Korean J Pain.
2022 Jul;35(3):345-352. 10.3344/kjp.2022.35.3.345.
Relationship between needle depth for lumbar transforaminal epidural injection and patients’ height and weight using magnetic resonance imaging
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- 2Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2530990
- DOI: http://doi.org/10.3344/kjp.2022.35.3.345
Abstract
- Background
Optimal needle depth in transforaminal epidural injection (TFEI) is determined by body measurements and is influenced by the needle entry angle. Physician can choose the appropriate needle length and perform the procedure more effectively if depth is predicted in advance.
Methods
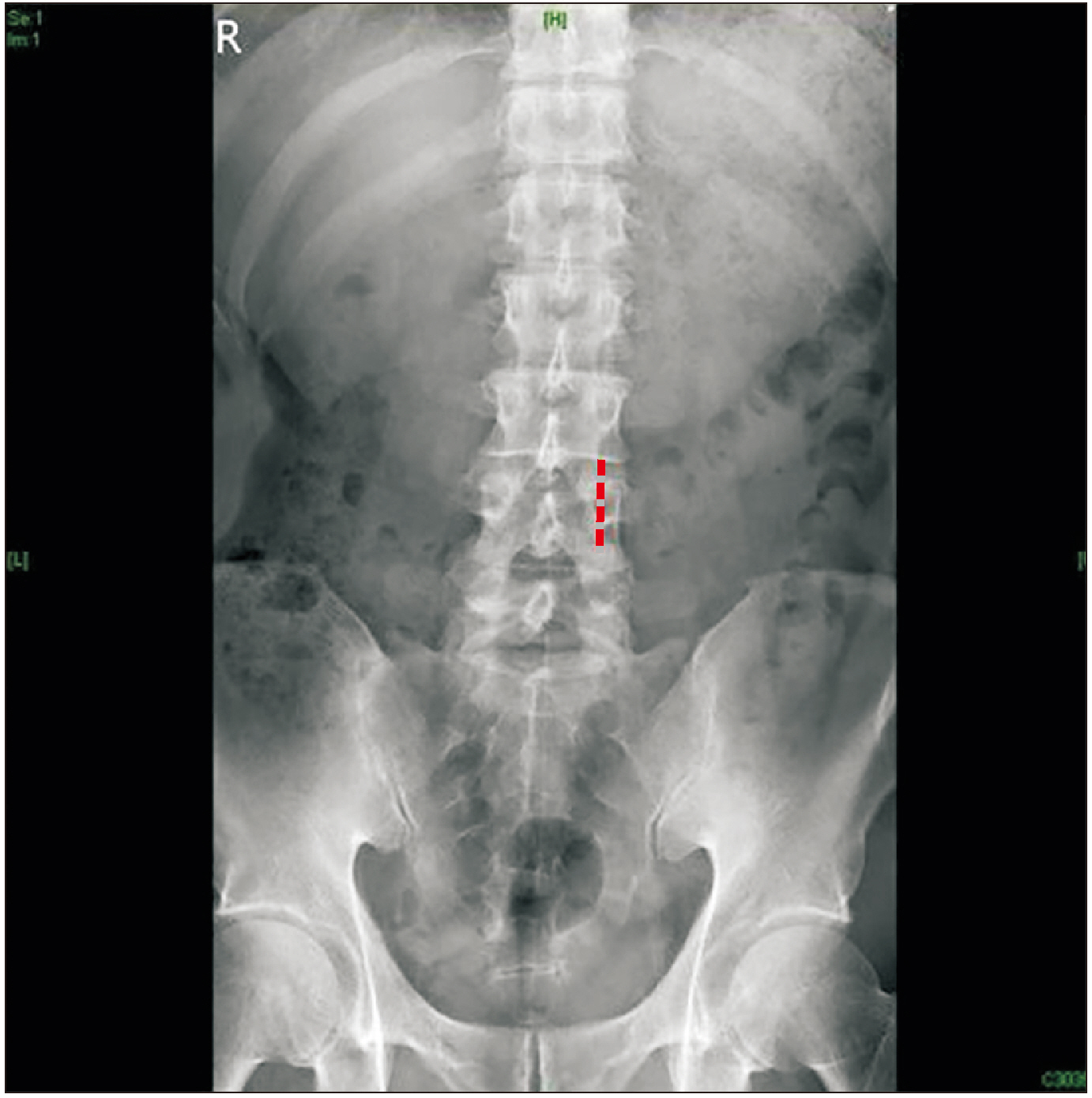
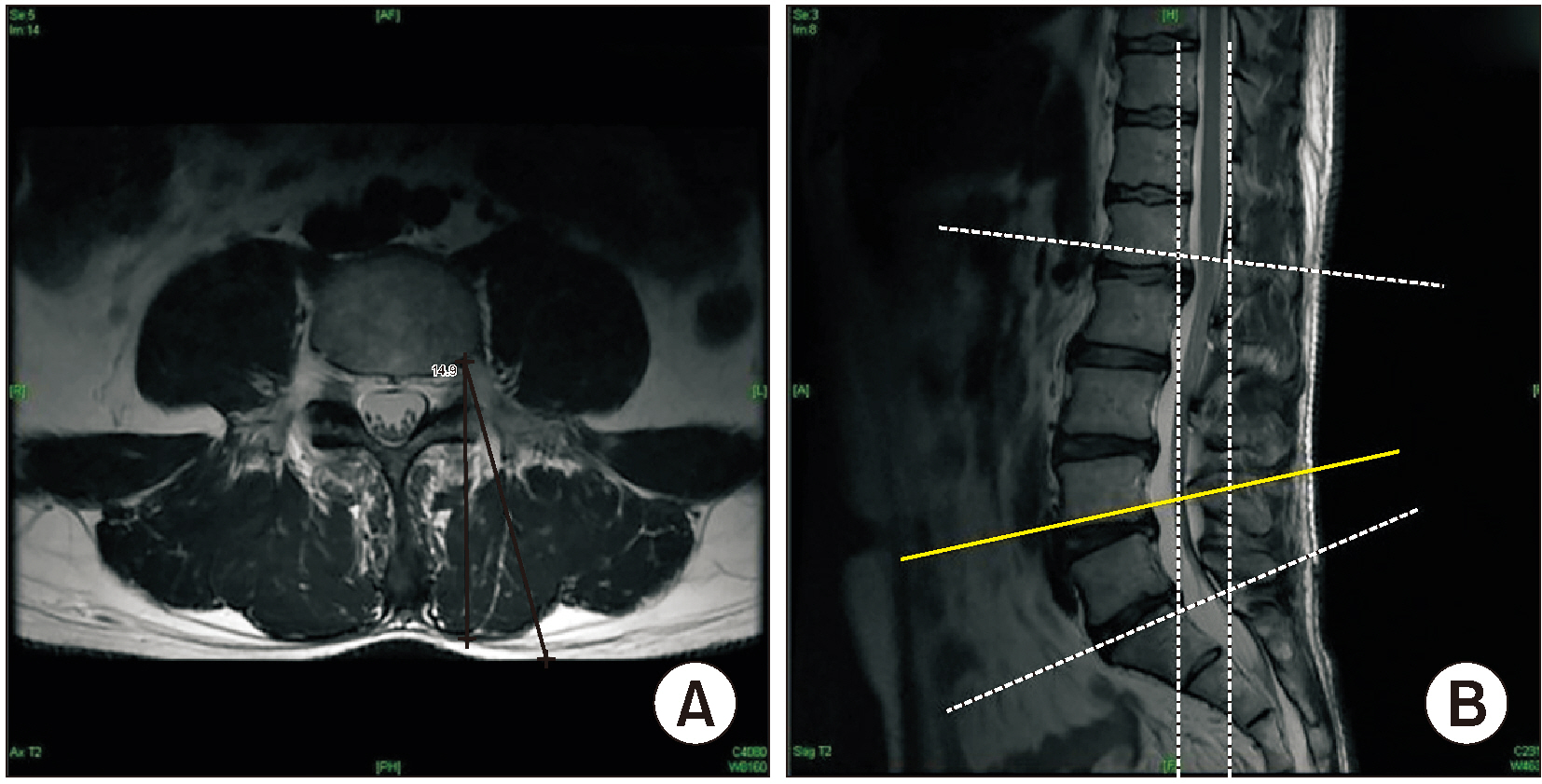
This retrospective study included patients with lumbosacral pain from a single university hospital. The skin depth from the target point was measured using magnetic resonance imaging transverse images. The depth was measured bilaterally for L4 and L5 TFEIs at 15°, 20°, and 25° oblique angles from the spinous process.
