J Korean Assoc Oral Maxillofac Surg.
2022 Aug;48(4):207-218. 10.5125/jkaoms.2022.48.4.207.
Investigation of the prevalence and main features of skull-base anomalies and characteristics of the sphenoid sinus using cone-beam computed tomography
- Affiliations
-
- 1Department of Dentomaxillofacial Radiology, Faculty of Dentistry, İstanbul Medipol University, İstanbul, Turkey
- 2Mehmet Tanrıkulu Health Services Vocational School, Bolu, Turkey
- 3Department of Dentomaxillofacial Radiology, Faculty of Dentistry, Bolu Abant İzzet Baysal University, Bolu, Turkey
- 4Department of Dentomaxillofacial Radiology, Faculty of Dentistry, Ankara University, Ankara, Turkey
- 5Ankara University Medical Design Application and Research Center (MEDITAM), Ankara, Turkey
- KMID: 2532821
- DOI: http://doi.org/10.5125/jkaoms.2022.48.4.207
Abstract
Objectives
This study aimed to define the prevalence and characteristics of skull base anomalies and the features of sphenoid sinus pneumatization (SSP).
Materials and Methods
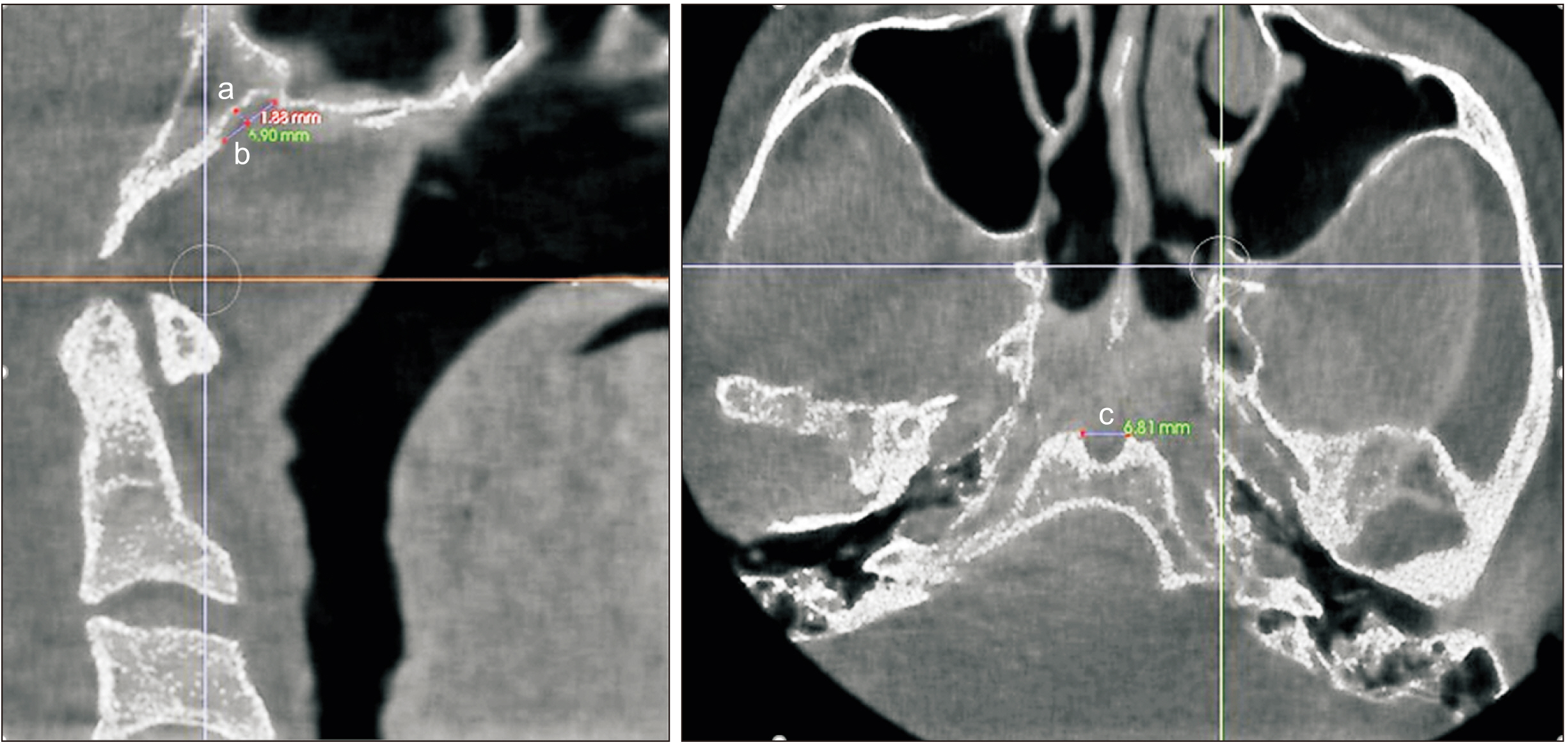
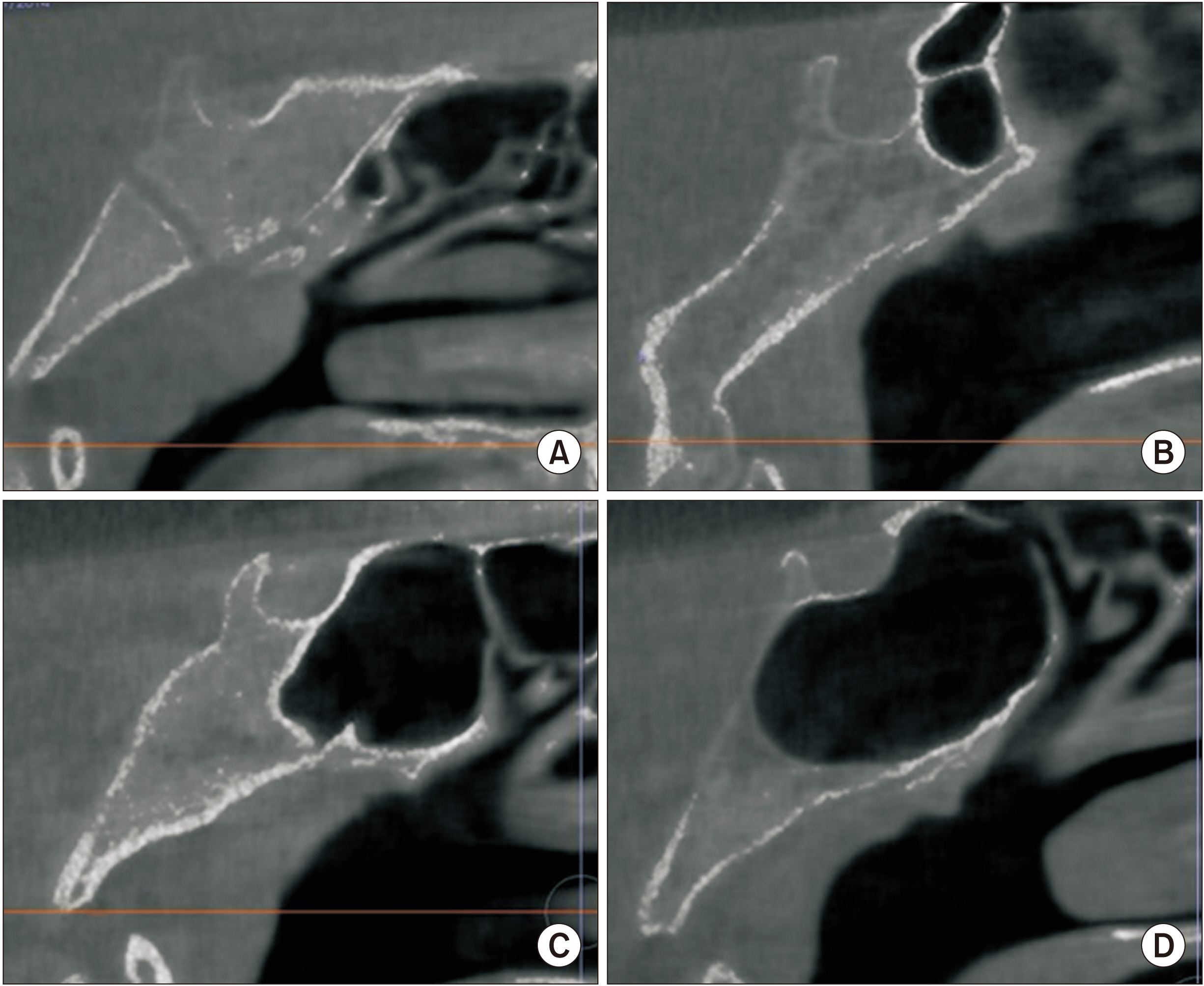
Five hundred cone-beam computed tomography scans were evaluated retrospectively for the presence of fossa navicularis magna (FNM), canalis basilaris medianus (CBM), sphenoid emissary foramen (SEF), and/or Onodi cells (OC). Patterns of the SSP and sphenoid sinus mucosa dimensions (SSMD) were also recorded.
