J Korean Med Sci.
2022 Aug;37(31):e245. 10.3346/jkms.2022.37.e245.
National Implementation of Emergency Department-Based Followup Program for Suicidal Attempts
- Affiliations
-
- 1Department of Emergency Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 2Laboratory of Emergency Medical Services, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea
- 3Department of Emergency Medicine, Seoul National University College of Medicine and Hospital, Seoul, Korea
- 4Ministry of Health and Welfare, Sejong, Korea
- KMID: 2532320
- DOI: http://doi.org/10.3346/jkms.2022.37.e245
Abstract
- Background
Death by suicide is a major public health problem. To provide multidisciplinary support to patients who attempted suicide, emergency department (ED)-based psychiatric screening and intervention programs were offered. We traced the long-term survival outcome of patients visiting the ED after suicide attempts using the national death certificate registration database.
Methods
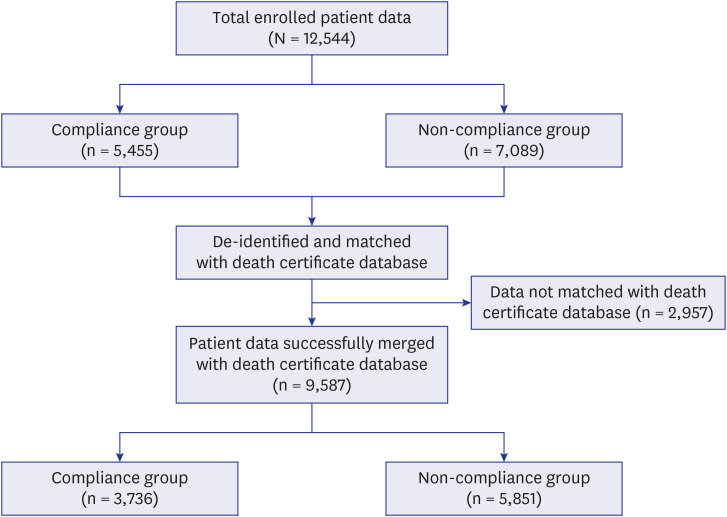
A retrospective observational study was conducted using a database of patients from “Psychiatric Crisis Response Centers” (PCRC) of 27 EDs between January 2013 and August 2015. Patients who visited the ED after attempting suicide were screened and interviewed by social workers from the PCRC. The database was merged with the national death certificate database to trace the death and cause of death of the patients until December 2018. The characteristics and outcomes were compared based on the patient’s compliance with the follow-up case management program.
Results
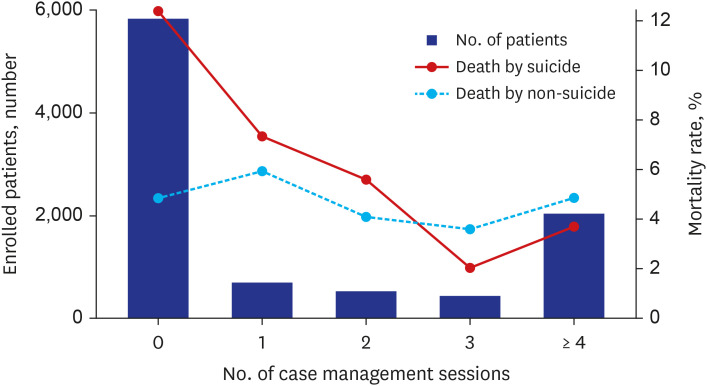
Of the 12,544 interviewed patients, the data of 9,587 patients were successfully matched with data from the death certificate database. Death by suicide was higher in the noncompliance group (4.5% vs. 12.4%, P < 0.001); however, death caused by factors other than suicide did not differ between groups (4.8% vs. 4.9%, P = 0.906).
Conclusion
Suicide resulted in a lower long-term mortality rate among patients who complied with the follow-up case management session in the ED-based brief psychiatric intervention and follow-up program.
Keyword
Figure
Reference
-
1. World Health Organization. Public Health Action for the Prevention of Suicide: A Framework. Geneva, Switzerland: World Health Organization;2012.2. Biddle L, Brock A, Brookes ST, Gunnell D. Suicide rates in young men in England and Wales in the 21st century: time trend study. BMJ. 2008; 336(7643):539–542. PMID: 18276666.