Results
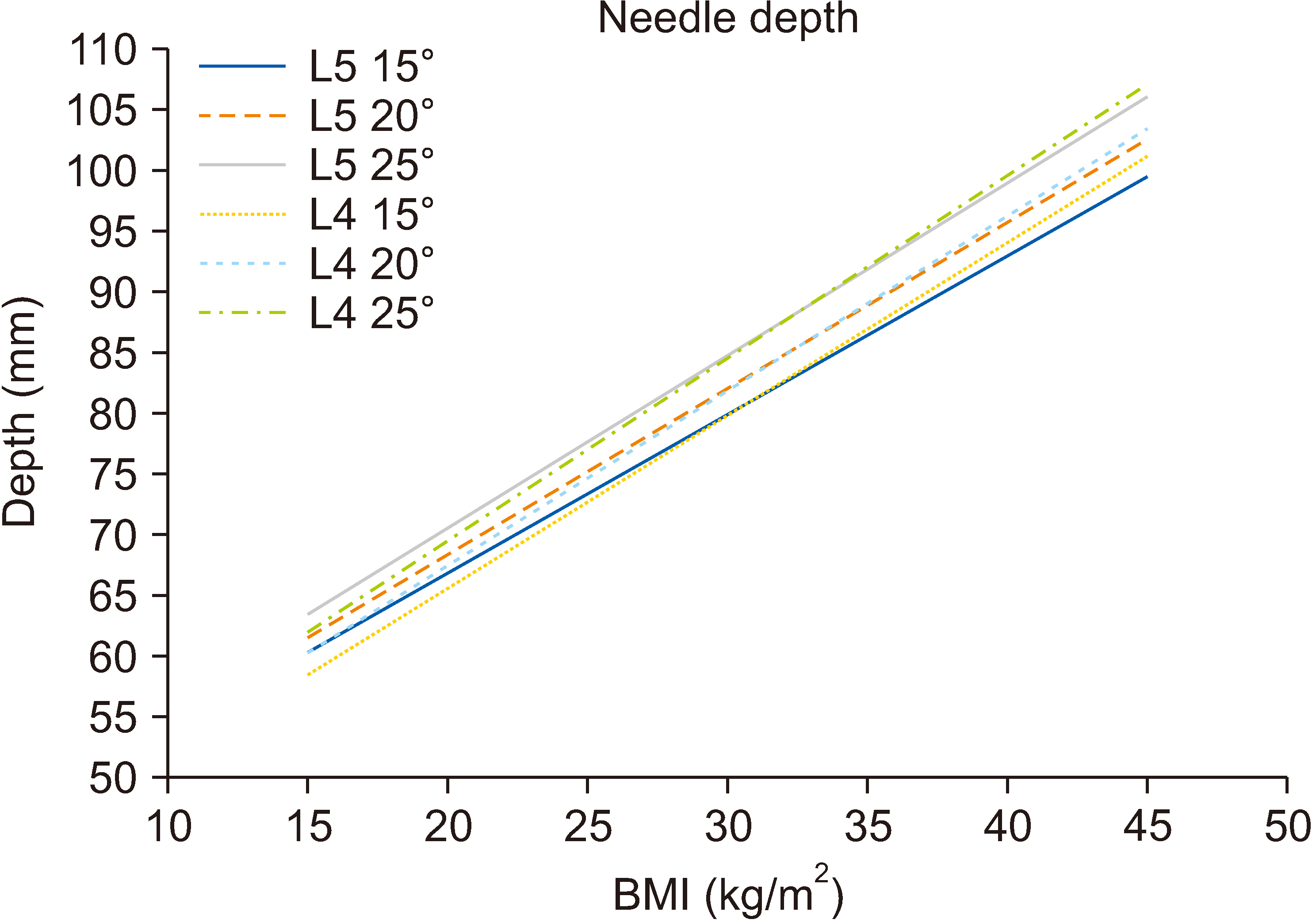
A total of 4,632 measurements of 386 patients were included. The lengths of the left and right TFEI at the same level and oblique angle were assessed, and no statistical differences were identified. Therefore, linear regression analysis was performed for bilateral L4 and L5 TFEIs. The R-squared values of height and weight combined were higher than the height, weight, and body mass index (BMI). The following equation was established: Depth (mm) = a – b (height, cm) + c (weight, kg). Based on the equation, maximal BMI capable with a 23G, 3.5-inch, Quincke-type point spinal needle was presented for three different angles (15°, 20°, and 25°) at lumbar levels L4 and L5.
