Ann Hepatobiliary Pancreat Surg.
2022 Aug;26(3):257-262. 10.14701/ahbps.21-159.
Influence of middle hepatic vein resection during right or left hepatectomy on post hepatectomy outcomes
- Affiliations
-
- 1Department of Hepato-Biliary and Pancreatic and Liver Transplantation, Queen Elizabeth Hospital, Birmingham, UK
- 2Department of Nuclear Medicine, Queen Elizabeth Hospital, Birmingham, UK
- KMID: 2532642
- DOI: http://doi.org/10.14701/ahbps.21-159
Abstract
- Backgrounds/Aims
Middle hepatic vein (MHV) is usually preserved as a part of the right or left hepatectomy in order preserve the venous outf low of remnant liver. The aim of this study was to evaluate if resection of MHV could inf luence post-resection outcomes of standard right or left hepatectomy.
Methods
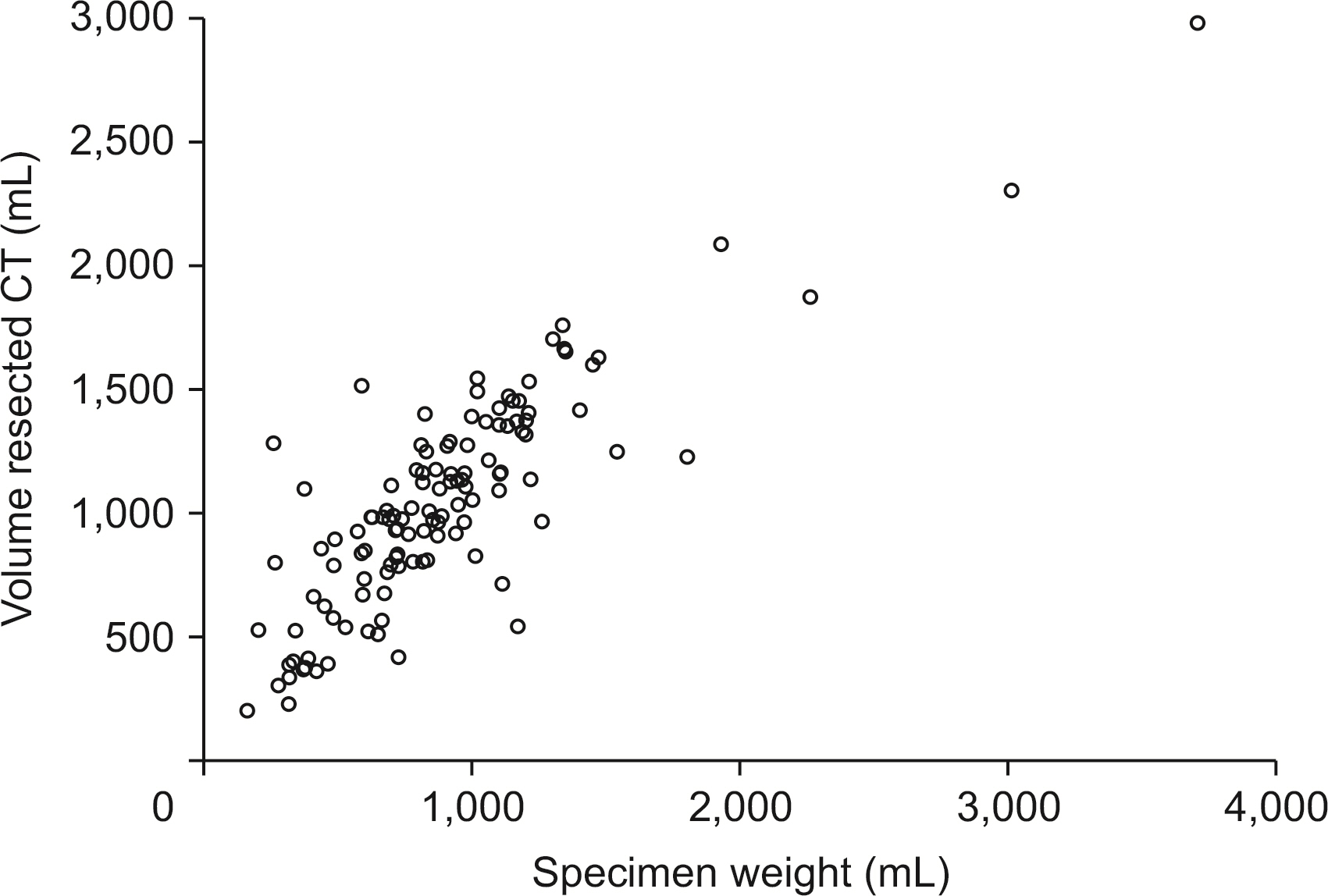
Patients who underwent standard right or left hepatectomy between January 2015 and December 2019 were included. Anatomical remnant liver volumes were measured retrospectively using the Hermes workstation (Hermes Medical Solutions AB, Stockholm, Sweden). Uni- and multi-variate analyses were performed to assess the difference in outcomes of those with preservation of MHV and those without preservation.
