J Korean Assoc Oral Maxillofac Surg.
2022 Jun;48(3):167-173. 10.5125/jkaoms.2022.48.3.167.
Minimal clinically important difference of mouth opening in oral submucous fibrosis patients: a retrospective study
- Affiliations
-
- 1Oral and Maxillofacial Surgery, Department of Dentistry, All India Institute of Medical Sciences (AIIMS), Jodhpur, India
- 2Department of Community Medicine and Family Medicine, All India Institute of Medical Sciences (AIIMS), Jodhpur, India
- KMID: 2531053
- DOI: http://doi.org/10.5125/jkaoms.2022.48.3.167
Abstract
Objectives
The purpose of this study was to estimate the minimal clinically important difference (MCID) of mouth opening (MO) and patient satisfaction in surgically treated oral submucous fibrosis (OSMF) patients.
Materials and Methods
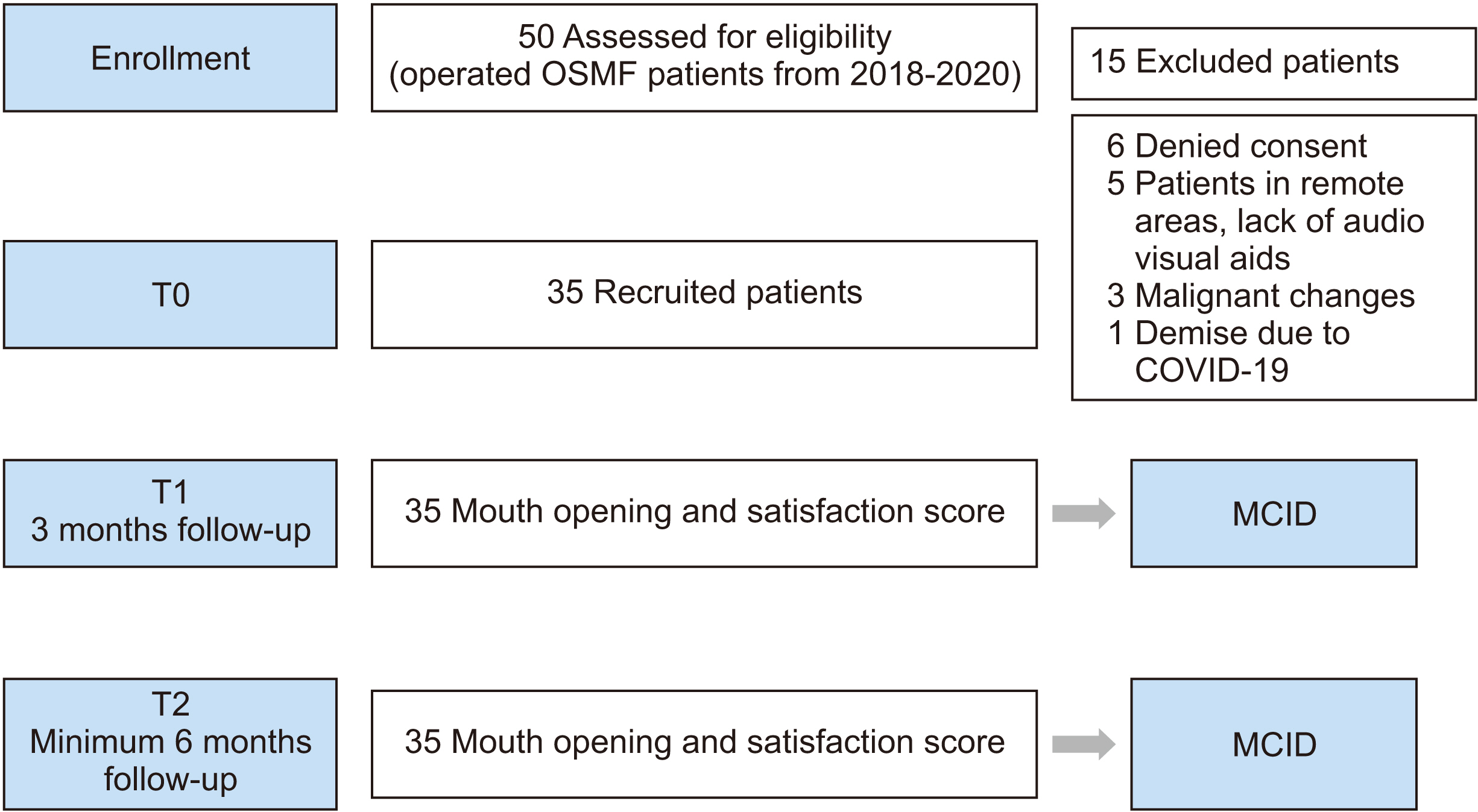
The status of MO was collected preoperatively (T0), postoperatively at 3 months (T1), and at a minimum of 6 months postoperatively (T2). MCID was determined through the anchor-based approach with the change difference method, mean change method, and receiver operator characteristic curve (ROC) method.
