Korean Circ J.
2022 Aug;52(8):593-603. 10.4070/kcj.2021.0399.
Association of Gender With Clinical Outcomes in a Contemporary Cohort of Patients With Atrial Fibrillation Receiving Oral Anticoagulants
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Myongji Hospital, Goyang, Korea
- 2Heart Institute, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University, Seoul, Korea
- 4Department of Cardiology, School of Medicine, Ewha Womans University, Seoul, Korea
- 5Department of Cardiology, Hanyang University Seoul Hospital, Seoul, Korea
- 6Division of Cardiology, Eulji University Hospital, Daejeon, Korea
- 7Division of Cardiology, Department of Internal Medicine, Korea University Medical Center, Seoul, Korea
- 8Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 9Division of Cardiology, Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu, Korea
- 10Division of Cardiology, Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea
- 11Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2532329
- DOI: http://doi.org/10.4070/kcj.2021.0399
Abstract
- Background and Objectives
In patients with atrial fibrillation (AF), females taking vitamin K antagonist are at higher risk of stroke or systemic embolism (SSE), bleeding and all-cause death than males. This study investigated the relationship between sex and adverse clinical events in a contemporary AF patient cohort taking anticoagulation.
Methods
This prospective multicenter AF registry study comprised 6,067 patients with AF (mean age, 70±9 years; men, 59%) with intermediate to high risk of stroke (CHA 2 DS 2-VAscore ≥1) and receiving oral anticoagulation therapy. Adverse clinical outcomes, including SSE, bleeding, death were evaluated in patients stratified by sex and anticoagulation patterns.
Results
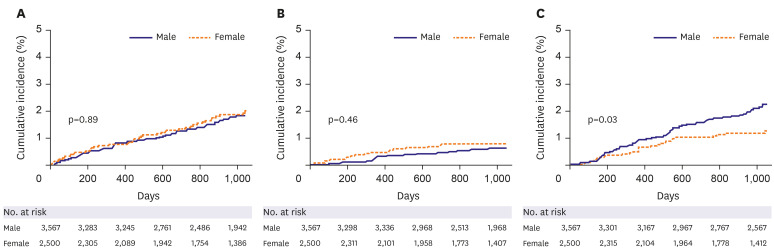
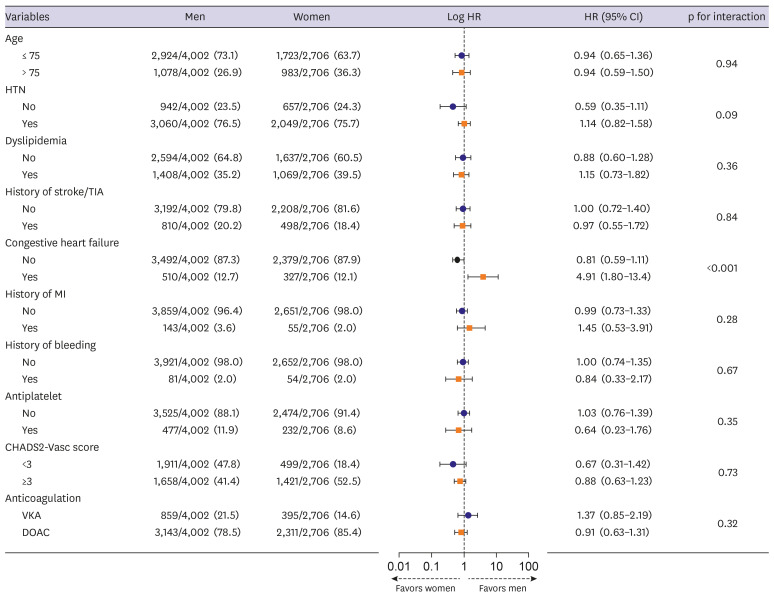
Women were older and used more direct oral anticoagulants (85% vs. 78%, p<0.001) than men. During a median (25 the and 75 the percentiles) follow-up of 30 (24, 38) months, the incidence rate and risk of SSE (0.7 in women vs. 0.7 in men per 100 person-years) and major bleeding (0.1 in women vs. 0.1 in men per 100 person-years) were not different between the sexes. However, women had a lower all-cause death rate (0.4 in women vs. 0.6 in men per 100 person-years, hazard ratio: 0.48, 95% confidence interval: 0.25–0.91, p=0.025) than men.
