Child Kidney Dis.
2022 Jun;26(1):25-30. 10.3339/ckd.22.020.
Mechanism, clinical consequences, and management of dyslipidemia in children with nephrotic syndrome
- Affiliations
-
- 1Department of Pediatrics, Yeungnam University College of Medicine, Daegu, Republic of Korea
- KMID: 2531931
- DOI: http://doi.org/10.3339/ckd.22.020
Abstract
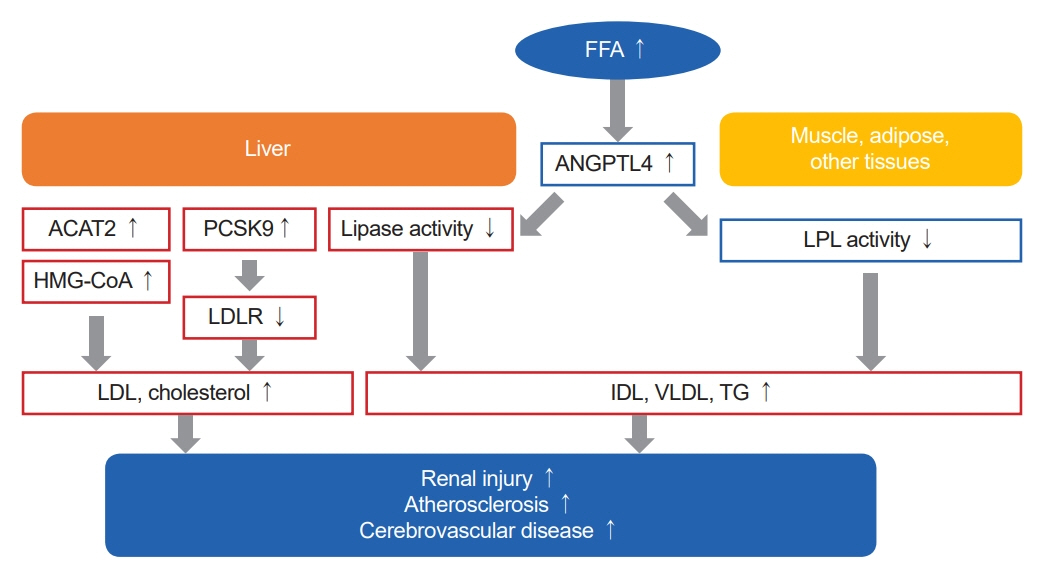
- Dyslipidemia in nephrotic syndrome (NS) is often characterized by marked increases in the levels of total cholesterol, triglycerides, low-density lipoprotein cholesterol, and other lipoproteins, such as very low-density lipoprotein, intermediate-density lipoprotein, and lipoprotein(a). It has been suggested that impaired catabolism of lipoproteins and cholesterol is mainly due to decreased lipoprotein lipase and hepatic lipase activity, and increased biosynthesis of lipoproteins in the liver. The management strategies for dyslipidemia in patients with NS consist of lifestyle modification, lipid-lowering agents represented by statins, second-line agents such as fibrates and bile acid sequestrants, and lipid apheresis. Compared with dyslipidemia in adult NS patients, whose risks of atherosclerotic disease and progressive renal injury are considered high, clinical data on dyslipidemia in pediatric NS patients are limited. Therefore, it is necessary to pay more attention to the evaluation and management of dyslipidemia in pediatric patients with NS in clinical practice.
Keyword
Figure
Reference
-
References
1. Larkins NG, Liu ID, Willis NS, Craig JC, Hodson EM. Non-corticosteroid immunosuppressive medications for steroid-sensitive nephrotic syndrome in children. Cochrane Database Syst Rev. 2020; 4:CD002290.
Article2. Kang HG, Cheong HI. Nephrotic syndrome: what’s new, what’s hot? Korean J Pediatr. 2015; 58:275–82.
Article3. Agrawal S, Zaritsky JJ, Fornoni A, Smoyer WE. Dyslipidaemia in nephrotic syndrome: mechanisms and treatment. Nat Rev Nephrol. 2018; 14:57–70.
Article4. Vaziri ND. Disorders of lipid metabolism in nephrotic syndrome: mechanisms and consequences. Kidney Int. 2016; 90:41–52.
Article5. Vaziri ND, Yuan J, Ni Z, Nicholas SB, Norris KC. Lipoprotein lipase deficiency in chronic kidney disease is accompanied by down-regulation of endothelial GPIHBP1 expression. Clin Exp Nephrol. 2012; 16:238–43.
Article6. Sato T, Liang K, Vaziri ND. Down-regulation of lipoprotein lipase and VLDL receptor in rats with focal glomerulosclerosis. Kidney Int. 2002; 61:157–62.