Conclusions
The maximal BMI that derived from the formulated equation is listed on the table, which can help in preparations for morbid obesity. If a patient has bigger BMI than the one in the table, the clinician should prepare longer needle than the usual spinal needle.
Keyword
Figure
Cited by 1 articles
-
Data sharing: a direction for securing research transparency
Francis Sahngun Nahm
Korean J Pain. 2022;35(4):359-360. doi: 10.3344/kjp.2022.35.4.359.
Reference
-
1. Kim LK, Kim JR, Shin SS, Kim IJ, Kim BN, Hwang GT. 2011; Analysis of influencing factors to depth of epidural space for lumbar transforaminal epidural block in Korean. Korean J Pain. 24:216–20. DOI: 10.3344/kjp.2011.24.4.216. PMID: 22220243. PMCID: PMC3248585.
Article2. Manchikanti L, Pampati V, Falco FJ, Hirsch JA. 2013; Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 38:157–68. DOI: 10.1097/BRS.0b013e318267f463. PMID: 22781007.3. Sencan S, Edipoglu IS, Celenlioglu AE, Yolcu G, Gunduz OH. 2020; Comparison of treatment outcomes in lumbar central stenosis patients treated with epidural steroid injections: interlaminar versus bilateral transforaminal approach. Korean J Pain. 33:226–33. DOI: 10.3344/kjp.2020.33.3.226. PMID: 32606267. PMCID: PMC7336349.
Article4. Helm S, Harmon PC, Noe C, Calodney AK, Abd-Elsayed A, Knezevic NN, et al. 2021; Transforaminal epidural steroid injections: a systematic review and meta-analysis of efficacy and safety. Pain Physician. 24(S1):S209–32. DOI: 10.36076/ppj.2021.24.S209-S232. PMID: 33492919.5. Bensler S, Sutter R, Pfirrmann CWA, Peterson CK. 2018; Particulate versus non-particulate corticosteroids for transforaminal nerve root blocks: comparison of outcomes in 494 patients with lumbar radiculopathy. Eur Radiol. 28:946–52. DOI: 10.1007/s00330-017-5045-z. PMID: 28894933.
Article6. Vad VB, Bhat AL, Lutz GE, Cammisa F. 2002; Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976). 27:11–6. DOI: 10.1097/00007632-200201010-00005. PMID: 11805628.7. Donohue NK, Tarima SS, Durand MJ, Wu H. 2020; Comparing pain relief and functional improvement between methylprednisolone and dexamethasone lumbosacral transforaminal epidural steroid injections: a self-controlled study. Korean J Pain. 33:192–8. DOI: 10.3344/kjp.2020.33.2.192. PMID: 32235020. PMCID: PMC7136301.
