J Cerebrovasc Endovasc Neurosurg.
2022 Jun;24(2):144-153. 10.7461/jcen.2022.E2021.12.003.
Comparison of transarterial n-BCA and Onyx embolization of brain arteriovenous malformations: A single-center 18-year retrospective analysis
- Affiliations
-
- 1Stritch School of Medicine, Loyola University Chicago, Maywood, IL, USA
- 2Semmes-Murphey Clinic, Memphis, TN, USA
- 3Clinical Research Office, Stritch School of Medicine, Loyola University Medical Center, Maywood, IL, USA
- 4Department of Pediatric Neurology, Stanford University School of Medicine, Palo Alto, CA, USA
- 5Department of Neurological Surgery, Stritch School of Medicine, Loyola University Medical Center, Maywood, IL, USA
- KMID: 2531657
- DOI: http://doi.org/10.7461/jcen.2022.E2021.12.003
Abstract
Objective
Brain arteriovenous malformations (AVM) are commonly treated with endovascular embolization. Due to the rapid evolution of endovascular technology and lack of consistent practice guidelines regarding AVM embolization, further study of AVM embolization outcomes is warranted.
Methods
We conducted a retrospective review of AVMs embolized at a single center from 2002-2019. Patient demographics, AVM characteristics, intention of embolization, and angiographic and clinical outcome after embolization were recorded. We compared the embolization results of those treated with n-butyl cyanoacrylate (n-BCA) and Onyx.
Results
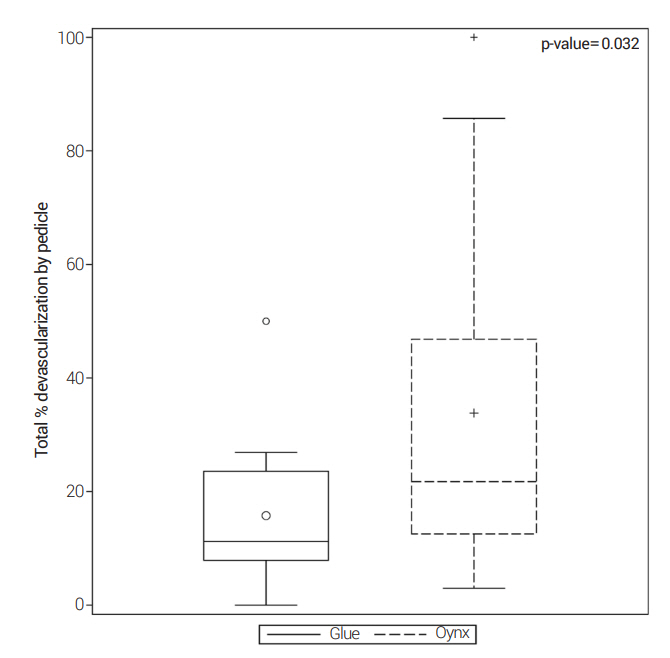
Over an 18-year period at our institution, 30 (33%) of 92 AVMs were treated with embolization. n-BCA was used in 12 cases and Onyx in 18 cases. Eighty-seven pedicles were embolized over 47 embolization sessions. Fifty percent of AVMs treated with n-BCA underwent more than one embolization session compared to 22% when Onyx was used. The median total percent volume reduction in the n-BCA AVMs was 52% compared to 51% in Onyx AVMs. There were 2 periprocedural complications in the n-BCA cohort and none in the Onyx cohort.
Conclusions
In this small retrospective series, Onyx and n-BCA achieved similar occlusion results, although n-BCA required more sessions and pedicles embolized to do so.
Keyword
Figure
Reference
-
1. Alaraj A, Amin-Hanjani S, Shakur SF, Aletich VA, Ivanov A, Carlson AP, et al. Quantitative assessment of changes in cerebral arteriovenous malformation hemodynamics after embolization. Stroke. 2015; Apr. 46(4):942–7.
Article2. Alexander MD, Hippe DS, Cooke DL, Hallam DK, Hetts SW, Kim H, et al. Targeted embolization of aneurysms associated with brain arteriovenous malformations at high risk for surgical resection: A case-control study. Neurosurgery. 2018; Mar. 82(3):343–49.
Article3. Atkinson RP, Awad IA, Batjer HH, Dowd CF, Furlan A, Giannotta SL, et al. Reporting terminology for brain arteriovenous malformation clinical and radiographic features for use in clinical trials. Stroke. 2001; Jun. 32(6):1430–42.
Article4. Chapot R, Stracke P, Velasco A, Nordmeyer H, Heddier M, Stauder M, et al. The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol. 2014; Mar. 41(1):87–91.
Article5. Crowley RW, Ducruet AF, Kalani MY, Kim LJ, Albuquerque FC, McDougall CG. Neurological morbidity and mortality associated with the endovascular treatment of cerebral arteriovenous malformations before and during the Onyx era. J Neurosurg. 2015; Jun. 122(6):1492–7.
Article6. Debrun GM, Aletich V, Ausman JI, Charbel F, Dujovny M. Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Neurosurgery. 1997; Jan. 40(1):112–20. discussion 120-1.
Article7. Elsenousi A, Aletich VA, Alaraj A. Neurological outcomes and cure rates of embolization of brain arteriovenous malformations with n-butyl cyanoacrylate or Onyx: a meta-analysis. J Neurointerv Surg. 2016; Mar. 8(3):265–72.