Results
The prevalence of FNM, CBM, SEF, and OC was 26.0%, 22.4%, 47.4%, and 18.4%, respectively. Two hundred sixty-two (52.4%) sellartype SSP were defined, followed by post-sellar 191 (38.2%), pre-sellar 31 (6.2%), and conchal 16 (3.2%) types. The frequency of SSMD less than 1 mm, 1-3 mm, and greater than 3 mm was 40.6%, 38.4%, and 21.0%, respectively. An SEF was detected more frequently in females, while SSMD greater than 3 mm was more frequent in males. An FNM was more prevalent in the 18-29 and 30-39 age groups and SEF was significantly less frequent in patients over 60 years of age compared to other age groups. A sinus mucosa larger than 3 mm was more common in the younger than 18 year group. The frequency of post-sellar-type pneumatization was lower in patients younger than 18 years.
Conclusion
Skull-base anomalies are common and may be detected incidentally during imaging procedures. The sphenoid sinus, its variations, and pneumatization patterns should also be taken into consideration in imaging procedures performed for various purposes.
Keyword
Figure
Reference
-
References
1. Policeni BA, Smoker WR. 2015; Imaging of the skull base: anatomy and pathology. Radiol Clin North Am. 53:1–14. https://doi.org/10.1016/j.rcl.2014.09.005. DOI: 10.1016/j.rcl.2014.09.005. PMID: 25476171.
Article2. Rai R, Iwanaga J, Shokouhi G, Loukas M, Mortazavi MM, Oskouian RJ, et al. 2018; A comprehensive review of the clivus: anatomy, embryology, variants, pathology, and surgical approaches. Childs Nerv Syst. 34:1451–8. https://doi.org/10.1007/s00381-018-3875-x. DOI: 10.1007/s00381-018-3875-x. PMID: 29955940.
Article3. Cellina M, Gibelli D, Floridi C, Toluian T, Valenti Pittino C, Martinenghi C, et al. 2020; Sphenoid sinuses: pneumatisation and anatomical variants-what the radiologist needs to know and report to avoid intraoperative complications. Surg Radiol Anat. 42:1013–24. https://doi.org/10.1007/s00276-020-02490-y. DOI: 10.1007/s00276-020-02490-y. PMID: 32394118.
Article4. Syed AZ, Zahedpasha S, Rathore SA, Mupparapu M. 2016; Evaluation of canalis basilaris medianus using cone-beam computed tomography. Imaging Sci Dent. 46:141–4. https://doi.org/10.5624/isd.2016.46.2.141. DOI: 10.5624/isd.2016.46.2.141. PMID: 27358822. PMCID: PMC4925651.
Article5. Currarino G. 1988; Canalis basilaris medianus and related defects of the basiocciput. AJNR Am J Neuroradiol. 9:208–11. PMID: 3124576. PMCID: PMC8331533.6. Akkoca Kaplan F, Bayrakdar İŞ, Bilgir E. 2020; Incidence of anomalous canals in the base of the skull: a retrospective radio-anatomical study using cone-beam computed tomography. Surg Radiol Anat. 42:171–7. https://doi.org/10.1007/s00276-019-02307-7. DOI: 10.1007/s00276-019-02307-7. PMID: 31446447.