Article8. Rezende R, Jacob Júnior C, da Silva CK, de Barcellos Zanon I, Cardoso IM, Batista Júnior JL. 2015; Comparison of the efficacy of transforaminal and interlaminar radicular block techniques for treating lumbar disk hernia. Rev Bras Ortop. 50:220–5. DOI: 10.1016/j.rbo.2013.12.007. PMID: 26229920. PMCID: PMC4519619.
Article9. Chang-Chien GC, Knezevic NN, McCormick Z, Chu SK, Trescot AM, Candido KD. 2014; Transforaminal versus interlaminar approaches to epidural steroid injections: a systematic review of comparative studies for lumbosacral radicular pain. Pain Physician. 17:E509–24. DOI: 10.36076/ppj.2014/17/E509. PMID: 25054401.10. Park JM, Jung H, Kwon OD, Hong SW, Kwak KH. 2013; Analysis of dispersion of lumbar interlaminar epidural injectates. Korean J Anesthesiol. 65(6 Suppl):S139–40. DOI: 10.4097/kjae.2013.65.6S.S139. PMID: 24478848. PMCID: PMC3903836. PMID: 58f3ce699fdf4d1ea71c18a6b35dda04.
Article11. Lutz GE, Vad VB, Wisneski RJ. 1998; Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil. 79:1362–6. DOI: 10.1016/S0003-9993(98)90228-3. PMID: 9821894.
Article12. Jeong JS, Shim JC, Woo JP, Shim JH. 2013; Fluoroscopic analysis of lumbar epidural contrast spread after retrograde interlaminar ventral epidural injection (RIVEI). Korean J Anesthesiol. 65:431–7. DOI: 10.4097/kjae.2013.65.5.431. PMID: 24363846. PMCID: PMC3866339. PMID: 08463409403c4b3b9f500a27e3bd3cd9.
Article13. Schaufele MK, Hatch L, Jones W. 2006; Interlaminar versus transforaminal epidural injections for the treatment of symptomatic lumbar intervertebral disc herniations. Pain Physician. 9:361–6. PMID: 17066121.14. Lee SC, Kim MW. 2004; The evaluation of epidural depth at L3-4 and L4-5 using magnetic resonance imaging and its relationship to BMI. Korean J Anesthesiol. 47:34–7. DOI: 10.4097/kjae.2004.47.1.34.
Article15. Ra IH, Min WK. 2015; Optimal angle of needle insertion for fluoroscopy-guided transforaminal epidural injection of L5. Pain Pract. 15:393–9. DOI: 10.1111/papr.12187. PMID: 24690186.
Article16. Hong JH, Lee YC, Lee HM, Kang CH. 2008; An analysis of the outcome of transforaminal epidural steroid injections in patients with spinal stenosis or herniated intervertebral discs. Korean J Pain. 21:38–43. DOI: 10.3344/kjp.2008.21.1.38.
Article17. Goodman BS, Posecion LW, Mallempati S, Bayazitoglu M. 2008; Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med. 1:212–22. DOI: 10.1007/s12178-008-9035-2. PMID: 19468908. PMCID: PMC2682416.
Article18. Chang A, Ng AT. 2020; Complications associated with lumbar transforaminal epidural steroid injections. Curr Pain Headache Rep. 24:67. DOI: 10.1007/s11916-020-00900-9. PMID: 32990823.
Article19. Husseini JS, Simeone FJ, Staffa SJ, Palmer WE, Chang CY. 2020; Fluoroscopically guided lumbar spine interlaminar and transforaminal epidural injections: inadvertent intravascular injection. Acta Radiol. 61:1534–40. DOI: 10.1177/0284185120903450. PMID: 32050772.
Article20. Algrain H, Liu A, Singh S, Vu TN, Cohen SP. 2018; Cervical epidural depth: correlation between cervical MRI measurements of the skin-to-cervical epidural space and the actual needle depth during interlaminar cervical epidural injections. Pain Med. 19:1015–22. DOI: 10.1093/pm/pnx066. PMID: 28482062.