Conclusions
In contemporary anticoagulation for AF, SSE and major bleeding risks did not differ between sexes. However, women showed a lower risk of all-cause death rate than men, indicating that the use of oral anticoagulants for treating AF in females does not appear to be a risk factor for adverse clinical events.
Keyword
Figure
Cited by 2 articles
-
A ‘Gender Paradox’ of Female as a Stroke Risk in Atrial Fibrillation: Do Women Live Longer Than Men?
Joo Hee Jeong, Jong-Il Choi
Korean Circ J. 2022;52(8):604-605. doi: 10.4070/kcj.2022.0175.What Is a Balanced Way of Anticoagulation for Efficacy and Safety in High-Risk Elderly Patients With Atrial Fibrillation?
Daehoon Kim
Korean Circ J. 2024;54(7):407-408. doi: 10.4070/kcj.2024.0170.
Reference
-
1. Kim D, Yang PS, Jang E, et al. 10-year nationwide trends of the incidence, prevalence, and adverse outcomes of non-valvular atrial fibrillation nationwide health insurance data covering the entire Korean population. Am Heart J. 2018; 202:20–26. PMID: 29802976.
Article2. Kim D, Yang PS, Jang E, et al. Increasing trends in hospital care burden of atrial fibrillation in Korea, 2006 through 2015. Heart. 2018; 104:2010–2017. PMID: 29666179.
Article3. Joung B, Lee JM, Lee KH, et al. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018; 48:1033–1080. PMID: 30403013.
Article4. Yoon M, Yang PS, Jang E, et al. Dynamic changes of CHA2DS2-VASc score and the risk of ischaemic stroke in Asian patients with atrial fibrillation: a nationwide cohort study. Thromb Haemost. 2018; 118:1296–1304. PMID: 29723875.
Article5. Ko D, Rahman F, Schnabel RB, Yin X, Benjamin EJ, Christophersen IE. Atrial fibrillation in women: epidemiology, pathophysiology, presentation, and prognosis. Nat Rev Cardiol. 2016; 13:321–332. PMID: 27053455.
Article6. Emdin CA, Wong CX, Hsiao AJ, et al. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ. 2016; 532:h7013. PMID: 26786546.
Article7. Yong CM, Tremmel JA, Lansberg MG, Fan J, Askari M, Turakhia MP. Sex differences in oral anticoagulation and outcomes of stroke and intracranial bleeding in newly diagnosed atrial fibrillation. J Am Heart Assoc. 2020; 9:e015689. PMID: 32394763.
Article8. Poli D, Antonucci E, Testa S, Ageno W, Palareti G. FCSA (Italian Federation of Anticoagulation Clinics). Gender differences of bleeding and stroke risk in very old atrial fibrillation patients on VKA treatment: results of the EPICA study on the behalf of FCSA (Italian Federation of Anticoagulation Clinics). Thromb Res. 2013; 131:12–16. PMID: 23141847.
Article9. Pancholy SB, Sharma PS, Pancholy DS, Patel TM, Callans DJ, Marchlinski FE. Meta-analysis of gender differences in residual stroke risk and major bleeding in patients with nonvalvular atrial fibrillation treated with oral anticoagulants. Am J Cardiol. 2014; 113:485–490. PMID: 24315113.
Article10. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962. PMID: 24315724.
Article11. Haas S, Camm AJ, Bassand JP, et al. GARFIELD-AF Investigators. Predictors of NOAC versus VKA use for stroke prevention in patients with newly diagnosed atrial fibrillation: results from GARFIELD-AF. Am Heart J. 2019; 213:35–46. PMID: 31128503.
Article12. Lee SR, Lee YS, Park JS, et al. Label adherence for non-vitamin K antagonist oral anticoagulants in a prospective cohort of Asian patients with atrial fibrillation. Yonsei Med J. 2019; 60:277–284. PMID: 30799590.
