J Neurocrit Care.
2022 Jun;15(1):61-64. 10.18700/jnc.220051.
Urgent decompression of tension pneumomediastinum in a patient to relieve elevated intracranial pressure: a case report
- Affiliations
-
- 1Division of Neurocritical Care, Department of Neurology and Neurosurgery, University of Texas Southwestern Medical Center, Dallas, TX, USA
- 2Department of Otolaryngology-Head and Neck Surgery, University of Texas Southwestern Medical Center, Dallas, TX, USA
- 3Division of Pulmonary Critical Care, Department of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, TX, USA
- KMID: 2532002
- DOI: http://doi.org/10.18700/jnc.220051
Abstract
- Background
Timely recognition and intervention for venous outflow obstruction due to intrathoracic pathology are critical for controlling elevated intracranial pressure.
Case Report
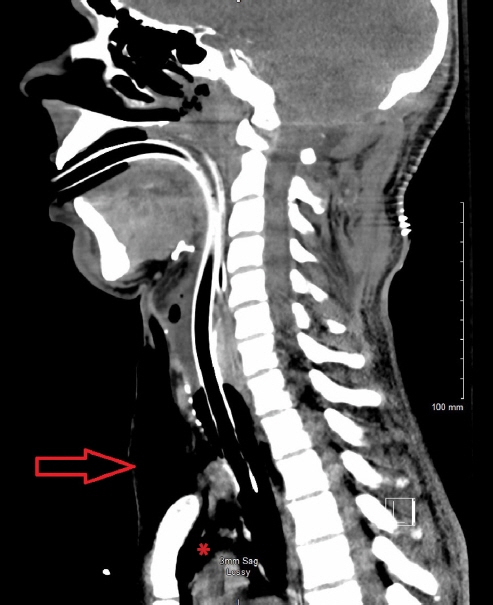
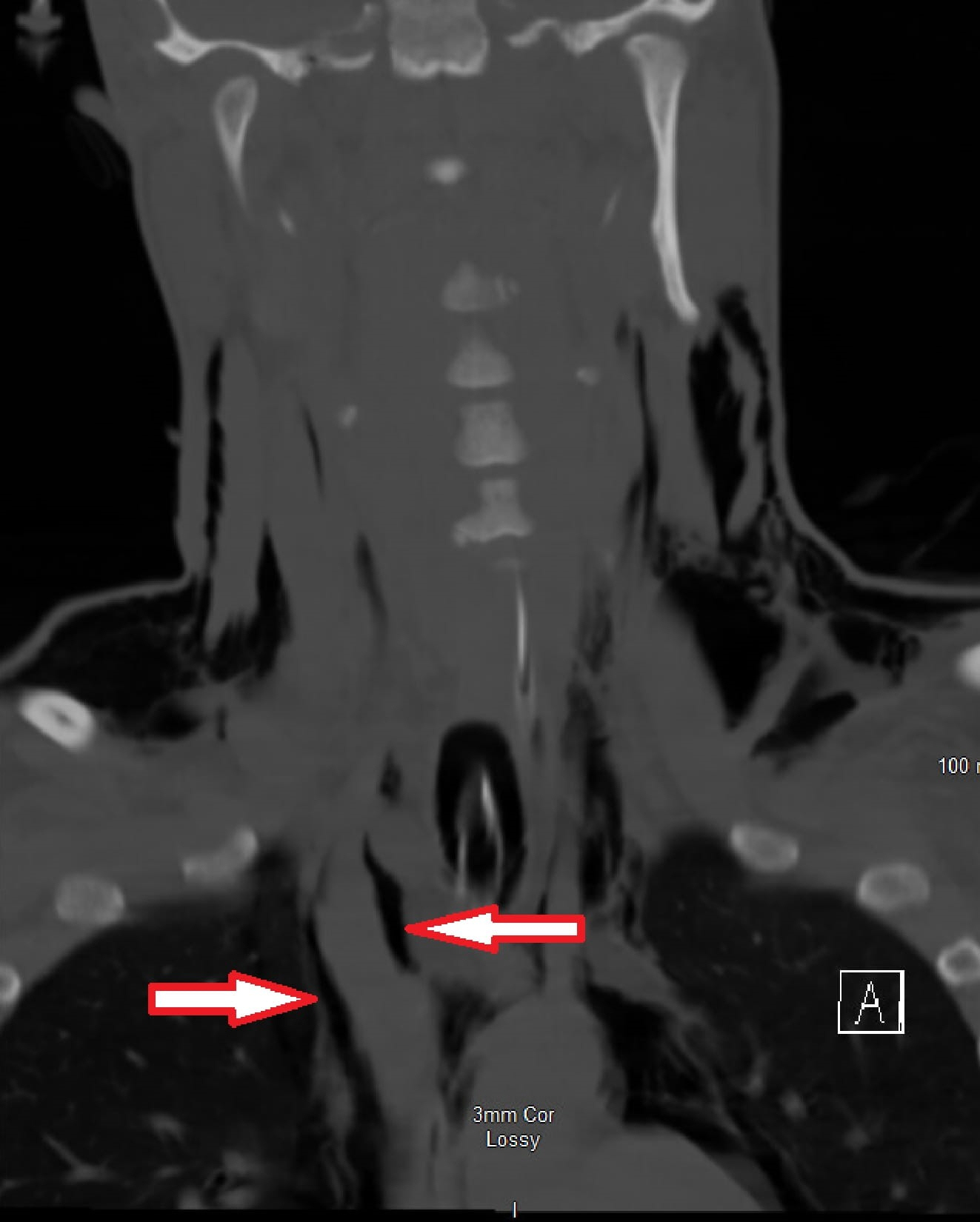
A 26-year-old man with pectus excavatum and a posterior fossa tumor requiring biopsy, decompression, and cerebrospinal fluid diversion developed pneumomediastinum following intubation with tension physiology and progressive elevation of intracranial pressure. Emergent tracheostomy was performed to decompress intrathoracic pressure, augment venous return, and ultimately expedite the patient’s definitive cancer therapy.
Conclusion
Recognition of the mediastinal pathology leading to venous obstruction may be required for the management of malignant intracranial hypertension. Tracheostomy may be a means to decompress mediastinal pressure and augment venous outflow in rare cases of pneumomediastinum with tension physiology.
Keyword
Figure
Reference
-
