Korean J Gastroenterol.
2022 Aug;80(2):99-102. 10.4166/kjg.2022.101.
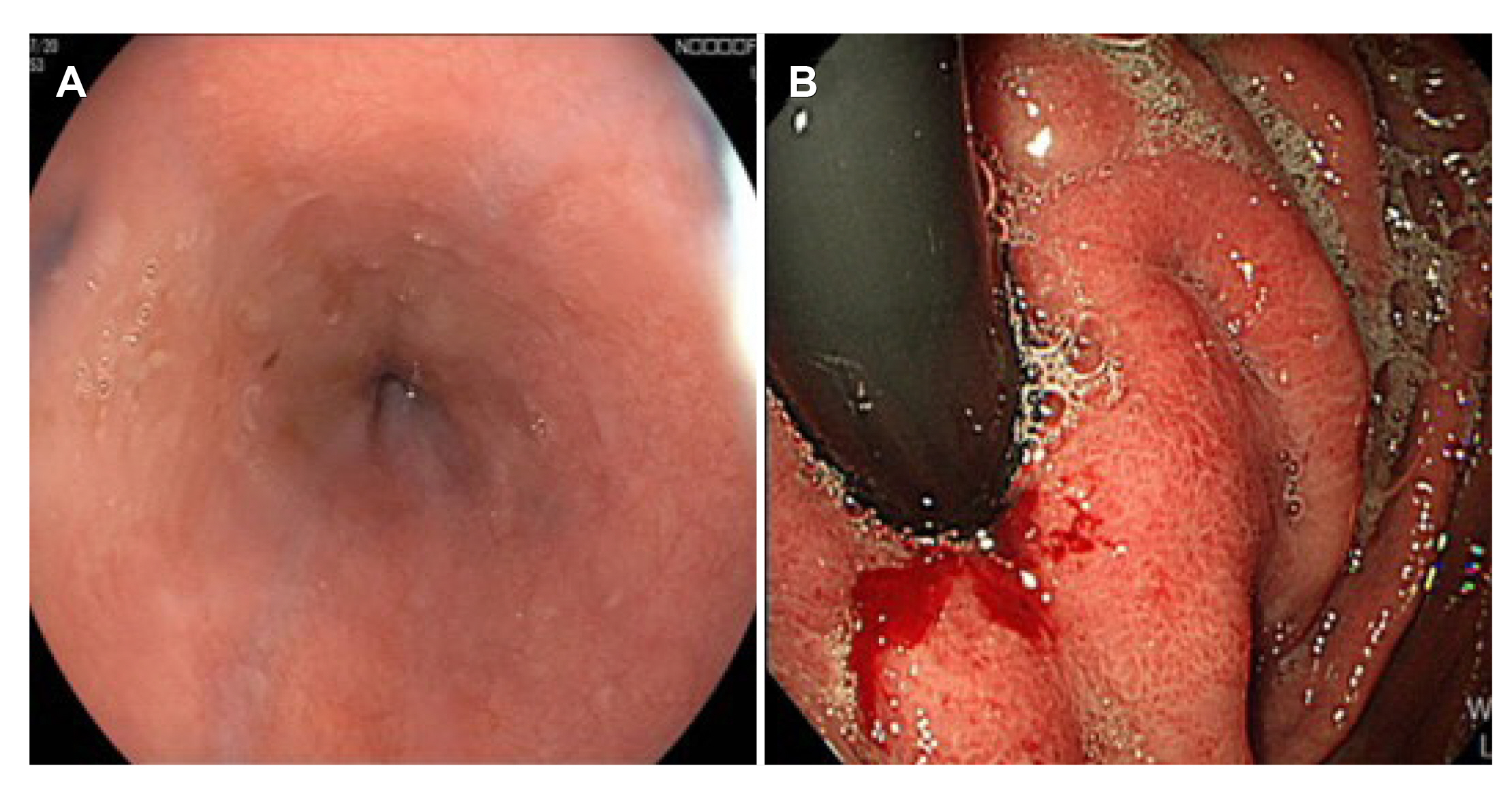
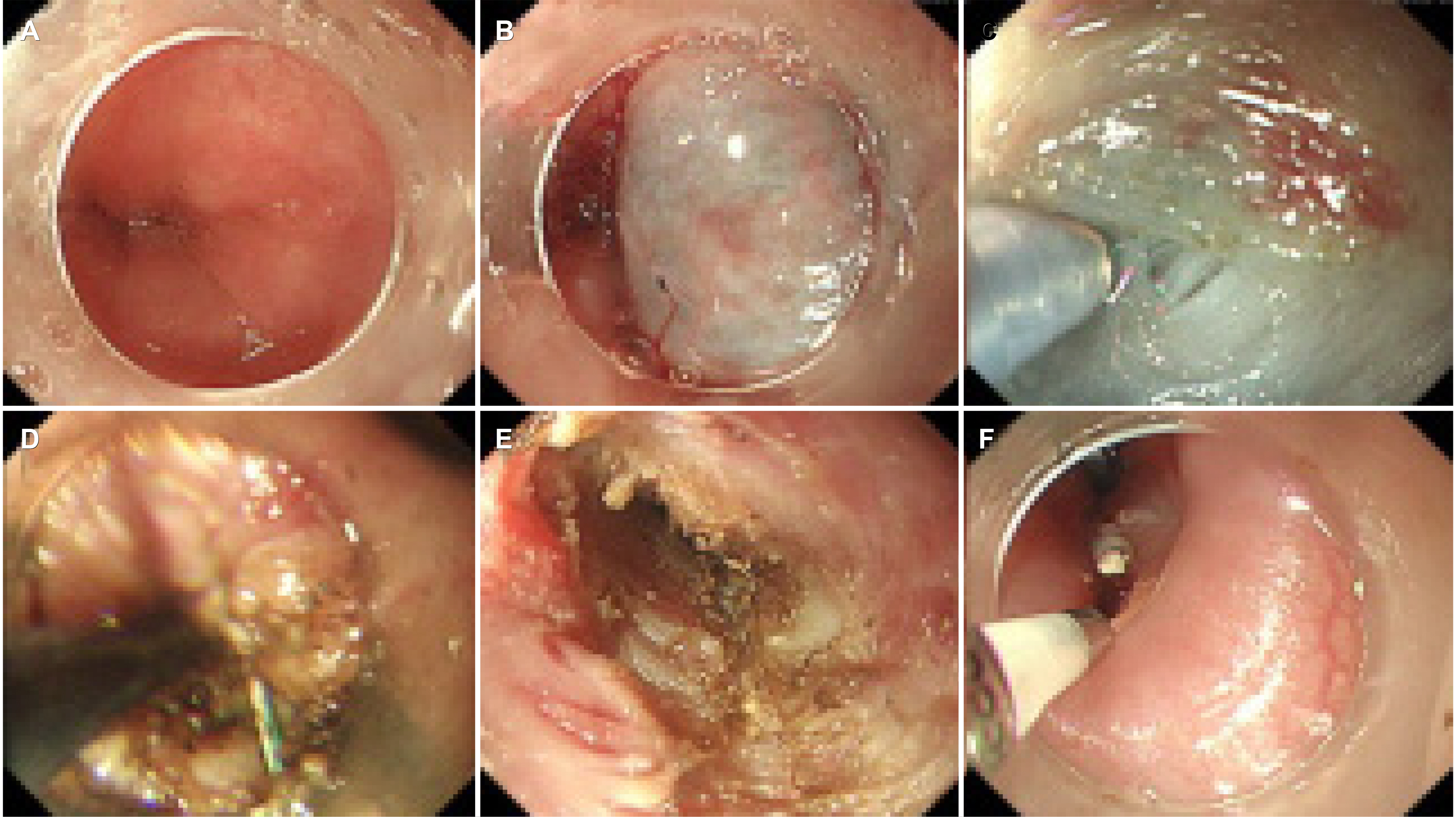
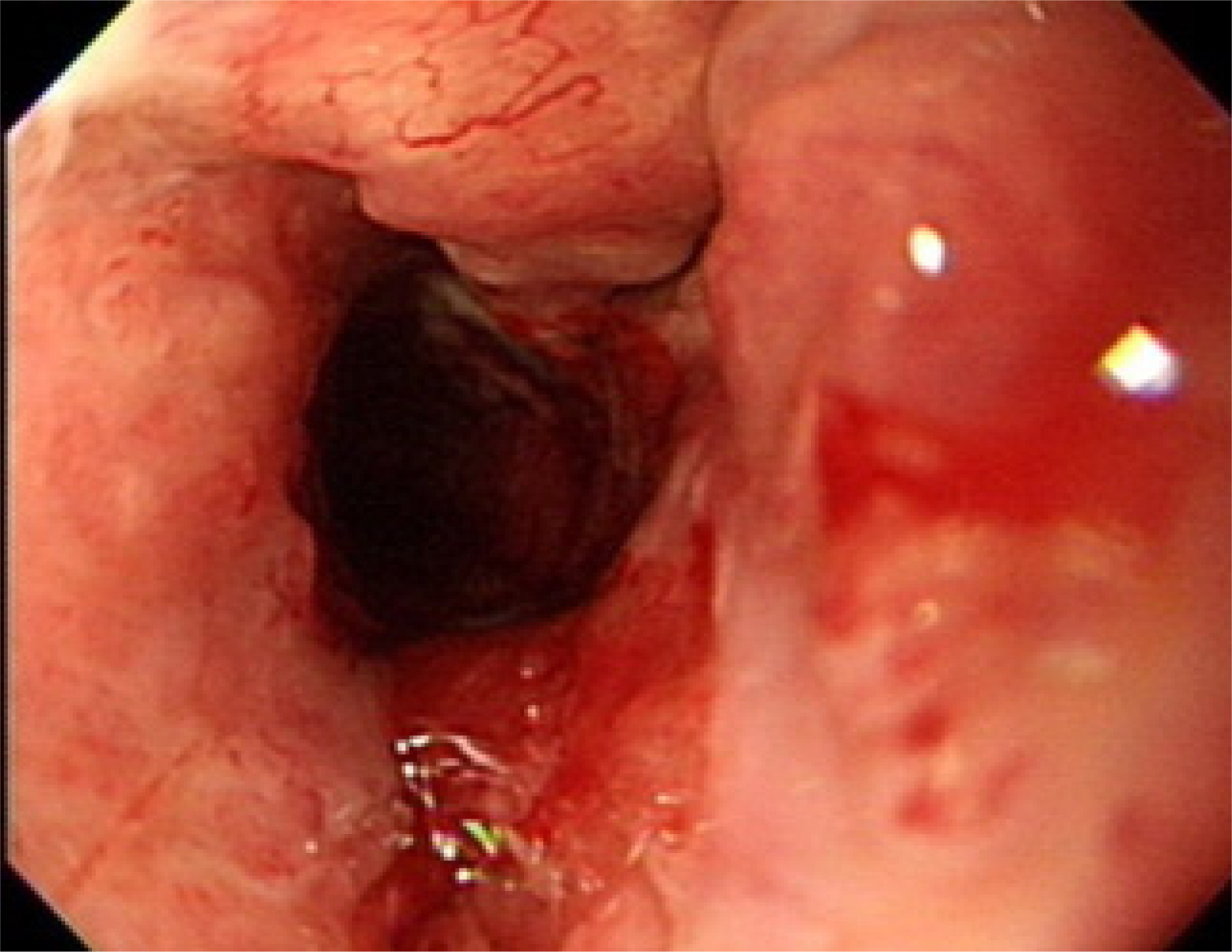
Secondary Achalasia of Gastric Linitis Plastica
- Affiliations
-
- 1Department of Gastroenterology, Cha Bundang Medical Center, CHA University, School of Medicine, Seongnam, Korea
- 2Department of Gastroenterology, CHA Gangnam Medical Center, CHA University, School of Medicine, Seoul, Korea
- KMID: 2532685
- DOI: http://doi.org/10.4166/kjg.2022.101
Figure
Reference
-
1. Liu W, Zeng XH, Yuan XL, et al. 2019; Open peroral endoscopic myotomy for the treatment of achalasia: a case series of 82 cases. Dis Esophagus. 32:1–7. DOI: 10.1093/dote/doz052. PMID: 31175357.2. Cohen S. 1979; Motor disorders of the esophagus. N Engl J Med. 301:184–192. DOI: 10.1056/NEJM197907263010404. PMID: 109758.3. Gregersen H, Lo KM. 2018; Pathophysiology and treatment