Results
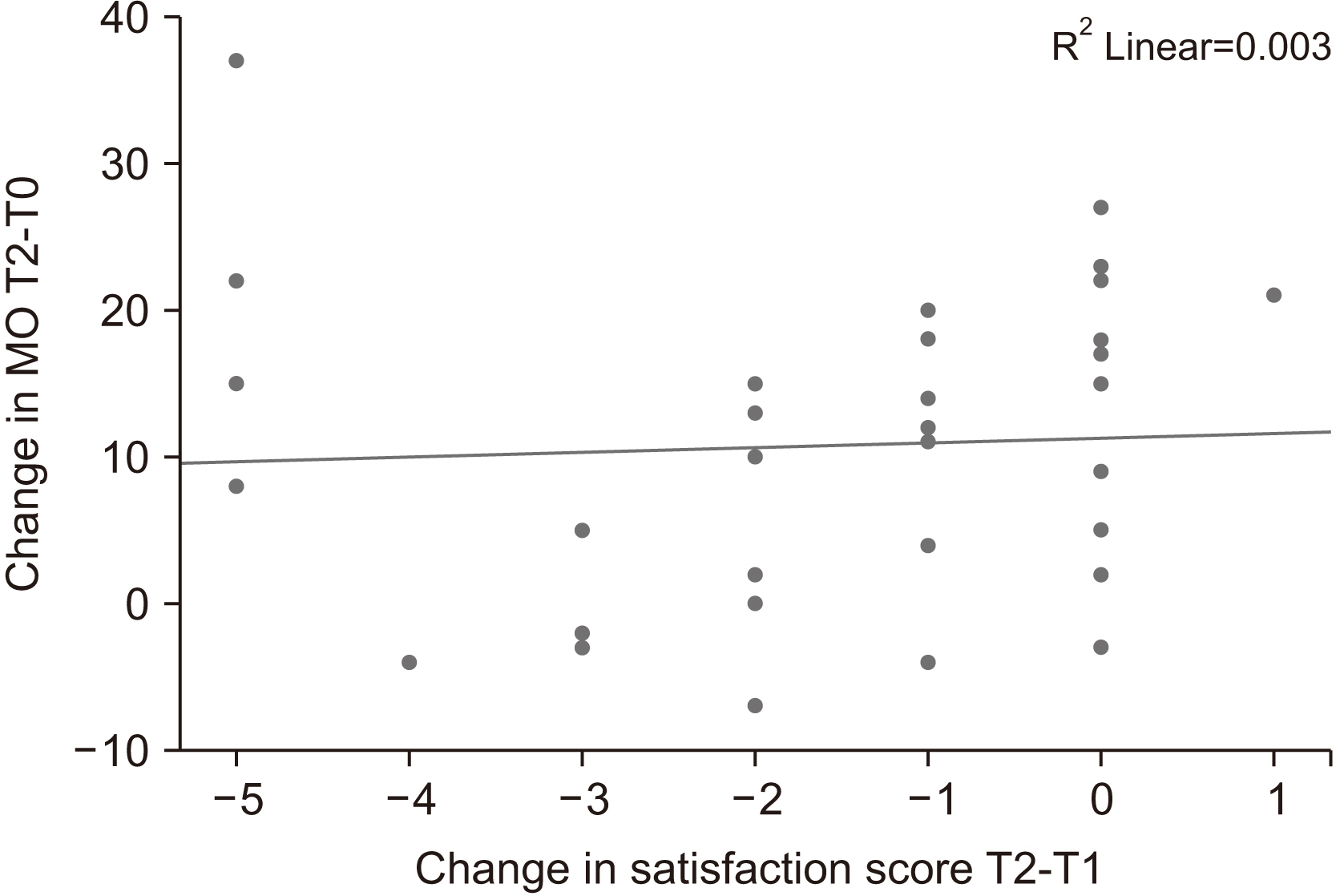
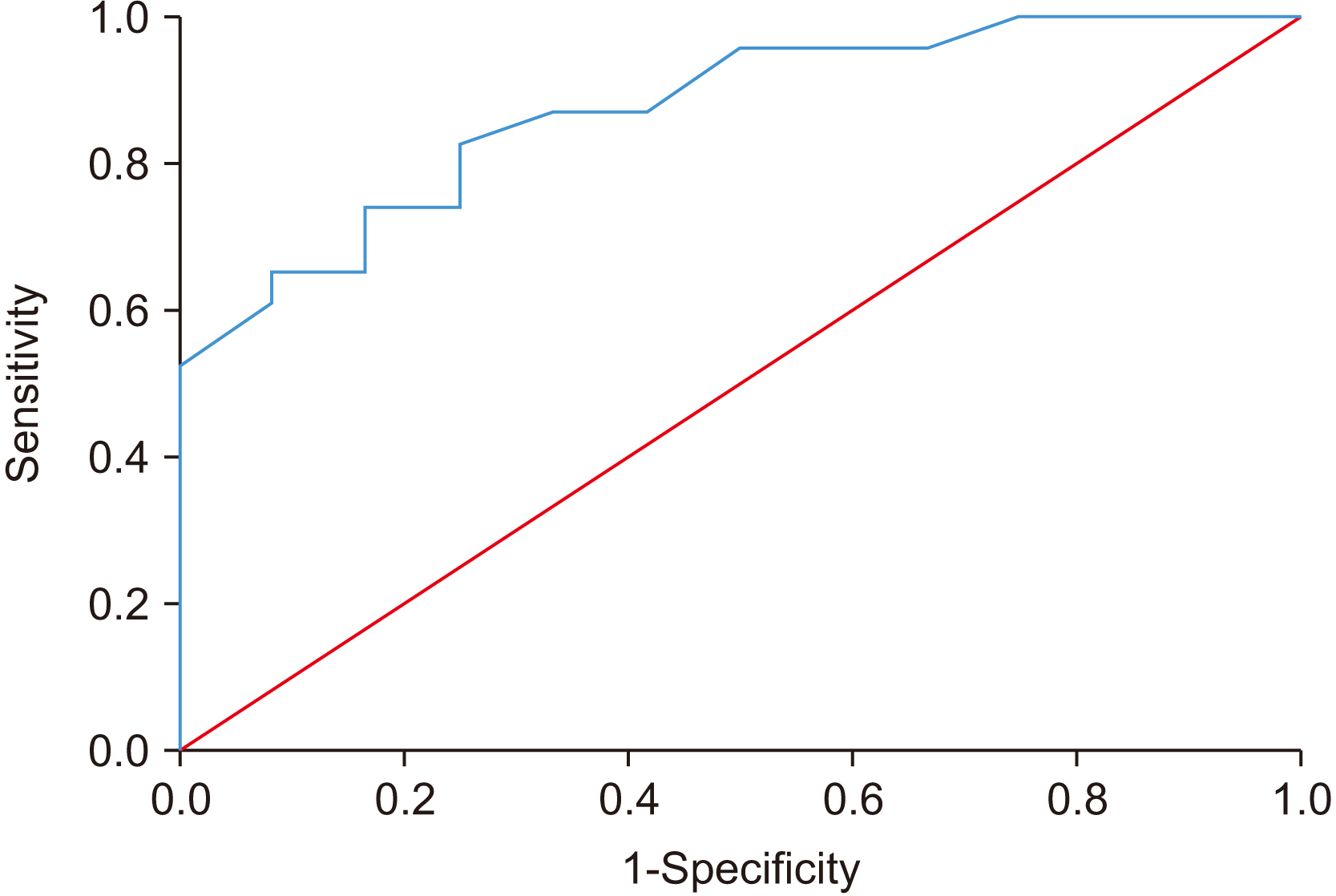
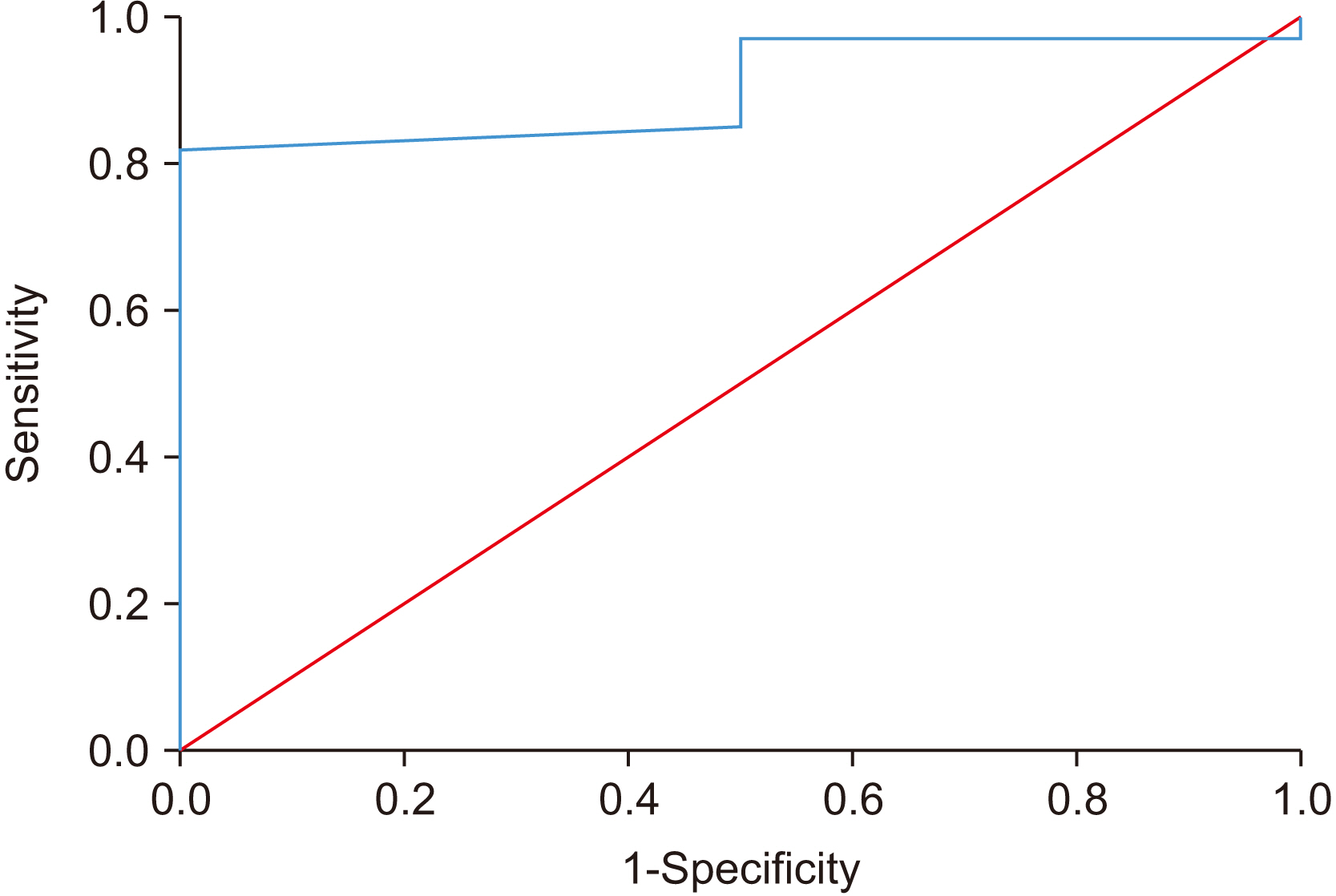
In this study, 35 patients enrolled and completed postoperative follow-up (T2) averaging a duration of 18.1 months. At T1, using the change difference method, MO was 14.89 mm and the ROC curve exhibited a 11.5 gain in MO (sensitivity 81.8% and specificity 100%, area under the curve [AUC] of 0.902) and was classified as MCID as reported by patients. At T2, MCID of MO was 9.75 mm using the change difference method and 11.75 mm by the mean change method. The ROC curve revealed that the MCID of MO at T2 was 10.5 mm with 73.9% sensitivity and 83.3% specificity (AUC of 0.873). The kappa value was 0.91, confirming reliability of the data.
Conclusion
This study demonstrated MCID values that indicate the clinical relevance of surgical treatment of OSMF if the minimum possible gain in MO is approximately 10 mm.