Article3. Brown JF. Psychiatric emergency services: a review of the literature and a proposed research agenda. Psychiatr Q. 2005; 76(2):139–165. PMID: 15884742.
Article4. Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019; 143(4):e20182192. PMID: 30886112.
Article5. Asarnow JR, Baraff LJ, Berk M, Grob CS, Devich-Navarro M, Suddath R, et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv. 2011; 62(11):1303–1309. PMID: 22211209.
Article6. Stanley B, Brown GK, Currier GW, Lyons C, Chesin M, Knox KL. Brief intervention and follow-up for suicidal patients with repeat emergency department visits enhances treatment engagement. Am J Public Health. 2015; 105(8):1570–1572. PMID: 26066951.
Article7. Frosch E, dosReis S, Maloney K. Connections to outpatient mental health care of youths with repeat emergency department visits for psychiatric crises. Psychiatr Serv. 2011; 62(6):646–649. PMID: 21632734.
Article8. Currier GW, Fisher SG, Caine ED. Mobile crisis team intervention to enhance linkage of discharged suicidal emergency department patients to outpatient psychiatric services: a randomized controlled trial. Acad Emerg Med. 2010; 17(1):36–43. PMID: 20015106.
Article9. Na KS, Park SC, Kwon SJ, Kim M, Kim HJ, Baik M, et al. Contents of the standardized suicide prevention program for gatekeeper intervention in Korea, version 2.0. Psychiatry Investig. 2020; 17(11):1149–1157.
Article10. Korea Foundation for Suicide Prevention. Emergency department based psychiatric brief intervention and follow-up program. Updated 2022. Accessed July 22, 2022. https://kfsp.org/sub.php?id=business&mode=view&menukey=8&idx=13&page=1&menukey=8 .11. Michiels EA, Dumas F, Quan L, Selby L, Copass M, Rea T. Long-term outcomes following pediatric out-of-hospital cardiac arrest. Pediatr Crit Care Med. 2013; 14(8):755–760. PMID: 23925145.
Article12. Gerson R, Havens J, Marr M, Storfer-Isser A, Lee M, Rojas Marcos C, et al. Utilization patterns at a specialized children’s comprehensive psychiatric emergency program. Psychiatr Serv. 2017; 68(11):1104–1111. PMID: 28617206.
Article13. Zeller SL, Rieger SM. Models of psychiatric emergency care. Curr Emerg Hosp Med Rep. 2015; 3(4):169–175.
Article14. Knox KL, Stanley B, Currier GW, Brenner L, Ghahramanlou-Holloway M, Brown G. An emergency department-based brief intervention for veterans at risk for suicide (SAFE VET). Am J Public Health. 2012; 102(Suppl 1):S33–S37. PMID: 22390597.
Article15. D’Onofrio G, Fiellin DA, Pantalon MV, Chawarski MC, Owens PH, Degutis LC, et al. A brief intervention reduces hazardous and harmful drinking in emergency department patients. Ann Emerg Med. 2012; 60(2):181–192. PMID: 22459448.
Article16. Kim B, Ahn JH, Cha B, Chung YC, Ha TH, Hong Jeong S, et al. Characteristics of methods of suicide attempts in Korea: Korea National Suicide Survey (KNSS). J Affect Disord. 2015; 188:218–225. PMID: 26368946.
Article17. Owens PL, Mutter R, Stocks C. Mental health and substance abuse-related emergency department visits among adults, 2007. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, USA: Agency for Healthcare Research and Quality;2010.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors related to Suicidal Ideation in People with Schizophrenia and Suicide Attempts
- Factors associated with suicide attempts among Korean older adults in community: A quantitative study using data from the 2021 Community Health Survey
- Associated Factors of Suicidal Ideation in Community Residents with Suicidal Attempt Experiences
- Combined Influence of Smoking and Alcohol Drinking on Suicidal Ideation and Attempts among Korean Adults: Using Data from the Korean National Health and Nutrition Examination Survey 2008~2011
- Gender difference in socioeconomic factors affecting suicidal ideation and suicidal attempts among community-dwelling elderly: based on the Korea Community Health Survey