Ann Surg Treat Res.
2022 Aug;103(2):87-95. 10.4174/astr.2022.103.2.87.
Impact of circumferential tumor location of mid to low rectal cancer on oncologic outcomes after preoperative chemoradiotherapy
- Affiliations
-
- 1Department of Surgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea
- KMID: 2532363
- DOI: http://doi.org/10.4174/astr.2022.103.2.87
Abstract
- Purpose
Some studies have suggested that circumferential tumor location (CTL) of rectal cancer may affect oncological outcomes. However, studies after preoperative chemoradiotherapy (CRT) are rare. This study aimed to evaluate the impact of CTL on oncologic outcomes of patients with mid to low rectal cancer who received preoperative CRT.
Methods
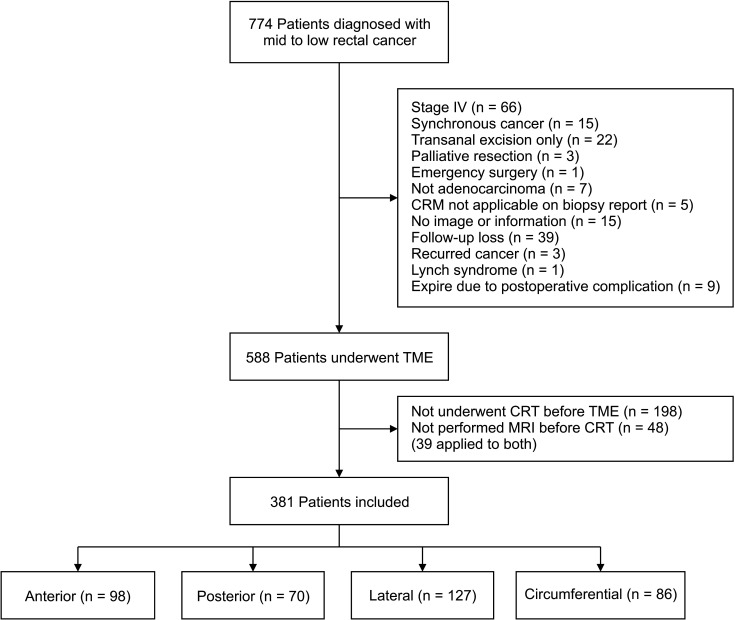
Patients with mid to low rectal cancer who underwent total mesorectal excision after CRT from January 2013 to December 2018 were included in this retrospective study. The impact of CTL on the pathological circumferential resection margin (CRM) status, local recurrence-free survival (LRFS), disease-free survival (DFS), and overall survival (OS) was analyzed.
Results
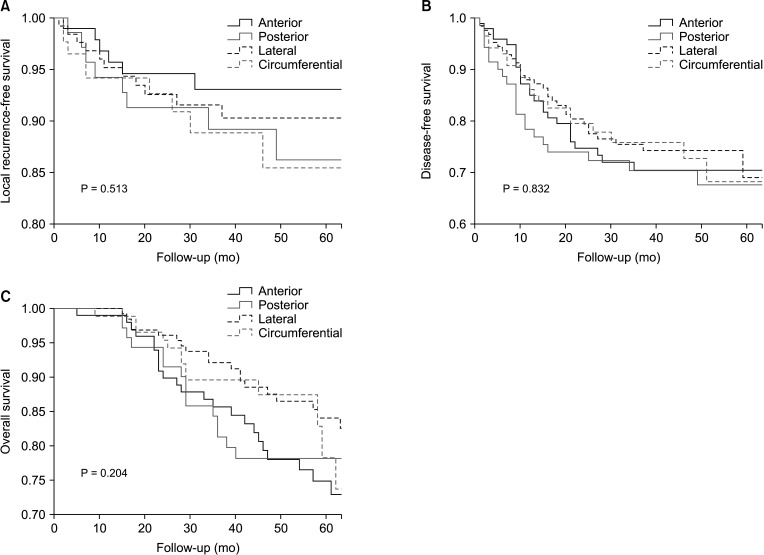
Of the 381 patients, 98, 70, 127, and 86 patients were categorized into the anterior, posterior, lateral, and circumferential tumor groups, respectively. Tumor location was not significantly associated with the pathological CRM involvement (anterior, 12.2% vs. posterior, 14.3% vs. lateral, 11.0% vs. circumferential, 17.4%; P = 0.232). Univariate analyses revealed no correlation between CTL and 3-year LRFS (93.0% vs. 89.1% vs. 91.5% vs. 88%, P = 0.513), 3-year DFS (70.3% vs. 70.2% vs. 75.3% vs. 75.7%, P = 0.832), and 5-year OS (74.7% vs. 78.0% vs. 83.9% vs. 78.2%, P = 0.204). Multivariate analysis identified low rectal cancer and pathological CRM involvement as independent risk factors for all survival outcomes (all P < 0.05).
