Anesth Pain Med.
2022 Apr;17(2):157-164. 10.17085/apm.21066.
Effects of chlorpheniramine on emergence agitation after general anesthesia for ureteroscopic stone surgery: a retrospective cohort study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea
- KMID: 2531691
- DOI: http://doi.org/10.17085/apm.21066
Abstract
- Background
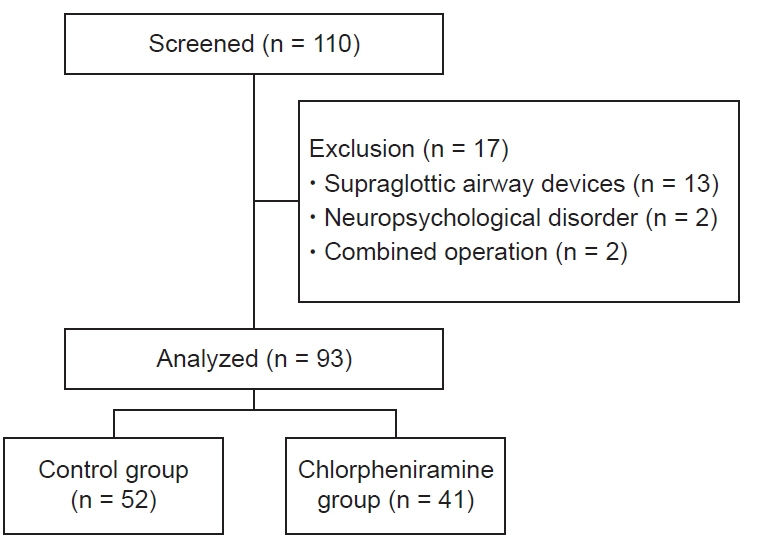
The presence of a urinary catheter, postoperative pain, and postoperative nausea and vomiting are risk factors for emergence agitation (EA). Antimuscarinic agents are primary agents used in the prevention and treatment of urinary catheter-related bladder discomfort. Chlorpheniramine has antimuscarinic, antinociceptive, and antiemetic effects. This retrospective study investigated the role of chlorpheniramine in EA prevention following ureteroscopic stone surgery. Methods: Of 110 adult patients who underwent ureteroscopic stone surgery under general anesthesia between January and December 2019, the medical records of 93 patients were analyzed retrospectively. The patients were divided into control (n = 52) and chlorpheniramine (n = 41) groups according to the receipt of intravenous chlorpheniramine before the induction of anesthesia. The incidence and severity of EA were compared between the groups as primary and secondary endpoints, respectively. The effects of chlorpheniramine on the requirement for inhalation anesthetic (desflurane) during surgery, changes in mean blood pressure and heart rate during emergence, and adverse events were also compared. Results: The incidence (21.2% in the control group, 24.4% in the chlorpheniramine group) and severity of EA did not differ between groups. The intraoperative requirement for desflurane, changes in mean blood pressure and heart rate during emergence, and adverse events were also similar between groups. Conclusions: Chlorpheniramine was not associated with a decrease in EA incidence or severity in patients who underwent ureteroscopic stone surgery
Figure
Reference
-
1. Fields A, Huang J, Schroeder D, Sprung J, Weingarten T. Agitation in adults in the post-anaesthesia care unit after general anaesthesia. Br J Anaesth. 2018; 121:1052–8.
Article2. Lee SJ, Sung TY. Emergence agitation: current knowledge and unresolved questions. Korean J Anesthesiol. 2020; 73:471–85.
Article3. Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010; 57:843–8.
Article4. Kim HC, Kim E, Jeon YT, Hwang JW, Lim YJ, Seo JH, et al. Postanaesthetic emergence agitation in adult patients after general anaesthesia for urological surgery. J Int Med Res. 2015; 43:226–35.
Article5. Hur M, Park SK, Yoon HK, Yoo S, Lee HC, Kim WH, et al. Comparative effectiveness of interventions for managing postoperative catheter-related bladder discomfort: a systematic review and network meta-analysis. J Anesth. 2019; 33:197–208.
Article6. van Schoor J. Antihistamines: a brief review. Prof Nurs Today. 2012; 16:16–21.7. Mahdy AM, Webster NR. Histamine and antihistamines. Anaesth Intensive Care Med. 2011; 12:324–9.
Article8. Tzeng JI, Lin HT, Chen YW, Hung CH, Wang JJ. Chlorpheniramine produces spinal motor, proprioceptive and nociceptive blockades in rats. Eur J Pharmacol. 2015; 752:55–60.
Article9. Morita T, Tei Y, Shishido H, Inoue S. Chlorpheniramine maleate as an alternative to antiemetic cyclizine. J Pain Symptom Manage. 2004; 27:388–90.