of achalasia in a muscle mechanical perspective. Ann N Y Acad Sci. 1434:173–184. DOI: 10.1111/nyas.13711. PMID: 29756656.4. Cassella RR, Brown AL Jr, Sayre GP, Ellis FH Jr. 1964; Achalasia of the esophagus: pathologic and etiologic considerations. Ann Surg. 160:474–487. DOI: 10.1097/00000658-196409000-00010. PMID: 14206851. PMCID: PMC1408778.5. Kahrilas PJ, Kishk SM, Helm JF, Dodds WJ, Harig JM, Hogan WJ. 1987; Comparison of pseudoachalasia and achalasia. Am J Med. 82:439–446. DOI: 10.1016/0002-9343(87)90443-8. PMID: 3548347.6. Tucker HJ, Snape WJ Jr, Cohen S. 1978; Achalasia secondary to carcinoma: manometric and clinical features. Ann Intern Med. 89:315–318. DOI: 10.7326/0003-4819-89-3-315. PMID: 686541.7. Sandler RS, Bozymski EM, Orlando RC. 1982; Failure of clinical criteria to distinguish between primary achalasia and achalasia secondary to tumor. Dig Dis Sci. 27:209–213. DOI: 10.1007/BF01296916. PMID: 7075419.8. Kolodny M, Schrader ZR, Rubin W, Hochman R, Sleisenger MH. 1968; Esophageal achalasia probably due to gastric carcinoma. Ann Intern Med. 69:569–573. DOI: 10.7326/0003-4819-69-3-569. PMID: 5673174.9. Reynolds JC, Parkman HP. 1989; Achalasia. Gastroenterol Clin North Am. 18:223–255. DOI: 10.1016/S0889-8553(21)00676-2. PMID: 23452629. PMCID: PMC3618975.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metastatic Gastric Linitis Plastica from Bladder Cancer Mimicking a Primary Gastric Carcinoma: a Case Report
- Primary Linitis Plastica of the Rectum: A Clinico-Pathologic Analysis of Five Cases with Special Reference to Comparison with Gastric Form
- Primary Linitis Plastica of the Colon with Mucinous Adenocarcinoma in Young Woman
- Gastric Outlet Obstruction Due to Gastric Amyloidosis Mimicking Malignancy in a Patient with Ankylosing Spondylitis
- Borrmann Type 4 Advanced Gastric Cancer: Focus on the Development of Scirrhous Gastric Cancer