Article7. Bayrak S, Göller Bulut D, Orhan K. 2019; Prevalence of anatomical variants in the clivus: fossa navicularis magna, canalis basilaris medianus, and craniopharyngeal canal. Surg Radiol Anat. 41:477–83. https://doi.org/10.1007/s00276-019-02200-3. DOI: 10.1007/s00276-019-02200-3. PMID: 30725217.
Article8. Kazkayasi M, Karadeniz Y, Altinok D, Koç C. 2001; [Investigation of the anatomic variations of the sphenoid sinus with the computed tomography]. KBB ve BBC Dergisi. 9:74–7. Turkish.9. Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S. 2008; Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull Base. 18:9–15. https://doi.org/10.1055/s-2007-992764. DOI: 10.1055/s-2007-992764. PMID: 18592020. PMCID: PMC2435468.
Article10. Hiremath SB, Gautam AA, Sheeja K, Benjamin G. 2018; Assessment of variations in sphenoid sinus pneumatization in Indian population: a multidetector computed tomography study. Indian J Radiol Imaging. 28:273–9. https://doi.org/10.4103/ijri.IJRI_70_18. DOI: 10.4103/ijri.IJRI_70_18. PMID: 30319202. PMCID: PMC6176678.
Article11. Ali IK, Sansare K, Karjodkar F, Saalim M. 2020; Imaging analysis of onodi cells on cone-beam computed tomography. Int Arch Otorhinolaryngol. 24:e319–22. https://doi.org/10.1055/s-0039-1698779. DOI: 10.1055/s-0039-1698779. PMID: 32754243. PMCID: PMC7394626.
Article12. Thimmaiah VT, Anupama C. 2017; Pneumatization patterns of onodi cell on multidetector computed tomography. J Oral Maxillofac Radiol. 5:63–6. https://doi.org/10.4103/jomr.jomr_3_17. DOI: 10.4103/jomr.jomr_3_17.
Article13. Beltramello A, Puppini G, El-Dalati G, Girelli M, Cerini R, Sbarbati A, et al. 1998; Fossa navicularis magna. AJNR Am J Neuroradiol. 19:1796–8. DOI: 10.53347/rid-94018. PMID: 9802508. PMCID: PMC8337486.14. Syed AZ, Mupparapu M. 2016; Fossa navicularis magna detection on cone-beam computed tomography. Imaging Sci Dent. 46:47–51. https://doi.org/10.5624/isd.2016.46.1.47. DOI: 10.5624/isd.2016.46.1.47. PMID: 27051639. PMCID: PMC4816771.
Article15. Ersan N. 2017; Prevalence and morphometric features of fossa navicularis on cone beam computed tomography in Turkish population. Folia Morphol (Warsz). 76:715–9. https://doi.org/10.5603/FM.a2017.0030. DOI: 10.5603/FM.a2017.0030. PMID: 28353302.
Article16. Shapiro R, Robinson F. 1967; The foramina of the middle fossa: a phylogenetic, anatomic and pathologic study. Am J Roentgenol Radium Ther Nucl Med. 101:779–94. https://doi.org/10.2214/ajr.101.4.779. DOI: 10.2214/ajr.101.4.779. PMID: 6073372.
Article17. Ónodi A. 1910. The optic nerve and the accessory sinuses of the nose: a contribution to the study of canalicular neuritis and atrophy of the optic nerve of nasal origin. William Wood;New York (NY): DOI: 10.2214/ajr.101.4.779.18. Segal N, Atamne E, Shelef I, Zamir S, Landau D. 2013; Intracranial infection caused by spreading through the fossa naviclaris magna - a case report and review of the literature. Int J Pediatr Otorhinolaryngol. 77:1919–21. https://doi.org/10.1016/j.ijporl.2013.09.013. DOI: 10.1016/j.ijporl.2013.09.013. PMID: 24148862.
Article19. Prabhu SP, Zinkus T, Cheng AG, Rahbar R. 2009; Clival osteomyelitis resulting from spread of infection through the fossa navicularis magna in a child. Pediatr Radiol. 39:995–8. https://doi.org/10.1007/s00247-009-1283-9. DOI: 10.1007/s00247-009-1283-9. PMID: 19415254.