Article7. Liu S, Vaziri ND. Role of PCSK9 and IDOL in the pathogenesis of acquired LDL receptor deficiency and hypercholesterolemia in nephrotic syndrome. Nephrol Dial Transplant. 2014; 29:538–43.
Article8. Morris AW. Nephrotic syndrome: PCSK9: a target for hypercholesterolaemia in nephrotic syndrome. Nat Rev Nephrol. 2016; 12:510.
Article9. Jin K, Park BS, Kim YW, Vaziri ND. Plasma PCSK9 in nephrotic syndrome and in peritoneal dialysis: a cross-sectional study. Am J Kidney Dis. 2014; 63:584–9.
Article10. Moorhead JF, Chan MK, El-Nahas M, Varghese Z. Lipid nephrotoxicity in chronic progressive glomerular and tubulo-interstitial disease. Lancet. 1982; 2:1309–11.
Article11. Clement LC, Mace C, Avila-Casado C, Joles JA, Kersten S, Chugh SS. Circulating angiopoietin-like 4 links proteinuria with hypertriglyceridemia in nephrotic syndrome. Nat Med. 2014; 20:37–46.
Article12. Vaziri ND, Liang K. Up-regulation of acyl-coenzyme A:cholesterol acyltransferase (ACAT) in nephrotic syndrome. Kidney Int. 2002; 61:1769–75.
Article13. Vaziri ND, Liang KH. Acyl-coenzyme A:cholesterol acyltransferase inhibition ameliorates proteinuria, hyperlipidemia, lecithin-cholesterol acyltransferase, SRB-1, and low-denisty lipoprotein receptor deficiencies in nephrotic syndrome. Circulation. 2004; 110:419–25.
Article14. Vaziri ND, Liang KH. Hepatic HMG-CoA reductase gene expression during the course of puromycin-induced nephrosis. Kidney Int. 1995; 48:1979–85.
Article15. Vaziri ND, Sato T, Liang K. Molecular mechanisms of altered cholesterol metabolism in rats with spontaneous focal glomerulosclerosis. Kidney Int. 2003; 63:1756–63.
Article16. Ordonez JD, Hiatt RA, Killebrew EJ, Fireman BH. The increased risk of coronary heart disease associated with nephrotic syndrome. Kidney Int. 1993; 44:638–42.
Article17. Mehta A, Mishra S, Ahmad K, Tiwari HC, Singh V, Singh A. Carotid intima media thickness in children with nephrotic syndrome: an observational case control study. Sudan J Paediatr. 2019; 19:110–6.
Article18. Radhakrishnan J, Appel AS, Valeri A, Appel GB. The nephrotic syndrome, lipids, and risk factors for cardiovascular disease. Am J Kidney Dis. 1993; 22:135–42.
Article19. Gyebi L, Soltani Z, Reisin E. Lipid nephrotoxicity: new concept for an old disease. Curr Hypertens Rep. 2012; 14:177–81.
Article20. Chung JJ, Huber TB, Godel M, Jarad G, Hartleben B, Kwoh C, et al. Albumin-associated free fatty acids induce macropinocytosis in podocytes. J Clin Invest. 2015; 125:2307–16.
Article21. Allison SJ. Podocyte biology: free fatty acid-induced macropinocytosis in podocytes. Nat Rev Nephrol. 2015; 11:386.
Article22. Eddy AA, Michael AF. Acute tubulointerstitial nephritis associated with aminonucleoside nephrosis. Kidney Int. 1988; 33:14–23.
Article23. Eddy AA, McCulloch L, Liu E, Adams J. A relationship between proteinuria and acute tubulointerstitial disease in rats with experimental nephrotic syndrome. Am J Pathol. 1991; 138:1111–23.24. Cases A, Coll E. Dyslipidemia and the progression of renal disease in chronic renal failure patients. Kidney Int Suppl. 2005; (99):S87–93.
Article25. D’Amico G, Gentile MG, Manna G, Fellin G, Ciceri R, Cofano F, et al. Effect of vegetarian soy diet on hyperlipidaemia in nephrotic syndrome. Lancet. 1992; 339:1131–4.
Article26. Gentile MG, Fellin G, Cofano F, Delle Fave A, Manna G, Ciceri R, et al. Treatment of proteinuric patients with a vegetarian soy diet and fish oil. Clin Nephrol. 1993; 40:315–20.27. Hall AV, Parbtani A, Clark WF, Spanner E, Huff MW, Philbrick DJ, et al. Omega-3 fatty acid supplementation in primary nephrotic syndrome: effects on plasma lipids and coagulopathy. J Am Soc Nephrol. 1992; 3:1321–9.
Article28. Bell S, Cooney J, Packard CJ, Caslake MJ, Deighan CJ. The effect of omega-3 fatty acids on the atherogenic lipoprotein phenotype in patients with nephrotic range proteinuria. Clin Nephrol. 2012; 77:445–53.