Results
A total of 144 patients were included. Right hepatectomy was performed for 114 (79.2%) and left hepatectomy was performed for 30 (20.8%) patients. MHV was resected for 13 (9.0%) in addition to the standard right or left hepatectomy. Median remnant liver volume was significantly higher in the MHV resected group (p < 0.01). There was no significant difference in serum level of bilirubin, international normalized ratio, alanine aminotransferase, creatinine on postoperative day 1, 3, 5, or 10, ≥ grade IIIa complications (p = 0.44), or 90-day mortality (p = 0.41). On multivariable analysis, resection of the MHV did not inf luence the incidence of post hepatectomy liver failure (p= 0.52).
Conclusions
Resection of the MHV at standard right or left hepatectomy did not have a negative impact on postoperative outcomes of patients with adequate remnant liver volume.
Keyword
Figure
Reference
-
1. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. 2011; Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 149:713–724. DOI: 10.1016/j.surg.2010.10.001. PMID: 21236455.2. Lee JW, Lee JH, Park Y, Lee W, Kwon J, Song KB, et al. 2020; Risk factors of posthepatectomy liver failure for perihilar cholangiocarcinoma: risk score and significance of future liver remnant volume-to-body weight ratio. J Surg Oncol. 122:469–479. DOI: 10.1002/jso.25974. PMID: 32424895.3. Inoue Y, Suzuki Y, Ota M, Fujii K, Kawaguchi N, Shimizu T, et al. 2018; Comparison of regeneration of remnant liver after hemihepatectomy with or without the middle hepatic vein. World J Surg. 42:1100–1110. DOI: 10.1007/s00268-017-4225-y. PMID: 28929234.4. Yu PF, Wu J, Zheng SS. 2007; Management of the middle hepatic vein and its tributaries in right lobe living donor liver transplantation. Hepatobiliary Pancreat Dis Int. 6:358–363. PMID: 17690029.5. Varghese CT, Bharathan VK, Gopalakrishnan U, Balakrishnan D, Menon RN, Sudheer OV, et al. 2018; Randomized trial on extended versus modified right lobe grafts in living donor liver transplantation. Liver Transpl. 24:888–896. DOI: 10.1002/lt.25014. PMID: 29350831.6. Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, et al. 2000; Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery. 127:512–519. DOI: 10.1067/msy.2000.105294. PMID: 10819059.7. Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, et al. 1995; Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 21:1317–1321. DOI: 10.1002/hep.1840210515. PMID: 7737637.8. Guglielmi A, Ruzzenente A, Conci S, Valdegamberi A, Iacono C. 2012; How much remnant is enough in liver resection? Dig Surg. 29:6–17. DOI: 10.1159/000335713. PMID: 22441614.9. Dasari BVM, Wilson M, Pufal K, Kadam P, Hodson J, Roberts KJ, et al. 2021; Variations between the anatomical and functional distribution, based on 99m technetium -mebrofinate SPECT-CT scan, in patients at risk of post hepatectomy liver failure. HPB (Oxford). 23:1807–1814. DOI: 10.1016/j.hpb.2021.04.014. PMID: 33975803.10. Bogner A, Reissfelder C, Striebel F, Mehrabi A, Ghamarnejad O, Rahbari M, et al. 2021; Intraoperative increase of portal venous pressure is an immediate predictor of posthepatectomy liver failure after major hepatectomy: a prospective study. Ann Surg. 274:e10–e17. DOI: 10.1097/SLA.0000000000003496. PMID: 31356261.11. Faitot F, Vibert E, Salloum C, Gorden DL, Coscas F, Adam R, et al. 2012; Importance of conserving middle hepatic vein distal branches for homogeneous regeneration of the left liver after right hepatectomy. HPB (Oxford). 14:746–753. DOI: 10.1111/j.1477-2574.2012.00514.x. PMID: 23043663. PMCID: PMC3482670.12. Morioka D, Tanaka K, Sekido H, Matsuo K, Sugita M, Ueda M, et al. 2006; Disruption of the middle hepatic vein is not crucial for liver regeneration of the remnant liver after right hemihepatectomy for hepatic tumors. Ann Surg Oncol. 13:1560–1568. DOI: 10.1245/s10434-006-9087-8. PMID: 17024557.13. Scatton O, Plasse M, Dondero F, Vilgrain V, Sauvanet A, Belghiti J. 2008; Impact of localized congestion related to venous deprivation after hepatectomy. Surgery. 143:483–489. DOI: 10.1016/j.surg.2007.11.002. PMID: 18374045.14. Sano T, Shimada K, Nara S, Sakamoto Y, Kosuge T. 2008; Reconstruction of hepatic venous tributaries using a Y-shaped left portal vein graft harvested from a resected left liver. Hepatogastroenterology. 55:228–230. PMID: 18507112.15. Mise Y, Hasegawa K, Satou S, Aoki T, Beck Y, Sugawara Y, et al. 2011; Venous reconstruction based on virtual liver resection to avoid congestion in the liver remnant. Br J Surg. 98:1742–1751. DOI: 10.1002/bjs.7670. PMID: 22034181.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic-assisted right hepatectomy via anterior approach for intrahepatic cholangiocarcinoma
- Portal vein embolization prior to hepatectomy: Techniques, outcomes and novel therapeutic approaches
- Analyzing bench-surgery time: A comparative study of pure laparoscopic and open left hepatectomy including the middle hepatic vein in living liver donors
- ALPPS in a patient with periductal infiltrating intrahepatic cholangiocarcinoma
- Parenchyma-preserving hepatectomy including segments I + IV resection and bile duct resection in a patient with type IV perihilar cholangiocarcinoma: A case report with video clip