J Korean Med Sci.
2022 Jul;37(27):e213. 10.3346/jkms.2022.37.e213.
Persistent Symptoms After Acute COVID-19 Infection in Omicron Era
- Affiliations
-
- 1Department of Neurology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 2Division of Pulmonary and Critical Care Medicine, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 3Department of Infectious Disease, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 4Department of Physical Medicine and Rehabilitation, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 5The Office of Chief Executive Officer and Chairman, Department of General Surgery, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- KMID: 2531251
- DOI: http://doi.org/10.3346/jkms.2022.37.e213
Abstract
- Background
We aim to compare the clinical characteristics and subjectively reported symptoms of the acute coronavirus disease (COVID) phase and those of the post-acute COVID phase to examine varying factors that affect the number of persistent symptoms and their categories.
Methods
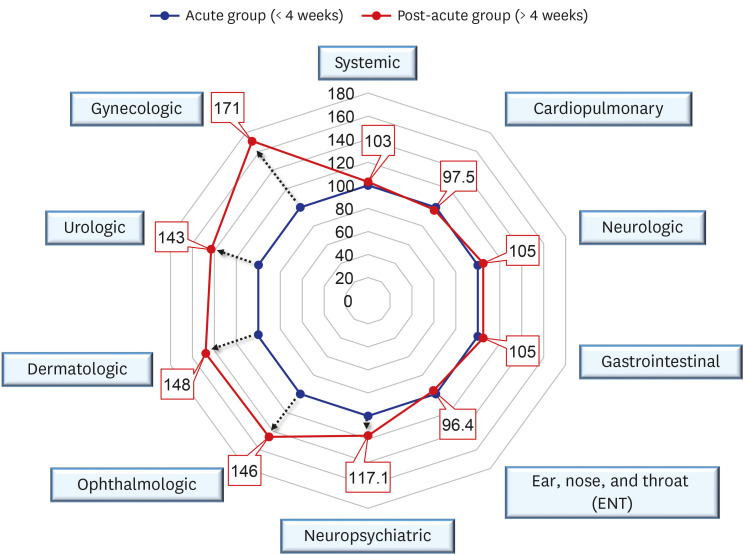
We categorized 1,122 patients who visited the post coronavirus disease 2019 (COVID-19) clinic into two groups: “acute group” (< 4 weeks following diagnosis of COVID-19) and “post-acute group” (> 4 weeks following diagnosis of COVID-19). We statistically compared clinical characteristics between the two groups and determined which factors are associated with the number of persistent symptoms and their categories.
Results
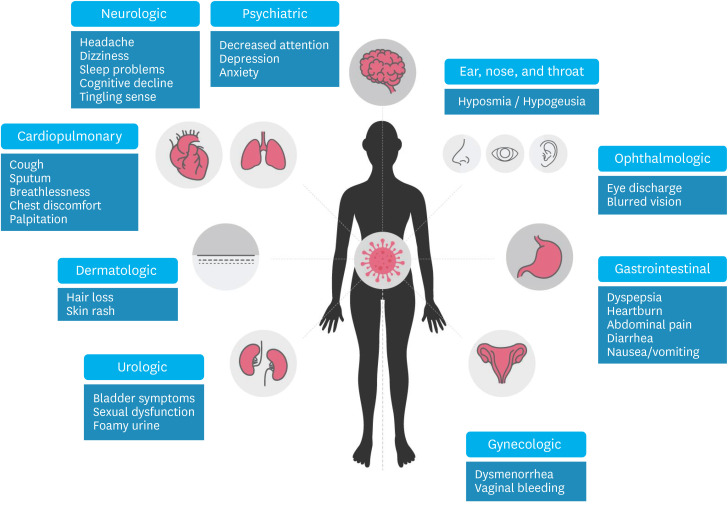
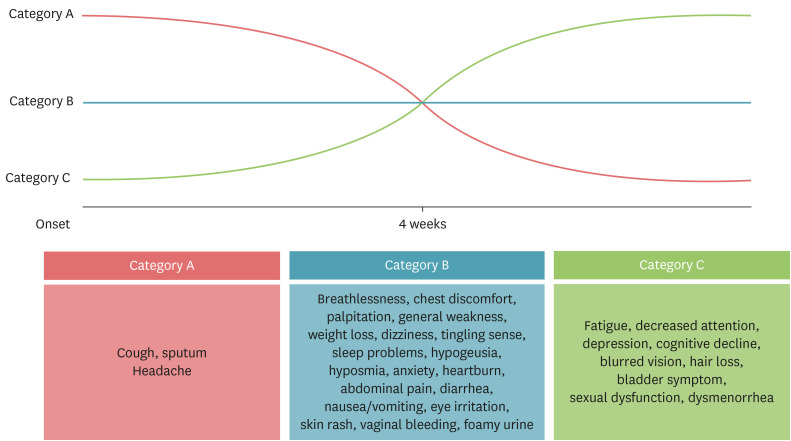
The persistent symptoms of post COVID-19 conditions were classified into three categories as follows: Category A (the prevalence of symptoms is higher in the acute-visit group than in the post-acute-visit group), Category B (the prevalence of symptoms is not different between the two groups) and Category C (the prevalence of symptoms is higher in the post-acute-visit group than in the acute-visit group). Category A mainly included respiratory symptoms. Category B had generalized weakness, weight loss, cardiologic symptoms, hypogeusia, hyposmia, anxiety, and various gastrointestinal symptoms. Category C included fatigue, decreased attention, depression, blurred vision, hair loss, and sexual dysfunction. Anxiety, depression, fatigue and age were also associated with the number of symptoms and their categories, and anxiety is the most correlated factor (P < 0.001) among them.
