Ann Clin Microbiol.
2022 Jun;25(2):53-58. 10.5145/ACM.2022.25.2.3.
Clinical and microbiological risk factors for community-associated Clostridioides difficile infections in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, National Health Insurance Service, Ilsan Hospital, Goyang, Korea
- 2Department of Laboratory Medicine and Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Laboratory Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- KMID: 2530723
- DOI: http://doi.org/10.5145/ACM.2022.25.2.3
Abstract
- Background
The incidence of community-associated (CA) Clostridioides difficile infection (CDI) has increased in Korea. In this study, we evaluated CA-CDI risk factors in terms of clinical features and ribotype considering its region-specific molecular epidemiology.
Methods
A retrospective case-control study was performed on two groups of CDI patients: 127 subjects with CA-CDI and 265 subjects with healthcare-associated (HA)-CDI. Risk factors for CA-CDI were evaluated in terms of clinical and microbiological features such as toxin type and ribotype.
Results
A comparison of the two groups of CDI patients revealed that inflammatory bowel disease, diarrhea, abdominal pain, and fever were more closely associated with CA-CDI. The toxin types and ribotypes of C. difficile were similar between the two groups. After adjusting for variables, no risk factors were identified for CA-CDI compared with HA-CDI.
Conclusion
Specific risk factors for CA-CDI were not identified in this study.
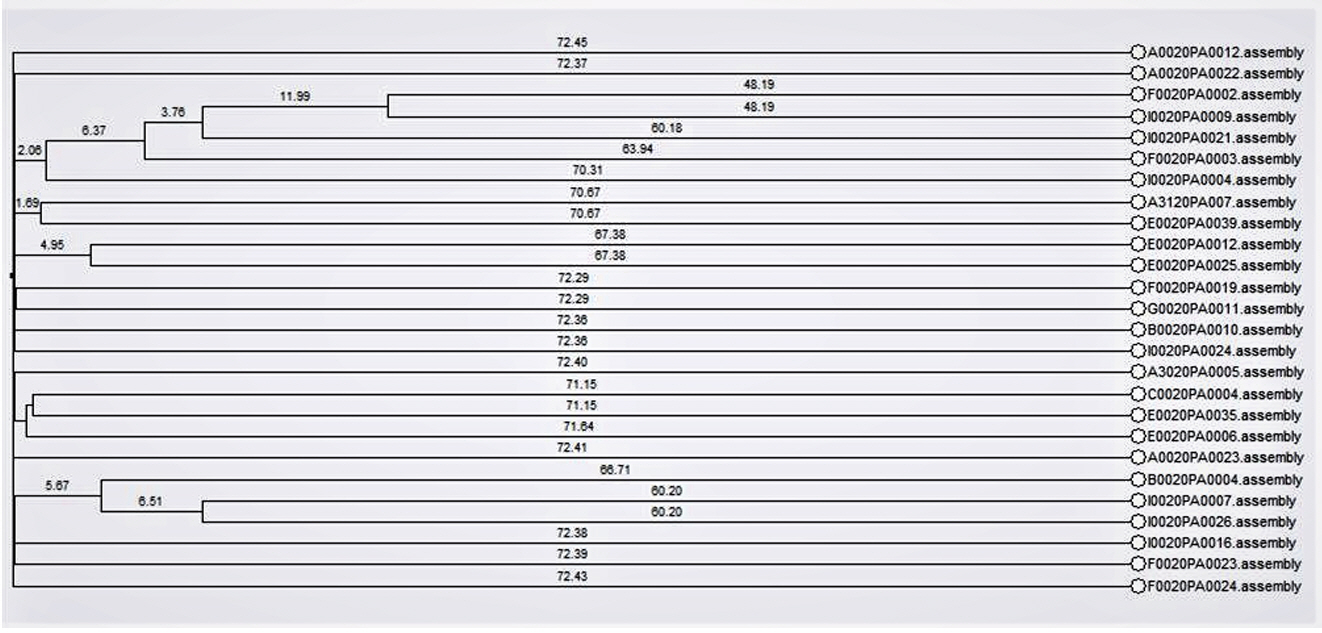
Figure
Reference
-
1. De Oliveira DMP, Forde BM, Kidd TJ, Harris PNA, Schembri MA, Beatson SA, et al. Antimicrobial resistance in ESKAPE pathogens. Clin Microbiol Rev 2020;33:e00181-19. .2. Karakonstantis S, Kritsotakis EI, Gikas A. Treatment options for K. pneumoniae, P. aeruginosa and A. baumannii co-resistant to carbapenems, aminoglycosides, polymyxins and tigecycline: an approach based on the mechanisms of resistance to carbapenems. Infection 2020;48:835-51. .3. Doi Y. Treatment options for carbapenem-resistant gram-negative bacterial infections. Clin Infect Dis 2019;69:S565-75. .4. Paulsson M, Granrot A, Ahl J, Tham J, Resman F, Riesbeck K, et al. Antimicrobial combination treatment including ciprofloxacin decreased the mortality rate of Pseudomonas aeruginosa bacteraemia: a retrospective cohort study. Eur J Clin Microbiol Infect Dis 2017;36:1187-96. .5. Kim D, Yoon EJ, Hong JS, Choi MH, Kim HS, Kim YR, et al. Major bloodstream infectioncausing bacterial pathogens and their antimicrobial resistance in South Korea, 2017-2019: phase I report from Kor-GLASS. Front Microbiol 2022;12:799084. .6. Rehman A, Patrick WM, Lamont IL. Mechanisms of ciprofloxacin resistance in Pseudomonas aeruginosa: new approaches to an old problem. J Med Microbiol 2019;68:1-10. .7. Ming DS, Chen QQ, Chen XT. Detection of 5 