Conclusion
CTL of rectal cancer after preoperative CRT was not significantly associated with the pathological CRM status, recurrence, and survival.
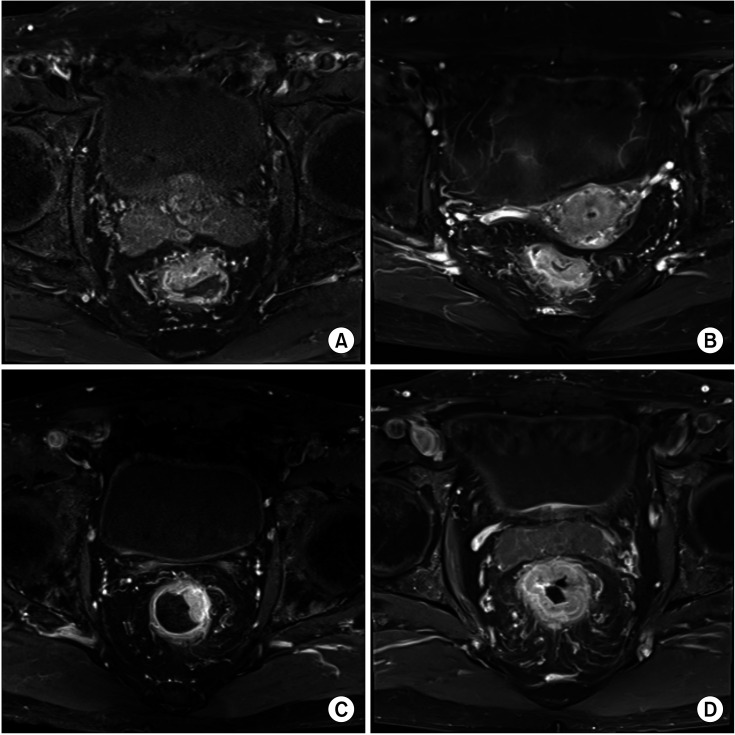
Figure
Reference
-
1. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998; 133:894–899. PMID: 9711965.2. Kapiteijn E, Putter H, van de Velde CJ. Cooperative investigators of the Dutch ColoRectal Cancer Group. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg. 2002; 89:1142–1149. PMID: 12190680.
Article3. Wibe A, Møller B, Norstein J, Carlsen E, Wiig JN, Heald RJ, et al. A national strategic change in treatment policy for rectal cancer: implementation of total mesorectal excision as routine treatment in Norway: a national audit. Dis Colon Rectum. 2002; 45:857–866. PMID: 12130870.
Article4. Banwell VC, Phillips HA, Duff MJ, Speake D, McLean C, Williams LJ, et al. Five-year oncological outcomes after selective neoadjuvant radiotherapy for resectable rectal cancer. Acta Oncol. 2019; 58:1267–1272. PMID: 31237192.