Conclusion
The persistent symptoms of post COVID-19 condition involve multi-organ and continue for four weeks or greater. Therefore, long-term observation and multidisciplinary interventions are essential for patients with post COVID-19 conditions.
Keyword
Figure
Reference
-
1. Araf Y, Akter F, Tang Yd, Fatemi R, Parvez SA, Zheng C, et al. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. 2022; 94(5):1825–1832. PMID: 35023191.
Article2. Ryu BH, Hong SI, Lim SJ, Cho Y, Hwang C, Kang H, et al. Clinical features of adult COVID-19 patients without risk factors before and after the nationwide SARS-CoV-2 B.1.617.2 (Delta)-variant outbreak in Korea: experience from Gyeongsangnam-do. J Korean Med Sci. 2021; 36(49):e341. PMID: 34931500.
Article3. Seok H, Lim S, Kim JY, Park CH, Kim JH, Woo ML, et al. Infectivity of coronavirus disease 2019: a prospective cohort study in the Korean metropolitan area. J Korean Med Sci. 2022; 37(14):e106. PMID: 35411726.
Article4. Yelin D, Moschopoulos CD, Margalit I, Gkrania-Klotsas E, Landi F, Stahl JP, et al. ESCMID rapid guidelines for assessment and management of long COVID. Clin Microbiol Infect. 2022; 28(7):S1198-743X(22)00092-1.
Article5. Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open. 2021; 4(5):e2111417. PMID: 34037731.6. Kim Y, Bitna-Ha , Kim SW, Chang HH, Kwon KT, Bae S, et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis. 2022; 22(1):93. PMID: 35086489.
Article7. Kim Y, Kim SW, Chang HH, Kwon KT, Bae S, Hwang S. Significance and associated factors of long-term sequelae in patients after acute COVID-19 infection in Korea. Infect Chemother. 2021; 53(3):463–476. PMID: 34405592.
Article8. Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011; 11(1):37. PMID: 21435231.
Article9. Park HY, Park WB, Lee SH, Kim JL, Lee JJ, Lee H, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health. 2020; 20(1):605. PMID: 32410603.
Article10. World Health Organization. Coronavirus disease (COVID-19): post COVID-19 condition. Updated 2021. Accessed April 22, 2022. http://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition .11. World Health Organization. Coronavirus disease (COVID-19): post COVID-19 condition. Updated 2021. Accessed April 22, 2022. http://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition .12. Goërtz YMJ, Van Herck M, Delbressine JM, Vaes AW, Meys R, Machado FVC, et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 2020; 6(4):00542-2020. PMID: 33257910.13. Jennings G, Monaghan A, Xue F, Mockler D, Romero-Ortuño R. A systematic review of persistent symptoms and residual abnormal functioning following acute COVID-19: ongoing symptomatic phase vs. post-COVID-19 syndrome. J Clin Med. 2021; 10(24):5913. PMID: 34945213.
Article14. Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021; 114(9):428–442. PMID: 34265229.
Article15. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370. PMID: 6880820.
Article16. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002; 52(2):69–77. PMID: 11832252.17. Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989; 46(10):1121–1123. PMID: 2803071.18. Hjollund NH, Andersen JH, Bech P. Assessment of fatigue in chronic disease: a bibliographic study of fatigue measurement scales. Health Qual Life Outcomes. 2007; 5(1):12. PMID: 17326844.
Article19. Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(30):993–998. PMID: 32730238.
Article20. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020; 26(7):1017–1032. PMID: 32651579.
Article21. Crook H, Raza S, Nowell J, Young M, Edison P. Long COVID-mechanisms, risk factors, and management. BMJ. 2021; 374(1648):n1648. PMID: 34312178.
Article22. Ehrenfeld M, Tincani A, Andreoli L, Cattalini M, Greenbaum A, Kanduc D, et al. COVID-19 and autoimmunity. Autoimmun Rev. 2020; 19(8):102597. PMID: 32535093.
Article23. Karlsson AC, Humbert M, Buggert M. The known unknowns of T cell immunity to COVID-19. Sci Immunol. 2020; 5(53):eabe8063. PMID: 33208380.
Article24. Ramakrishnan RK, Kashour T, Hamid Q, Halwani R, Tleyjeh IM. Unraveling the mystery surrounding post-acute sequelae of COVID-19. Front Immunol. 2021; 12:686029. PMID: 34276671.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post-COVID-19 Syndrome
- Descriptive analysis of the incidence rate of post-acute COVID-19 syndrome in the Republic of Korea Army
- Comparison of the Clinical and Laboratory Features of COVID-19 in Children During All Waves of the Epidemic: A Single Center Retrospective Study
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era
- COVID-19 and Fungal Infection