Clin Endosc.
2022 Jul;55(4):570-573. 10.5946/ce.2021.175.
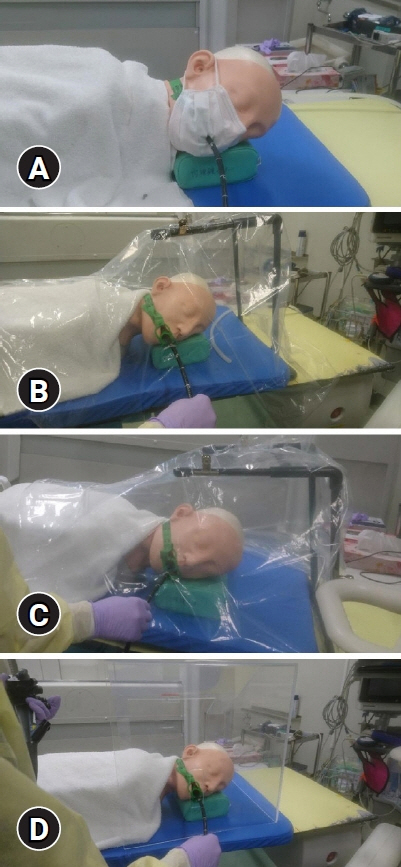
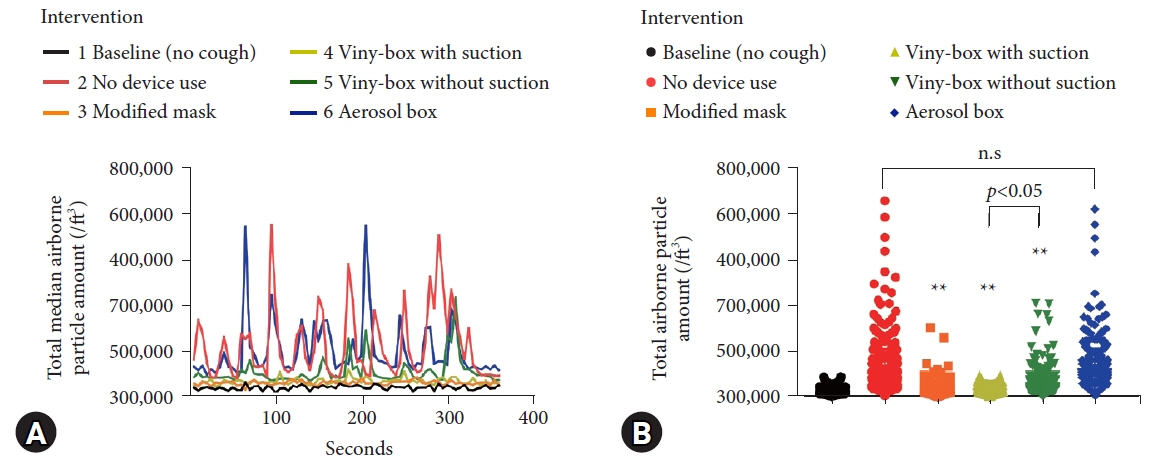
A comparison of the effectiveness of four aerosol shielding devices in reducing endoscopists’ exposure to airborne particles during simulated upper gastrointestinal endoscopy
- Affiliations
-
- 1Department of Gastroenterology, Osaka City University Graduate School of Medicine, Osaka, Japan
- KMID: 2531952
- DOI: http://doi.org/10.5946/ce.2021.175
Figure
Reference
-
1. Chan SM, Ma TW, Chong MK-C, et al. A proof of concept study: esophagogastroduodenoscopy is an aerosol-generating procedure and continuous oral suction during the procedure reduces the amount of aerosol generated. Gastroenterology. 2020; 159:1949–1951.2. Sagami R, Nishikiori H, Sato T, et al. Endoscopic shield: barrier enclosure during the endoscopy to prevent aerosol droplets during the COVID-19 pandemic. VideoGIE. 2020; 5:445–448.3. Kobara H, Nishiyama N, Masaki T. Shielding for patients using a single-use vinyl-box under continuous aerosol suction to minimize SARS-CoV-2 transmission during emergency endoscopy. Dig Endosc. 2020; 32:e114–e115.4. Endo H, Koike T, Masamune A. Novel device for preventing diffusion of aerosol droplets from subjects undergoing esophagogastroduodenoscopy during COVID-19 pandemic. Dig Endosc. 2020; 32:e140–e141.5. Maruyama H, Higashimori A, Yamamoto K, et al. Coronavirus disease outbreak: a simple infection prevention measure using a surgical mask during endoscopy. Endoscopy. 2020; 52:E461–E462.6. Canelli R, Connor CW, Gonzalez M, et al. Barrier enclosure during endotracheal intubation. N Engl J Med. 2020; 382:1957–1958.7. Gupta JK, Lin CH, Chen Q. Flow dynamics and characterization of a cough. Indoor Air. 2009; 19:517–525.8. Simpson JP, Wong DN, Verco L, et al. Measurement of airborne particle exposure during simulated tracheal intubation using various proposed aerosol containment devices during the COVID-19 pandemic. Anaesthesia. 2020; 75:1587–1595.9. Dalli J, Khan MF, Marsh B, et al. Evaluating intubation boxes for airway management. Br J Anaesth. 2020; 125:e293–e295.10. U.S. Food and Drug Administration (FDA). Protective barrier enclosures without negative pressure used during the COVID-19 pandemic may increase risk to patients and health care providers: letter to health care providers [Internet]. Silver Spring (MD): FDA;2020. [updated 2020 Aug 21; cited 2021 Aug 4]. Available from: https://www.fda.gov/medical-devices/letters-health-care-providers/protective-barrier-enclosures-without-negative-pressure-used-during-covid-19-pandemic-may-increase.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aerosol protection using modified N95 respirator during upper gastrointestinal endoscopy: a randomized controlled trial
- Observable Laryngopharyngeal Lesions during the Upper Gastrointestinal Endoscopy
- Management of aerosol generation during upper gastrointestinal endoscopy
- Preclinical Efficacy and Clinical Feasibility of a Novel Aerosol-Exposure Protection Mask for Esophagogastroduodenoscopy
- A Novel Aerosol-Exposure Protection Mask for Patients During Upper Endoscopy