Article5. Dassanayake BK, Samita S, Deen RY, Wickramasinghe NS, Hewavisenthi J, Deen KI. Local recurrence of rectal cancer in patients not receiving neoadjuvant therapy: the importance of resection margins. Ceylon Med J. 2011; 56:159–161. PMID: 22298209.
Article6. Augestad KM, Lindsetmo RO, Stulberg J, Reynolds H, Senagore A, Champagne B, et al. International preoperative rectal cancer management: staging, neoadjuvant treatment, and impact of multidisciplinary teams. World J Surg. 2010; 34:2689–2700. PMID: 20703471.
Article7. Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. NCCN guidelines insights: rectal cancer, version 6.2020. J Natl Compr Canc Netw. 2020; 18:806–815. PMID: 32634771.
Article8. Jhaveri KS, Hosseini-Nik H. MRI of rectal cancer: an overview and update on recent advances. AJR Am J Roentgenol. 2015; 205:W42–W55. PMID: 26102418.
Article9. Kang BM, Park YK, Park SJ, Lee KY, Kim CW, Lee SH. Does circumferential tumor location affect the circumferential resection margin status in mid and low rectal cancer? Asian J Surg. 2018; 41:257–263. PMID: 28118954.
Article10. Lindsey I, Guy RJ, Warren BF, Mortensen NJ. Anatomy of Denonvilliers’ fascia and pelvic nerves, impotence, and implications for the colorectal surgeon. Br J Surg. 2000; 87:1288–1299. PMID: 11044153.
Article11. Chan CL, Bokey EL, Chapuis PH, Renwick AA, Dent OF. Local recurrence after curative resection for rectal cancer is associated with anterior position of the tumour. Br J Surg. 2006; 93:105–112. PMID: 16302179.
Article12. Franz C, Lang HM, Ghamarnejad O, Khajeh E, Mehrabi A, Ulrich A, et al. Prognostic impact of ventral versus dorsal tumor location after total mesorectal excision of rectal cancer. Ann Surg Oncol. 2020; 27:430–438. PMID: 31549320.
Article13. García-Granero E, Faiz O, Flor-Lorente B, García-Botello S, Esclápez P, Cervantes A. Prognostic implications of circumferential location of distal rectal cancer. Colorectal Dis. 2011; 13:650–657. PMID: 20236143.
Article14. Lee SH, Hernandez de Anda E, Finne CO, Madoff RD, Garcia-Aguilar J. The effect of circumferential tumor location in clinical outcomes of rectal cancer patients treated with total mesorectal excision. Dis Colon Rectum. 2005; 48:2249–2257. PMID: 16400512.
Article15. Wang X, Chen G, Zhang Y, Ghareeb WM, Yu Q, Zhu H, et al. The impact of circumferential tumour location on the clinical outcome of rectal cancer patients managed with neoadjuvant chemoradiotherapy followed by total mesorectal excision. Eur J Surg Oncol. 2020; 46:1118–1123. PMID: 32113887.
Article16. MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet. 1993; 341:457–460. PMID: 8094488.
Article17. Weiser MR. AJCC 8th edition: colorectal cancer. Ann Surg Oncol. 2018; 25:1454–1455. PMID: 29616422.
Article18. Rödel C, Martus P, Papadoupolos T, Füzesi L, Klimpfinger M, Fietkau R, et al. Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol. 2005; 23:8688–8696. PMID: 16246976.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impairment of Immunonutritional Status During Treatment is a Factor Associated With Oncologic Outcomes in Patients With Rectal Cancer Treated With Preoperative Chemoradiotherapy
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Abdominoperineal Resection in the Treatment of Locally-advanced Low Rectal Cancer: Is Preoperative Chemoradiation Advantageous?
- Long-term oncologic outcomes in pathologic tumor response after neoadjuvant chemoradiation for locally advanced rectal cancer
- Results of Preoperative Chemoradiotherapy in Low Rectal Cancer