Article13. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962. PMID: 27567408.
Article14. Steffel J, Verhamme P, Potpara TS, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation: executive summary. Europace. 2018; 20:1231–1242. PMID: 29562331.
Article15. Kim H, Kim TH, Cha MJ, et al. A prospective survey of atrial fibrillation management for real-world guideline adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Registry. Korean Circ J. 2017; 47:877–887. PMID: 29171211.
Article16. Takabayashi K, Hamatani Y, Yamashita Y, et al. Incidence of stroke or systemic embolism in paroxysmal versus sustained atrial fibrillation: the Fushimi atrial fibrillation registry. Stroke. 2015; 46:3354–3361. PMID: 26514188.
Article17. Sullivan RM, Zhang J, Zamba G, Lip GY, Olshansky B. Relation of gender-specific risk of ischemic stroke in patients with atrial fibrillation to differences in warfarin anticoagulation control (from AFFIRM). Am J Cardiol. 2012; 110:1799–1802. PMID: 22995971.
Article18. Pokorney SD, Simon DN, Thomas L, et al. Patients’ time in therapeutic range on warfarin among US patients with atrial fibrillation: results from ORBIT-AF registry. Am Heart J. 2015; 170:141–148. 148.e1PMID: 26093875.
Article19. Lee JM, Kim TH, Cha MJ, et al. Gender-related differences in management of nonvalvular atrial fibrillation in an Asian population. Korean Circ J. 2018; 48:519–528. PMID: 29856147.
Article20. Dalgaard F, Xu H, Matsouaka RA, et al. Management of atrial fibrillation in older patients by morbidity burden: insights from get with the guidelines-atrial fibrillation. J Am Heart Assoc. 2020; 9:e017024. PMID: 33241750.
Article21. Law SW, Lau WC, Wong IC, et al. Sex-based differences in outcomes of oral anticoagulation in patients with atrial fibrillation. J Am Coll Cardiol. 2018; 72:271–282. PMID: 30012320.
Article22. Yu HT, Yang PS, Hwang J, et al. Social inequalities of oral anticoagulation after the introduction of non-vitamin K antagonists in patients with atrial fibrillation. Korean Circ J. 2020; 50:267–277. PMID: 32100483.
Article23. Afzal S, Zaidi ST, Merchant HA, Babar ZU, Hasan SS. Prescribing trends of oral anticoagulants in England over the last decade: a focus on new and old drugs and adverse events reporting. J Thromb Thrombolysis. 2021; 52:646–653. PMID: 33666824.
Article24. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021; 42:373–498. PMID: 32860505.25. van Rein N, Heide-Jørgensen U, Lijfering WM, Dekkers OM, Sørensen HT, Cannegieter SC. Major bleeding rates in atrial fibrillation patients on single, dual, or triple antithrombotic therapy. Circulation. 2019; 139:775–786. PMID: 30586754.
Article26. Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010; 170:1433–1441. PMID: 20837828.
Article27. Wilkinson C, Wu J, Searle SD, et al. Clinical outcomes in patients with atrial fibrillation and frailty: insights from the ENGAGE AF-TIMI 48 trial. BMC Med. 2020; 18:401. PMID: 33357217.
Article28. Dalgaard F, Pieper K, Verheugt F, et al. GARFIELD-AF model for prediction of stroke and major bleeding in atrial fibrillation: a Danish nationwide validation study. BMJ Open. 2019; 9:e033283.
Article29. Huisman MV, Rothman KJ, Paquette M, et al. The changing landscape for stroke prevention in AF: findings from the GLORIA-AF registry phase 2. J Am Coll Cardiol. 2017; 69:777–785. PMID: 28209218.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oral Anticoagulants for Atrial Fibrillation Patients with Active Cancer
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- New oral anticoagulants
- Stroke Prevention in Atrial Fibrillation
- Application of New Oral Anticoagulants: Prevention of Stroke in Patients with Nonvalvular Atrial Fibrillation