Article8. Foroni R, Gerosa M, Pasqualin A, Hoch J, Giri G, Pasoli A, et al. Shape recovery and volume calculation from biplane angiography in the stereotactic radiosurgical treatment of arteriovenous malformations. Int J Radiat Oncol Biol Phys. 1996; Jun. 1. 35(3):565–77.
Article9. Frizzel RT, Fisher WS. Cure, morbidity, and mortality associated with embolization of brain arteriovenous malformations: a review of 1246 patients in 32 series over a 35-year period. Neurosurgery. 1995; Dec. 37(6):1031–9. discussion 1039.10. Haw CS, terBrugge K, Willinsky R, Tomlinson G. Complications of embolization of arteriovenous malformations of the brain. J Neurosurg. 2006; Feb. 104(2):226–32.
Article11. Heidenreich JO, Hartlieb S, Stendel R, Schlattmann P, Wolf K-J, Schilling AM. Bleeding complications after endovascular therapy of cerebral arteriovenous malformations. AJNR Am J Neuroradiol. 2006; Feb. 27(2):313–6.12. Imbesi SG, Knox K, Kerber CW. Reproducibility analysis of a new objective method for measuring arteriovenous malformation nidus size at angiography. AJNR Am J Neuroradiol. 2002; Mar. 23(3):412–5.13. Jayaraman MV, Marcellus ML, Hamilton S, Do HM, Campbell D, Chang SD, et al. Neurologic complications of arteriovenous malformation embolization using liquid embolic agents. AJNR Am J Neuroradiol. 2008; Feb. 29(2):242–6.
Article14. Jayaraman MV, Meyers PM, Derdeyn CP, Fraser JF, Hirsch JA, Hussain MS, et al. Reporting standards for angiographic evaluation and endovascular treatment of cerebral arteriovenous malformations. J Neurointerv Surg. 2012; Sep. 4(5):325–30.15. Kashanian A, Sparks H, Kaprealian T, Pouratian N. Assessing the volume of large cerebral arteriovenous malformations: Can the ABC/2 formula reliably predict true volume? J Clin Neurosci. 2019; Jul. 65:1–5.
Article16. Loh Y, Duckwiler GR. Onyx Trial Investigators. A prospective, multicenter, randomized trial of the Onyx liquid embolic system and N-butyl cyanoacrylate embolization of cerebral arteriovenous malformations. Clinical article. J Neurosurg. 2010; Oct. 113(4):733–41.17. Mohr JP, Overbey JR, Hartmann A, von Kummer R, Salman RA, Kim H, et al. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol. 2020; Jul. 19(7):573–81.
Article18. n-BCA Trail Investigators. N-butyl cyanoacrylate embolization of cerebral arteriovenous malformations: results of a prospective, randomized, multi-center trial. AJNR Am J Neuroradiol. 2002; May. 23(5):748–55.19. Pasqualin A, Barone G, Cioffi F, Rosta L, Scienza R, Da Pian R. The relevance of anatomic and hemodynamic factors to a classification of cerebral arteriovenous malformations. Neurosurgery. 1991; Mar. 28(3):370–9.
Article20. Pierot L, Cognard C, Herbreteau D, Fransen H, van Rooij WJ, Boccardi E, et al. Endovascular treatment of brain arteriovenous malformations using a liquid embolic agent: results of a prospective, multicentre study (BRAVO). Eur Radiol. 2013; Oct. 23(10):2838–45.
Article21. Roark C, Vadlamudi V, Chaudhary N, Gemmete JJ, Seinfeld J, Thompson BG. ABC/2 method does not accurately predict cerebral arteriovenous malformation volume. Neurosurgery. 2018; Feb. 82(2):220–5.
Article22. Sahlein DH, Mora P, Becske T, Nelson PK. Nidal embolization of brain arteriovenous malformations: rates of cure, partial embolization, and clinical outcome. J Neurosurg. 2012; Jul. 117(1):65–77.
Article23. See AP, Mohammaden MH, Rizko M, Stapleton CJ, Amin-Hanjani S, Charbel FT, et al. Morbidity and mortality associated with sequential flow reduction embolization technique of cerebral arteriovenous malformations using n-butyl cyanoacrylate. J Neurointerv Surg. 2021; Mar. 13(3):237–41.
Article24. Solomon RA, Connolly ES. Arteriovenous malformations of the brain. N Engl J Med. 2017; May. 376(19):1859–66.
Article25. Vinuela F, Dion JE, Duckwiler G, Martin NA, Lylyk P, Fox A, et al. Combined endovascular embolization and surgery in the management of cerebral arteriovenous malformations: experience with 101 cases. J Neurosurg. 1991; Dec. 75(6):856–64.
Article26. Weber W, Kis B, Siekmann R, Kuehne D. Endovascular treatment of intracranial arteriovenous malformations with onyx: technical aspects. AJNR Am J Neuroradiol. 2007; Feb. 28(2):371–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of transarterial n-BCA and Onyx embolization of brain arteriovenous malformations: A single-center 18-year retrospective analysis
- Transarterial Balloon-assisted Onyx Embolization of Intracranial Arteriovenous Malformations Using a Dual-lumen Balloon Microcatheter: Two Case Reports
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)
- Complication Associated with Onyx Embolization of Spinal Cord Arteriovenous Malformation
- Hairball-Like Migration of “Onyx Threads” into the Draining Vein during Transarterial Embolization of a Dural Arteriovenous Fistula: A Case Report and Experimental Validation