Article10. Rose DK. Recovery room problems or problems in the PACU. Can J Anaesth. 1996; 43(5 Pt 2):R116–28.
Article11. Laguna JJ, Archilla J, Doña I, Corominas M, Gastaminza G, Mayorga C, et al. Practical guidelines for perioperative hypersensitivity reactions. J Investig Allergol Clin Immunol. 2018; 28:216–32.
Article12. Abdellatif AA, Kamal MM, Ishak RA. Addition of dexamethasone–chlorpheniramine mixture reduces the incidence of vomiting associated with oral ketamine premedication after pediatric dental procedures. Ain-Shams J Anaesthesiol. 2016; 9:478–84.
Article13. Lee SJ, Choi SJ, In CB, Sung TY. Effects of tramadol on emergence agitation after general anesthesia for nasal surgery: a retrospective cohort study. Medicine (Baltimore). 2019; 98:e14763.14. Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med. 1999; 27:1325–9.
Article15. Vlajkovic GP, Sindjelic RP. Emergence delirium in children: many questions, few answers. Anesth Analg. 2007; 104:84–91.
Article16. Cohen IT, Hannallah RS, Hummer KA. The incidence of emergence agitation associated with desflurane anesthesia in children is reduced by fentanyl. Anesth Analg. 2001; 93:88–91.
Article17. Hahm TS, Kim CS, Koo MS, Shin BS, Hwang HY, Lee SM, et al. The effect of H1-receptor antagonist on hemodynamic change during anesthesia. Korean J Anesthesiol. 2006; 51:395–9.
Article18. Lorenz W, Duda D, Dick W, Sitter H, Doenicke A, Black A, et al. Incidence and clinical importance of perioperative histamine release: randomised study of volume loading and antihistamines after induction of anaesthesia. Trial Group Mainz/Marburg. Lancet. 1994; 343:933–40.19. Raffa RB. Antihistamines as analgesics. J Clin Pharm Ther. 2001; 26:81–5.
Article20. Ergenoglu P, Akin S, Yalcin Cok O, Eker E, Kuzgunbay B, Turunc T, et al. Effect of intraoperative paracetamol on catheter-related bladder discomfort: a prospective, randomized, double-blind study. Curr Ther Res Clin Exp. 2012; 73:186–94.
Article21. Kim JA, Min JH, Lee HS, Jo HR, Je UJ, Paek JH. Effects of glycopyrrolate premedication on preventing postoperative catheter-related bladder discomfort in patients receiving ureteroscopic removal of ureter stone. Korean J Anesthesiol. 2016; 69:563–7.
Article22. In CB, Lee SJ, Sung TY, Cho CK, Jee YS. Effects of chlorpheniramine maleate on catheter-related bladder discomfort in patients undergoing ureteroscopic stone removal: a randomized double-blind study. Int J Med Sci. 2021; 18:1075–81.
Article23. Simons FE. H1-antihistamines: more relevant than ever in the treatment of allergic disorders. J Allergy Clin Immunol. 2003; 112(4 Suppl):S42–52.24. Abdelrahman TN, Kasem AA. Role of preemptive chlorpheniramine maleate in reducing postoperative agitation after functional endoscopic sinus surgeries (FESS). Ain-Shams J Anesthesiol. 2020; 12:26.
Article25. Chen L, Xu M, Li GY, Cai WX, Zhou JX. Incidence, risk factors and consequences of emergence agitation in adult patients after elective craniotomy for brain tumor: a prospective cohort study. PLoS One. 2014; 9:e114239.
Article26. Keles S, Kocaturk O. Postoperative discomfort and emergence delirium in children undergoing dental rehabilitation under general anesthesia: comparison of nasal tracheal intubation and laryngeal mask airway. J Pain Res. 2018; 11:103–10.
Article27. Frederick HJ, Wofford K, de Lisle Dear G, Schulman SR. A randomized controlled trial to determine the effect of depth of anesthesia on emergence agitation in children. Anesth Analg. 2016; 122:1141–6.
Article28. Holzki J, Kretz FJ. Changing aspects of sevoflurane in paediatric anaesthesia: 1975-99. Paediatr Anaesth. 1999; 9:283–6.
Article29. Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth. 2010; 104:216–23.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of propofol and nalbuphine on emergence agitation after sevoflurane anesthesia in children for strabismus surgery
- The Effect of Combined Use of Remifentanil on Postoperative Recovery Time and Emergence Agitation during Sevoflurane Anesthesia in Children
- Risk factors of inadequate emergence following general anesthesia with an emphasis on patients with substance dependence history
- The effects of the non-anesthetic, non-fluoroscopic ureteroscopic removal of the lower ureter stone
- Comparison of Thiopental Sodium and Ketamine Induction on Emergence Agitation after Desflurane Anesthesia in Children undergoing a Tonsillectomy