kinds of genes related to plasmid-mediated quinolone resistance in four species of nonfermenting bacteria with 2 drug resistant phenotypes. Can J Infect Dis Med Microbiol 2020;2020:3948719. .8. Chávez-Jacobo VM, Hernández-Ramírez KC, Romo-Rodríguez P, Pérez-Gallardo RV, Campos-García J, Gutiérrez-Corona JF, et al. CrpP is a novel ciprofloxacin-modifying enzyme encoded by the Pseudomonas aeruginosa pUM505 plasmid. Antimicrob Agents Chemother 2018;62:e02629-17. .9. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; CLSI Supplement M100. Wayne; PA: 2020. .10. Center for Genomic Epidemiology. Center for Genomic Epidemiology Web site. www. genomicepidemiology.org [Online] (last visited on 13 June 2022). .11. Blanc DS, Magalhães B, Koenig I, Senn L, Grandbastien B. Comparison of whole Genome (wg-) and core genome (cg-) MLST (BioNumericsTM) versus SNP variant calling for epidemiological investigation of Pseudomonas aeruginosa. Front Microbiol 2020;11:1729. .12. Park Y, Oh J, Park S, Sum S, Song W, Chae J, et al. Antimicrobial resistance and novel mutations detected in the gyrA and parC genes of Pseudomonas aeruginosa strains isolated from companion dogs. BMC Vet Res 2020;16:111. .13. Kim JO, Yoo IY, Yu JK, Kwon JA, Kim SY, Park YJ. Predominance and clonal spread of CTX-M-15 in cefotaxime-resistant Klebsiella pneumoniae in Korea and their association with plasmid-mediated quinolone resistance determinants. J Infect Chemother 2021;27:1186-92. .14. Lee S, Park N, Yun S, Hur E, Song J, Lee H, et al. Presence of plasmid-mediated quinolone resistance (PMQR) genes in non-typhoidal Salmonella strains with reduced susceptibility to f luoroquinolones isolated from human salmonellosis in Gyeonggi-do, South Korea from 2016 to 2019. Gut Pathog 2021;13:35. .15. Yoon EJ, Jeong SH. Mobile carbapenemase genes in Pseudomonas aeruginosa. Front Microbiol 2021;12:614058. .16. Kocsis B, Toth A, Gulyas D, Ligeti B, Katona K, Rokusz L, et al. Acquired qnrVC1 and blaNDM-1 resistance markers in an international high-risk Pseudomonas aeruginosa ST773 clone. J Med Microbiol 2019;68:336-8. .17. Lindgren PK, Marcusson LL, Sandvang D, Frimodt-Møller N, Hughes D. Biological cost of single and multiple norfloxacin resistance mutations in Escherichia coli implicated in urinary tract infections. Antimicrob Agents Chemother 2005;49:2343-51. .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and microbiological risk factors for severe Clostridioides difficile infections in Korea
- Current Strategy and Perspective View for Preventing Clostridioides Difficile Infection in Acute Care Facilities
- Clostridioides Infection in Patients with Inflammatory Bowel Disease
- Which is the Preferred Regimen for Non-Severe Clostridioides difficile Infection in Korea, Vancomycin or Metronidazole?
- Incidence and Characteristics of Clostridioides difficile Infection in Children