Pediatr Emerg Med J.
2022 Jun;9(1):57-60. 10.22470/pemj.2022.00493.
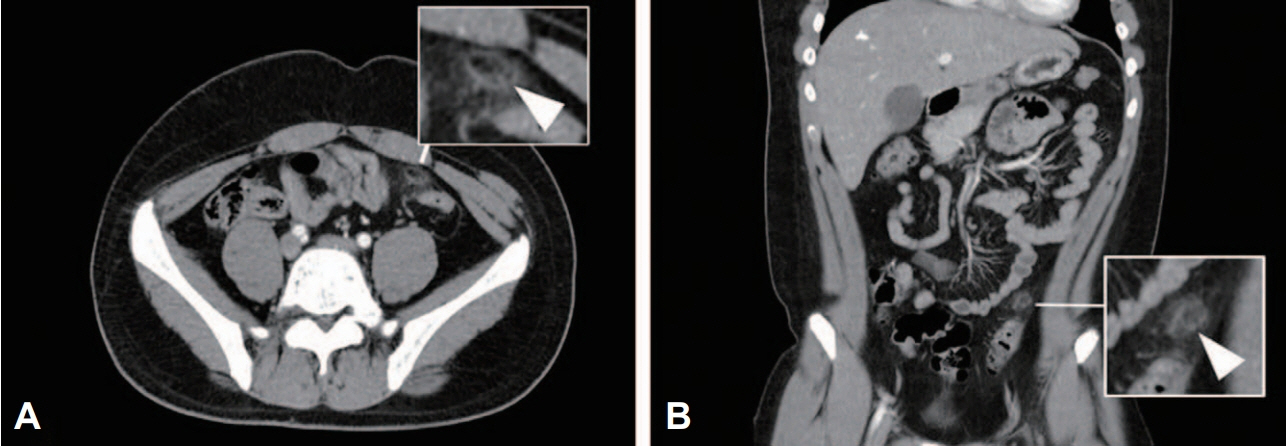
An adolescent boy with epiploic appendagitis presenting with pain in the left lower quadrant lasting for more than 10 days
- Affiliations
-
- 1Department of Pediatrics, Hanyang University Seoul Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, Hanyang University Guri Hospital, Guri, Republic of Korea
- 3Department of Pediatrics, Hanyang University College of Medicine, Seoul, Republic of Korea
- KMID: 2531532
- DOI: http://doi.org/10.22470/pemj.2022.00493
Abstract
- We report a case of a 14-year-old Korean boy presenting with pain in the left lower quadrant, persisting for over 10 days. Except for the persistent pain, no other symptoms, such as vomiting and diarrhea, were observed. In addition, laboratory findings were normal. He was eventually diagnosed with epiploic appendagitis, a rare disease in children. This case highlights the need for imaging study for early diagnosis of epiploic appendagitis or surgical emergencies in children who visit emergency departments with pain in the left lower quadrant without specific clinical findings.
Keyword
Figure
Reference
-
References
1. Boardman J, Kaplan KJ, Hollcraft C, Bui-Mansfield LT. Radiologic-pathologic conference of Keller Army Community Hospital at West Point, the United States Military Academy: torsion of the epiploic appendage. AJR Am J Roentgenol. 2003; 180:748.
Article2. Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, et al. Epiploic appendagitis--clinical characteristics of an uncommon surgical diagnosis. BMC Surg. 2007; 7:11.3. Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. Radiographics. 2005; 25:1521–34.
Article4. Chen JH, Wu CC, Wu PH. Epiploic appendagitis: an uncommon and easily misdiagnosed disease. J Dig Dis. 2011; 12:448–52.
Article5. Lo Re G, Carcione P, Vernuccio F, Martorana A, Midiri F, Cimador M, et al. Primary epiploic appendagitis in a pediatric patient: prominent role of magnetic resonance imaging in the diagnosis. Minerva Pediatr. 2015; 67:529–30.6. Legome EL, Belton AL, Murray RE, Rao PM, Novelline RA. Epiploic appendagitis: the emergency department presentation. J Emerg Med. 2002; 22:9–13.
Article7. Grundmann RT, Petersen M, Lippert H, Meyer F. The acute (surgical) abdomen-epidemiology, diagnosis and general principles of management. Z Gastroenterol. 2010; 48:696–706. German.
Article8. McCollough M, Sharieff GQ. Abdominal pain in children. Pediatr Clin North Am. 2006; 53:107–37.
Article9. Leung AK, Sigalet DL. Acute abdominal pain in children. Am Fam Physician. 2003; 67:2321–6.10. Kim JS. Acute abdominal pain in children. Pediatr Gastroenterol Hepatol Nutr. 2013; 16:219–24.
Article11. Vinson DR. Epiploic appendagitis: a new diagnosis for the emergency physician. Two case reports and a review. J Emerg Med. 1999; 17:827–32.
Article12. Thomas JH, Rosato FE, Patterson LT. Epiploic appendagitis. Surg Gynecol Obstet. 1974; 138:23–5.13. Akinosoglou K, Kraniotis P, Thomopoulos K, Assimakopoulos SF. Epiploic appendagitis: a non-surgical cause of acute abdomen. Ann Gastroenterol. 2015; 28:296–8.14. Patel H, Abdelbaki A, Steenbergen P, Chanana C, Li S. Know the name: acute epiploic appendagitis-CT findings and review of literature. AME Case Rep. 2018; 2:8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Epiploic Appendagitis after COVID-19
- A Case of Epiploic Appendagitis with Acute Gastroenteritis
- Incidentally Diagnosed Colon Cancer by Ultrasound due to Acute Abdomen Caused by Primary Epiploic Appendagitis
- A Case of Primary Epiploic Appendagitis
- A Case of Epiploic Appendagitis Presented with Right Lower Quadrant Pain of Abdomen