Article29. Rabelink AJ, Hene RJ, Erkelens DW, Joles JA, Koomans HA. Effects of simvastatin and cholestyramine on lipoprotein profile in hyperlipidaemia of nephrotic syndrome. Lancet. 1988; 2:1335–8.
Article30. Thomas ME, Harris KP, Ramaswamy C, Hattersley JM, Wheeler DC, Varghese Z, et al. Simvastatin therapy for hypercholesterolemic patients with nephrotic syndrome or significant proteinuria. Kidney Int. 1993; 44:1124–9.
Article31. Wheeler DC, Bernard DB. Lipid abnormalities in the nephrotic syndrome: causes, consequences, and treatment. Am J Kidney Dis. 1994; 23:331–46.
Article32. Massy ZA, Ma JZ, Louis TA, Kasiske BL. Lipid-lowering therapy in patients with renal disease. Kidney Int. 1995; 48:188–98.
Article33. Kong X, Yuan H, Fan J, Li Z, Wu T, Jiang L, et al. Lipid-lowering agents for nephrotic syndrome. Cochrane Database Syst Rev. 2013; (12):CD005425.
Article34. Brown CD, Azrolan N, Thomas L, Roberts KG, Bostom A, Zhao ZH, et al. Reduction of lipoprotein(a) following treatment with lovastatin in patients with unremitting nephrotic syndrome. Am J Kidney Dis. 1995; 26:170–7.
Article35. Khurana M, Silverstein DM. Etiology and management of dyslipidemia in children with chronic kidney disease and end-stage renal disease. Pediatr Nephrol. 2015; 30:2073–84.
Article36. Coleman JE, Watson AR. Hyperlipidaemia, diet and simvastatin therapy in steroid-resistant nephrotic syndrome of childhood. Pediatr Nephrol. 1996; 10:171–4.
Article37. Sanjad SA, al-Abbad A, al-Shorafa S. Management of hyperlipidemia in children with refractory nephrotic syndrome: the effect of statin therapy. J Pediatr. 1997; 130:470–4.
Article38. Groggel GC, Cheung AK, Ellis-Benigni K, Wilson DE. Treatment of nephrotic hyperlipoproteinemia with gemfibrozil. Kidney Int. 1989; 36:266–71.
Article39. Buyukcelik M, Anarat A, Bayazit AK, Noyan A, Ozel A, Anarat R, et al. The effects of gemfibrozil on hyperlipidemia in children with persistent nephrotic syndrome. Turk J Pediatr. 2002; 44:40–4.40. Jacobson TA. Myopathy with statin-fibrate combination therapy: clinical considerations. Nat Rev Endocrinol. 2009; 5:507–18.
Article41. Valeri A, Gelfand J, Blum C, Appel GB. Treatment of the hyperlipidemia of the nephrotic syndrome: a controlled trial. Am J Kidney Dis. 1986; 8:388–96.
Article42. Di Bartolo B, Scherer DJ, Brown A, Psaltis PJ, Nicholls SJ. PCSK9 inhibitors in hyperlipidemia: current status and clinical outlook. BioDrugs. 2017; 31:167–74.
Article43. Haas ME, Levenson AE, Sun X, Liao WH, Rutkowski JM, de Ferranti SD, et al. The role of proprotein convertase subtilisin/kexin type 9 in nephrotic syndrome-associated hypercholesterolemia. Circulation. 2016; 134:61–72.
Article44. Jatem E, Lima J, Montoro B, Torres-Bondia F, Segarra A. Efficacy and safety of PCSK9 inhibitors in hypercholesterolemia associated with refractory nephrotic syndrome. Kidney Int Rep. 2020; 6:101–9.45. Hattori M, Chikamoto H, Akioka Y, Nakakura H, Ogino D, Matsunaga A, et al. A combined low-density lipoprotein apheresis and prednisone therapy for steroid-resistant primary focal segmental glomerulosclerosis in children. Am J Kidney Dis. 2003; 42:1121–30.
Article46. Muso E. Beneficial effect of LDL-apheresis in refractory nephrotic syndrome. Clin Exp Nephrol. 2014; 18:286–90.
Article47. Raina R, Krishnappa V. An update on LDL apheresis for nephrotic syndrome. Pediatr Nephrol. 2019; 34:1655–69.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of Serum Cytokines in Nephrotic Syndrome
- Impact of COVID-19 on the clinical course of nephrotic syndrome in children: a single-center study
- A Case of Severe Influenza Infection in a Child with Nephrotic Syndrome on Steroid Therapy
- Clinical Analysis of Children with Nephrotic Syndrome
- Thyriod Function Studies in Children with Nephrotic Syndrome