Article21. Galbraith AS, Wallace E, Devitt A. 2019; Examining the association of body mass index and the depth of epidural space, radiation dose exposure and fluoroscopic screening time during transforaminal nerve block injection: a retrospective cohort study. Ir J Med Sci. 188:295–302. DOI: 10.1007/s11845-018-1845-7. PMID: 29911292.
Article22. Jones JH, Singh N, Nidecker A, Li CS, Fishman S. 2017; Assessing the agreement between radiologic and clinical measurements of lumbar and cervical epidural depths in patients undergoing prone interlaminar epidural steroid injection. Anesth Analg. 124:1678–85. DOI: 10.1213/ANE.0000000000001839. PMID: 28099288. PMCID: PMC5398916.
Article23. Hong JH, Lee MY, Jung SW, Lee SY. 2015; Does spinal stenosis correlate with MRI findings and pain, psychologic factor and quality of life? Korean J Anesthesiol. 68:481–7. DOI: 10.4097/kjae.2015.68.5.481. PMID: 26495059. PMCID: PMC4610928. PMID: 140d6b1309054adfbbbc5f0ec53f594b.
Article24. Brunner P, Amoretti N, Soares F, Brunner E, Cazaux E, Brocq O, et al. 2012; Approaches in injections for radicular pain: the transforaminal, epidural and transfacet approaches. Diagn Interv Imaging. 93:711–22. DOI: 10.1016/j.diii.2012.07.005. PMID: 22925594.
Article25. Bhatia A, Flamer D, Shah PS, Cohen SP. 2016; Transforaminal epidural steroid injections for treating lumbosacral radicular pain from herniated intervertebral discs: a systematic review and meta-analysis. Anesth Analg. 122:857–70. DOI: 10.1213/ANE.0000000000001155. PMID: 26891397.26. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, et al. 2002; Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. 81:898–905. DOI: 10.1097/00002060-200212000-00003. PMID: 12447088.
Article27. Botwin K, Natalicchio J, Brown LA. 2004; Epidurography contrast patterns with fluoroscopic guided lumbar transforaminal epidural injections:a prospective evaluation. Pain Physician. 7:211–5. DOI: 10.36076/ppj.2004/7/211. PMID: 16868594.28. Lee JH, Shin KH, Park SJ, Lee GJ, Lee CH, Kim DH, et al. 2018; Comparison of clinical efficacy between transforaminal and interlaminar epidural injections in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 21:433–48. DOI: 10.36076/ppj.2018.5.433. PMID: 30282389.29. Carnie J, Boden J, Gao Smith F. 2002; Prediction by computerised tomography of distance from skin to epidural space during thoracic epidural insertion. Anaesthesia. 57:701–4. DOI: 10.1046/j.1365-2044.2002.02572_4.x. PMID: 12059829.
Article30. Brummett CM, Williams BS, Hurley RW, Erdek MA. 2009; A prospective, observational study of the relationship between body mass index and depth of the epidural space during lumbar transforaminal epidural steroid injection. Reg Anesth Pain Med. 34:100–5. DOI: 10.1097/AAP.0b013e31819a12ba. PMID: 19282707. PMCID: PMC2715548.
Article31. Yingsakmongkol W, Poriswanich K, Kotheeranurak V, Numkarunarunrote N, Limthongkul W, Singhatanadgige W. 2022; How prone position affects the anatomy of lumbar nerve roots and psoas morphology for prone transpsoas lumbar interbody fusion. World Neurosurg. 160:e628–35. DOI: 10.1016/j.wneu.2022.01.104. PMID: 35108649.
Article32. Amaral R, Daher MT, Pratali R, Arnoni D, Pokorny G, Rodrigues R, et al. 2021; The effect of patient position on psoas morphology and in lumbar lordosis. World Neurosurg. 153:e131–40. DOI: 10.1016/j.wneu.2021.06.067. PMID: 34166827.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Influencing Factors to Depth of Epidural Space for Lumbar Transforaminal Epidural Block in Korean
- Correlation between Epidural Depth and Physical Measurements
- Epidural hematoma treated by aspiration after transforaminal epidural steroid injection - A case report -
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Epidural Depth in Geriatric Patients