Figure
Cited by 1 articles
-
Exploring the role of angiogenesis in fibrosis and malignant transformation in oral submucous fibrosis: a systematic review and meta-analysis
Keerthika R, Akhilesh Chandra, Dinesh Raja, Mahesh Khairnar, Rahul Agrawal
J Korean Assoc Oral Maxillofac Surg. 2024;50(5):243-252. doi: 10.5125/jkaoms.2024.50.5.243.
Reference
-
References
1. Rao NR, Villa A, More CB, Jayasinghe RD, Kerr AR, Johnson NW. 2020; Oral submucous fibrosis: a contemporary narrative review with a proposed inter-professional approach for an early diagnosis and clinical management. J Otolaryngol Head Neck Surg. 49:3. https://doi.org/10.1186/s40463-020-0399-7. DOI: 10.1186/s40463-020-0399-7. PMID: 31915073. PMCID: PMC6951010.
Article2. Chole RH, Patil R. 2018; Assessment of the quality of life and performance status in patients with oral submucous fibrosis in central India. Clujul Med. 91:203–8. https://doi.org/10.15386/cjmed-806. DOI: 10.15386/cjmed-806. PMID: 29785159. PMCID: PMC5958986.
Article3. Kyte DG, Calvert M, van der Wees PJ, ten Hove R, Tolan S, Hill JC. 2015; An introduction to patient-reported outcome measures (PROMs) in physiotherapy. Physiotherapy. 101:119–25. https://doi.org/10.1016/j.physio.2014.11.003. DOI: 10.1016/j.physio.2014.11.003. PMID: 25620440.
Article4. Jaeschke R, Singer J, Guyatt GH. 1989; Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 10:407–15. https://doi.org/10.1016/0197-2456(89)90005-6. DOI: 10.1016/0197-2456(89)90005-6. PMID: 2691207.
Article5. Sutton RM, McDonald EL, Shakked RJ, Fuchs D, Raikin SM. 2019; Determination of minimum clinically important difference (MCID) in visual analog scale (VAS) pain and foot and ankle ability measure (FAAM) scores after hallux valgus surgery. Foot Ankle Int. 40:687–93. https://doi.org/10.1177/1071100719834539. DOI: 10.1177/1071100719834539. PMID: 30841749.
Article6. Torrens C, Guirro P, Santana F. 2016; The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 25:262–8. https://doi.org/10.1016/j.jse.2015.07.020. DOI: 10.1016/j.jse.2015.07.020. PMID: 26422525.
Article7. Tashjian RZ, Deloach J, Porucznik CA, Powell AP. 2009; Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 18:927–32. https://doi.org/10.1016/j.jse.2009.03.021. DOI: 10.1016/j.jse.2009.03.021. PMID: 19535272.
Article8. Asher AL, Kerezoudis P, Mummaneni PV, Bisson EF, Glassman SD, Foley KT, et al. 2018; Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the Quality Outcomes Database. Neurosurg Focus. 44:E2. https://doi.org/10.3171/2017.10.FOCUS17554. DOI: 10.3171/2017.10.FOCUS17554. PMID: 29290132.
Article9. Levy JM, Mace JC, Bodner TE, Alt JA, Smith TL. 2017; Defining the minimal clinically important difference for olfactory outcomes in the surgical treatment of chronic rhinosinusitis. Int Forum Allergy Rhinol. 7:821–6. https://doi.org/10.1002/alr.21964. DOI: 10.1002/alr.21964. PMID: 28556611. PMCID: PMC5544549.
Article10. Ingram M, Choi YH, Chiu CY, Haggard R, Dougall AL, Buschang P, et al. 2011; Use of the minimal clinically important difference (MCID) for evaluating treatment outcomes with TMJMD patients: a preliminary study. J Appl Biobehav Res. 16:148–66. https://doi.org/10.1111/j.1751-9861.2011.00068.x. DOI: 10.1111/j.1751-9861.2011.00068.x. PMID: 22919263. PMCID: PMC3423998.
Article11. Khanna JN, Andrade NN. 1995; Oral submucous fibrosis: a new concept in surgical management. Report of 100 cases. Int J Oral Maxillofac Surg. 24:433–9. https://doi.org/10.1016/s0901-5027(05)80473-4. DOI: 10.1016/S0901-5027(05)80473-4. PMID: 8636640.