Article20. Murjani B, Bhosale R, Ramaswami E, Kadam S, Ramchandani A. 2021; Anatomical variations of clivus: a descriptive anatomical study. Surg Radiol Anat. 43:945–51. https://doi.org/10.1007/s00276-021-02686-w. DOI: 10.1007/s00276-021-02686-w. PMID: 33483831.
Article21. Akkoca Kaplan F, Yesilova E, Bayrakdar IS, Ugurlu M. 2019; Evaluation of the relationship between age and gender of fossa navicularis magna with cone-beam computed tomography in orthodontic subpopulation. J Anat Soc India. 68:201–4. DOI: 10.4103/JASI.JASI_79_19.
Article22. Magat G. 2019; Evaluation of morphometric features of fossa navicularis using cone-beam computed tomography in a Turkish subpopulation. Imaging Sci Dent. 49:209–12. https://doi.org/10.5624/isd.2019.49.3.209. DOI: 10.5624/isd.2019.49.3.209. PMID: 31583203. PMCID: PMC6761062.
Article23. Jacquemin C, Bosley TM, al Saleh M, Mullaney P. 2000; Canalis basilaris medianus: MRI. Neuroradiology. 42:121–3. https://doi.org/10.1007/s002340050029. DOI: 10.1007/s002340050029. PMID: 10663489.
Article24. Khairy S, Almubarak AO, Aloraidi A, Alahmadi KOA. 2019; Canalis basalis medianus with cerebrospinal fluid leak: rare presentation and literature review. Br J Neurosurg. 33:432–3. https://doi.org/10.1080/02688697.2017.1346173. DOI: 10.1080/02688697.2017.1346173. PMID: 28660774.
Article25. Ozer MA, Govsa F. 2014; Measurement accuracy of foramen of vesalius for safe percutaneous techniques using computer-assisted three-dimensional landmarks. Surg Radiol Anat. 36:147–54. https://doi.org/10.1007/s00276-013-1148-7. DOI: 10.1007/s00276-013-1148-7. PMID: 23793788.
Article26. Poornima B, Phaniraj S, Mallikarjun M. 2015; A study of incidence of emissary sphenoidal foramen in dry adult human skull bones. Indian J Pharm Sci Res. 5:273–5.27. Raval BB, Singh PR, Rajguru J. 2015; A morphologic and morphometric study of foramen vesalius in dry adult human skulls of gujarat region. J Clin Diagn Res. 9:AC04–7. https://doi.org/10.7860/JCDR/2015/11632.5553. DOI: 10.7860/JCDR/2015/11632.5553. PMID: 25859437. PMCID: PMC4378719.
Article28. Pathmashri VP, Thenmozhi D. 2015; Occurrence, shape and size of foramen vesalius in dry human skulls. J Pharm Sci Res. 7:718–9.29. Leonel LCPC, Peris-Celda M, de Sousa SDG, Haetinger RG, Liberti EA. 2020; The sphenoidal emissary foramen and the emissary vein: anatomy and clinical relevance. Clin Anat. 33:767–81. https://doi.org/10.1002/ca.23504. DOI: 10.1002/ca.23504. PMID: 31625185.
Article30. Bayrak S, Kurşun-Çakmak EŞ, Atakan C, Orhan K. 2018; Anatomic study on sphenoidal emissary foramen by using cone-beam computed tomography. J Craniofac Surg. 29:e477–80. https://doi.org/10.1097/SCS.0000000000004492. DOI: 10.1097/SCS.0000000000004492. PMID: 29543681.
Article31. Meybodi AT, Vigo V, Benet A. 2017; The Onodi cell: an anatomic illustration. World Neurosurg. 103:950.e5–6. https://doi.org/10.1016/j.wneu.2017.05.012. DOI: 10.1016/j.wneu.2017.05.012. PMID: 28502687.
Article32. Badawi K, Madani GA, Seddeg Y. 2017; The radiological study of Onodi cells among adult sudanese subjects. IOSR-JDMS. 16:106–9.33. Wada K, Moriyama H, Edamatsu H, Hama T, Arai C, Kojima H, et al. 2015; Identification of Onodi cell and new classification of sphenoid sinus for endoscopic sinus surgery. Int Forum Allergy Rhinol. 5:1068–76. https://doi.org/10.1002/alr.21567. DOI: 10.1002/alr.21567. PMID: 26097234.
