2009.01820.x. DOI: 10.1111/j.1600-0501.2009.01820.x. PMID: 19958375.
Article12. Matos GRM. 2021; Surface roughness of dental implant and osseointegration. J Maxillofac Oral Surg. 20:1–4. https://doi.org/10.1007/s12663-020-01437-5. DOI: 10.1007/s12663-020-01437-5. PMID: 33584035. PMCID: PMC7855123.
Article13. Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. 2012; Success criteria in implant dentistry: a systematic review. J Dent Res. 91:242–8. https://doi.org/10.1177/0022034511431252. DOI: 10.1177/0022034511431252. PMID: 22157097.
Article14. Newman M, Takei H, Klokkevold P, Carranza F. 2014. Carranzaʼs clinical periodontology. 12th ed. Saunders;St. Louis (MO):15. Gittens RA, Olivares-Navarrete R, Schwartz Z, Boyan BD. 2014; Implant osseointegration and the role of microroughness and nanostructures: lessons for spine implants. Acta Biomater. 10:3363–71. https://doi.org/10.1016/j.actbio.2014.03.037. DOI: 10.1016/j.actbio.2014.03.037. PMID: 24721613. PMCID: PMC4103432.
Article16. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. 1981; Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 52:155–70. https://doi.org/10.3109/17453678108991776. DOI: 10.3109/17453678108991776. PMID: 7246093.
Article17. Anil S, Anand PS, Alghamdi H, Jansen JA. Turkyilmaz I, editor. 2011. Dental implant surface enhancement and osseointegration. Implant dentistry. IntechOpen;London: p. 83–108. DOI: 10.5772/16475.
Article18. Elias CN, Meirelles L. 2010; Improving osseointegration of dental implants. Expert Rev Med Devices. 7:241–56. https://doi.org/10.1586/erd.09.74. DOI: 10.1586/erd.09.74. PMID: 20214429.
Article19. Lee JH, Jeong SN. 2020; Efficacy of deep convolutional neural network algorithm for the identification and classification of dental implant systems, using panoramic and periapical radiographs: a pilot study. Medicine (Baltimore). 99:e20787. https://doi.org/10.1097/MD.0000000000020787. DOI: 10.1097/MD.0000000000020787. PMID: 32590758. PMCID: PMC7328970.
Article20. OʼSullivan D, Sennerby L, Meredith N. 2004; Influence of implant taper on the primary and secondary stability of osseointegrated titanium implants. Clin Oral Implants Res. 15:474–80. https://doi.org/10.1111/j.1600-0501.2004.01041.x. DOI: 10.1111/j.1600-0501.2004.01041.x. PMID: 15248883.
Article21. Javed F, Ahmed HB, Crespi R, Romanos GE. 2013; Role of primary stability for successful osseointegration of dental implants: factors of influence and evaluation. Interv Med Appl Sci. 5:162–7. https://doi.org/10.1556/IMAS.5.2013.4.3. DOI: 10.1556/imas.5.2013.4.3. PMID: 24381734. PMCID: PMC3873594.
Article22. Jang WW, Kang DW, Kim YK. 2019; Long-term evaluation of the prognosis of straight and tapered implant with resorbable blast media surface: retrospective clinical study. Oral Biol Res. 43:23–31. https://doi.org/10.21851/obr.43.01.201903.23. DOI: 10.21851/obr.43.01.201903.23.
Article23. Chambrone L, Shibli JA, Mercúrio CE, Cardoso B, Preshaw PM. 2015; Efficacy of standard (SLA) and modified sandblasted and acid-etched (SLActive) dental implants in promoting immediate and/or early occlusal loading protocols: a systematic review of prospective studies. Clin Oral Implants Res. 26:359–70. https://doi.org/10.1111/clr.12347. DOI: 10.1111/clr.12347. PMID: 24814519.
Article24. van Velzen FJ, Ofec R, Schulten EA, Ten Bruggenkate CM. 2015; 10-Year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res. 26:1121–8. https://doi.org/10.1111/clr.12499. DOI: 10.1111/clr.12499. PMID: 25370914.
Article25. Shi X, Xu L, Violin KB, Lu S. 2016; Improved osseointegration of long-term stored SLA implant by hydrothermal sterilization. J Mech Behav Biomed Mater. 53:312–9. https://doi.org/10.1016/j.jmbbm.2015.08.038. DOI: 10.1016/j.jmbbm.2015.08.038. PMID: 26382972.
Article26. Lee JT, Cho SA. 2016; Biomechanical evaluation of laser-etched Ti implant surfaces vs. chemically modified SLA Ti implant surfaces: Removal torque and resonance frequency analysis in rabbit tibias. J Mech Behav Biomed Mater. 61:299–307. https://doi.org/10.1016/j.jmbbm.2016.03.034. DOI: 10.1016/j.jmbbm.2016.03.034. PMID: 27093590.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of various surface treatments for titanium on surface micro roughness, static wettability, fibronectin adsorption
- Scanning Electron Microscopic Study of the Effects of Citric Acid on the Change of Implant Surface According to Application Time
- A comparative clinical study on oxidized titanium implants and sandblasted large-grit acid etched implants in soft bone
- Retrospective clinical study of an implant with a sandblasted, large-grit, acid-etched surface and internal connection: analysis of short-term success rate and marginal bone loss
- The influence of tetracycline-HCl for micromorphology of Thermal dual acid etched surface implants