Article12. Wright A, Hannon J, Hegedus EJ, Kavchak AE. 2012; Clinimetrics corner: a closer look at the minimal clinically important difference (MCID). J Man Manip Ther. 20:160–6. https://doi.org/10.1179/2042618612Y.0000000001. DOI: 10.1179/2042618612Y.0000000001. PMID: 23904756. PMCID: PMC3419574.
Article13. Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC. 2007; Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 7:541–6. https://doi.org/10.1016/j.spinee.2007.01.008. DOI: 10.1016/j.spinee.2007.01.008. PMID: 17448732.
Article14. Crosby RD, Kolotkin RL, Williams GR. 2003; Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. 56:395–407. https://doi.org/10.1016/s0895-4356(03)00044-1. DOI: 10.1016/S0895-4356(03)00044-1. PMID: 12812812.
Article15. Sedaghat AR. 2019; Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngol Head Neck Surg. 161:551–60. https://doi.org/10.1177/0194599819852604. DOI: 10.1177/0194599819852604. PMID: 31159641.
Article16. Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. 2008; Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J. 8:968–74. https://doi.org/10.1016/j.spinee.2007.11.006. DOI: 10.1016/j.spinee.2007.11.006. PMID: 18201937.
Article17. Parker SL, Mendenhall SK, Shau DN, Adogwa O, Anderson WN, Devin CJ, et al. 2012; Minimum clinically important difference in pain, disability, and quality of life after neural decompression and fusion for same-level recurrent lumbar stenosis: understanding clinical versus statistical significance. J Neurosurg Spine. 16:471–8. https://doi.org/10.3171/2012.1.SPINE11842. DOI: 10.3171/2012.1.SPINE11842. PMID: 22324801.
Article18. Ren D, Wu T, Wan C, Li G, Qi Y, Fang Y, et al. 2021; Exploration of the methods of establishing the minimum clinical important difference based on anchor and its application in the quality of life measurement scale QLICP-ES (V2.0) for esophageal cancer. Health Qual Life Outcomes. 19:173. https://doi.org/10.1186/s12955-021-01808-7. DOI: 10.1186/s12955-021-01808-7. PMID: 34215267. PMCID: PMC8254221.
Article19. Coeytaux RR, Kaufman JS, Chao R, Mann JD, Devellis RF. 2006; Four methods of estimating the minimal important difference score were compared to establish a clinically significant change in headache impact test. J Clin Epidemiol. 59:374–80. https://doi.org/10.1016/j.jclinepi.2005.05.010. DOI: 10.1016/j.jclinepi.2005.05.010. PMID: 16549259.
Article20. de Vet HC, Beckerman H, Terwee CB, Terluin B, Bouter LM. 2006; Definition of clinical differences. J Rheumatol. 33:434. author reply 435. PMID: 16465677.21. Tubach F, Ravaud P, Beaton D, Boers M, Bombardier C, Felson DT, et al. 2007; Minimal clinically important improvement and patient acceptable symptom state for subjective outcome measures in rheumatic disorders. J Rheumatol. 34:1188–93. PMID: 17477485. PMCID: PMC2760122.22. Copay AG, Chung AS, Eyberg B, Olmscheid N, Chutkan N, Spangehl MJ. 2018; Minimum clinically important difference: current trends in the orthopaedic literature, part I: upper extremity: a systematic review. JBJS Rev. 6:e1. https://doi.org/10.2106/JBJS.RVW.17.00159. DOI: 10.2106/JBJS.RVW.17.00159. PMID: 30179897.
Article23. Maltenfort M, Díaz-Ledezma C. 2017; Statistics in brief: minimum clinically important difference-availability of reliable estimates. Clin Orthop Relat Res. 475:933–46. https://doi.org/10.1007/s11999-016-5204-6. DOI: 10.1007/s11999-016-5204-6. PMID: 28050812. PMCID: PMC5339150.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nasolabial and extended nasolabial flaps for reconstruction in oral submucous fibrosis
- Association Between Grading of Oral Submucous Fibrosis With Frequency and Consumption of Areca Nut and Its Derivatives in a Wide Age Group: A Multi-centric Cross Sectional Study From Karachi, Pakistan
- Application of free radial forearm flap after release of fibrotic ankylosis on buccal area
- Mouth opening limitation due to oral submucosa fibrosis: a case report
- Proinflammatory cytokine levels in oral lichen planus, oral leukoplakia, and oral submucous fibrosis