Article34. Banaz F, Alnoury IS, Al-Shehri A, Alandejani T. 2014; Retrospective computed tomography prevalence of Onodi cells among adults in Jeddah, Saudi Arabia: age and gender difference. Am J Res Commun. 2:45–56.35. Senturk M, Guler I, Azgin I, Sakarya EU, Ovet G, Alatas N, et al. 2017; The role of Onodi cells in sphenoiditis: results of multiplanar reconstruction of computed tomography scanning. Braz J Otorhinolaryngol. 83:88–93. https://doi.org/10.1016/j.bjorl.2016.01.011. DOI: 10.1016/j.bjorl.2016.01.011. PMID: 27161189.
Article36. Shokri A, Faradmal MJ, Hekmat B. 2019; Correlations between anatomical variations of the nasal cavity and ethmoidal sinuses on cone-beam computed tomography scans. Imaging Sci Dent. 49:103–13. https://doi.org/10.5624/isd.2019.49.2.103. DOI: 10.5624/isd.2019.49.2.103. PMID: 31281787. PMCID: PMC6597371.
Article37. Idowu OE, Balogun BO, Okoli CA. 2009; Dimensions, septation, and pattern of pneumatization of the sphenoidal sinus. Folia Morphol (Warsz). 68:228–32. PMID: 19950072.38. Treviño-Gonzalez JL, Maldonado-Chapa F, Becerra-Jimenez JA, Soto-Galindo GA, Morales-Del Angel JA. 2021; Sphenoid sinus: pneumatization and septation patterns in a hispanic population. ORL J Otorhinolaryngol Relat Spec. 83:362–71. https://doi.org/10.1159/000514458. DOI: 10.1159/000514458. PMID: 33794542.
Article39. Fooanant S, Angkurawaranon S, Angkurawaranon C, Roongrotwattanasiri K, Chaiyasate S. 2017; Sphenoid sinus diseases: a review of 1,442 patients. Int J Otolaryngol. 2017:9650910. https://doi.org/10.1155/2017/9650910. DOI: 10.1155/2017/9650910. PMID: 29090009. PMCID: PMC5635283.
Article40. Kanwar SS, Mital M, Gupta PK, Saran S, Parashar N, Singh A. 2017; Evaluation of paranasal sinus diseases by computed tomography and its histopathological correlation. J Oral Maxillofac Radiol. 5:46–52.41. Marcolini TR, Safraider MC, Socher JA, Lucena GO. 2015; Differential diagnosis and treatment of isolated pathologies of the sphenoid sinus: retrospective study of 46 cases. Int Arch Otorhinolaryngol. 19:124–9. https://doi.org/10.1055/s-0034-1397337. DOI: 10.1055/s-0034-1397337. PMID: 25992167. PMCID: PMC4399171.
Article42. Turgut S, Ozcan KM, Celikkanat S, Ozdem C. 1997; Isolated sphenoid sinusitis. Rhinology. 35:132–5. DOI: 10.2500/105065895781873764. PMID: 9403945.43. Almomen A, Alshakhs A, Alturaifi A. 2020; The different causes and management of chronic sphenoid rhinosinusitis. Glob J Otolaryngol. 22:GJO.MS.ID.556076. MS.ID.556076. https://doi.org/10.19080/GJO.2020.22.556076. DOI: 10.19080/GJO.2020.22.556076.
Article44. Kushwah APS, Bhalse R, Pande S. 2015; CT evaluation of diseases of Paranasal sinuses & histopathological studies. Int J Med Res Rev. 3:1306–10. https://doi.org/10.17511/ijmrr.2015.i11.237. DOI: 10.17511/ijmrr.2015.i11.237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arrested pneumatization of the sphenoid sinus mimicking intraosseous lesions of the skull base
- Evaluation of morphometric features of fossa navicularis using cone-beam computed tomography in a Turkish subpopulation
- Chondroma of the Sphenoid Sinus: Case Report
- Prevalence of incidental paranasal sinus opacification in dental paediatric patients
- A Case of Massive Skull Base Erosion by Fungus Ball in the Sphenoid Sinus