1. Durward QJ, Amacher AL, Del Maestro RF, Sibbald WJ. Cerebral and cardiovascular responses to changes in head elevation in patients with intracranial hypertension. J Neurosurg. 1983; 59:938–44.
Article2. Karanjia N, Nordquist D, Stevens R, Nyquist P. A clinical description of extubation failure in patients with primary brain injury. Neurocrit Care. 2011; 15:4–12.
Article3. McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129(1 Suppl):48S–53S.4. Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008; 19:691–707.
Article5. Macklin CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implications. Arch Intern Med. 1939; 64:913–26.
Article6. Cummings RG, Wesly RL, Adams DH, Lowe JE. Pneumopericardium resulting in cardiac tamponade. Ann Thorac Surg. 1984; 37:511–8.
Article7. el Gamel A, Barrett P, Kopff G. Pneumopericardium: a rare cause of cardiac tamponade in an infant on a positive pressure ventilation. Acta Paediatr. 1994; 83:1220–1.
Article8. Shennib HF, Barkun AN, Matouk E, Blundell PE. Surgical decompression of a tension pneumomediastinum: a ventilatory complication of status asthmaticus. Chest. 1988; 93:1301–2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Split-Thickness Decompression in the Management of Intracranial Pressure
- What should an intensivist know about pneumocephalus and tension pneumocephalus?
- Respiratory Arrest due to Tension Pneumoperitoneum and Pneumomediastinum without Pneumothorax: Complication of the Lumbar Spinal Surgery
- Pneumomediastinum and Subcutaneous Emphysema after Use of Metallic Endotracheal Tube for Laser Operation: A case report
- Tension pneumoperitoneum during pneumatic reduction of pediatric intussusception: case report