J Rheum Dis.
2022 Jul;29(3):181-186. 10.4078/jrd.2022.29.3.181.
Pediatric Sarcoidosis Misdiagnosed as Hepatosplenic Abscesses: A Case Report and Review
- Affiliations
-
- 1Department of Pediatrics, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Pathology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2530682
- DOI: http://doi.org/10.4078/jrd.2022.29.3.181
Abstract
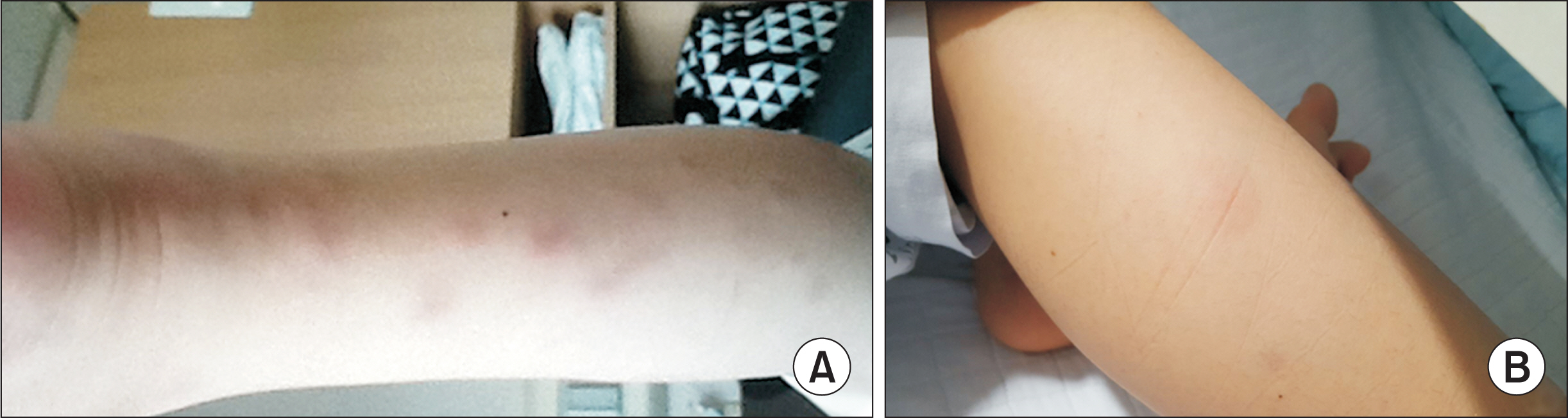
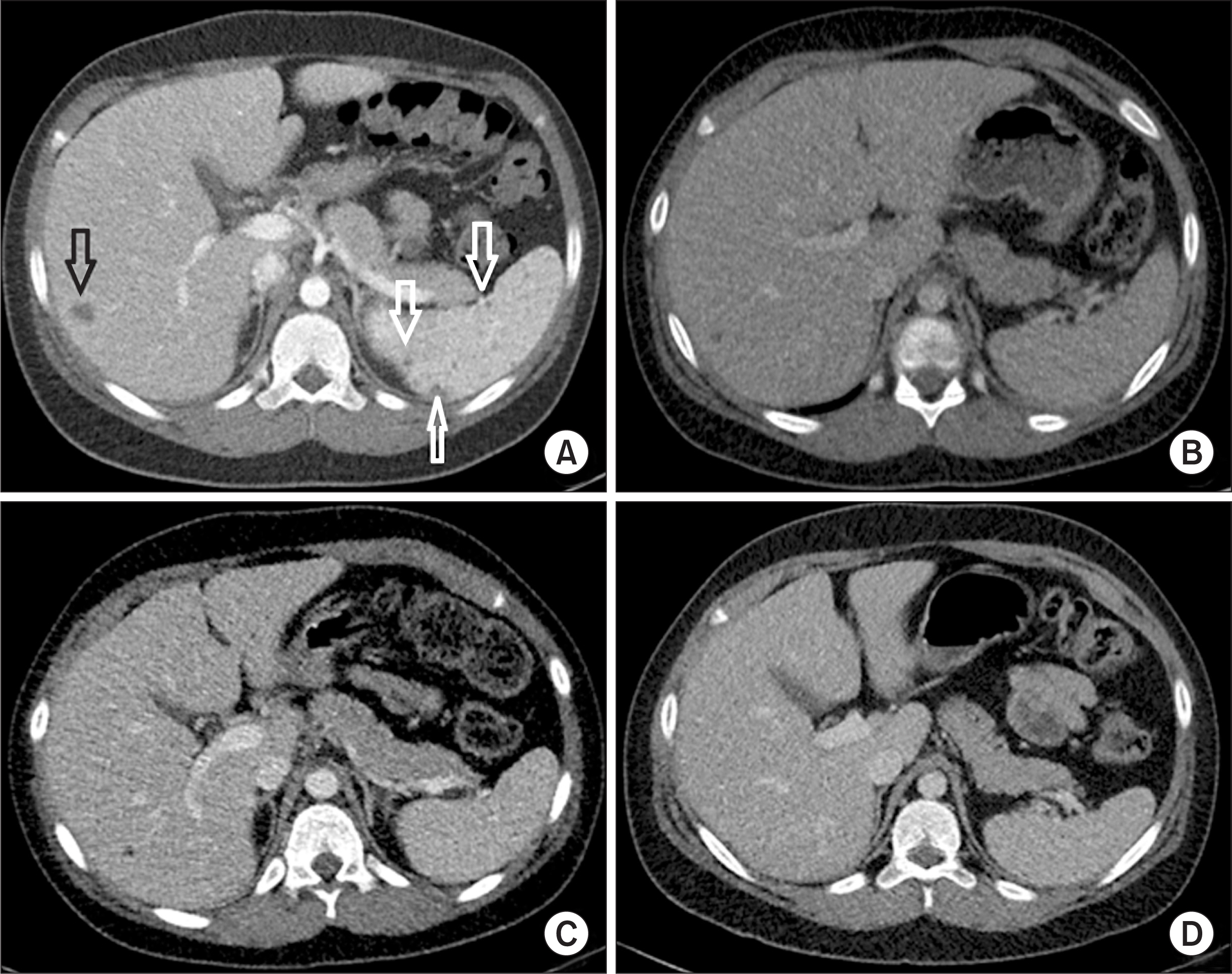
- Sarcoidosis is a systemic granulomatous disorder of unknown etiology characterized by granuloma formation. Due to the limited incidence of sarcoidosis in pediatric patients, little is known about the clinical course of this disease. A combination of clinical, radiologic, and pathologic examination is necessary to exclude other differential diagnoses (i.e., infection and granulomatous inflammatory disorder) and establish a diagnosis of sarcoidosis. Here, we report a case of histologically confirmed sarcoidosis initially misdiagnosed as hepatosplenic abscesses in an 11-year-old male. Treatment with corticosteroids improved his symptoms and resolved his skin and hepatosplenic lesions. A three-year follow-up was uneventful. This study emphasizes the importance of considering sarcoidosis in children presenting with findings of multi-organ involvement in the presence of histologic evidence of granuloma.
Keyword
Figure
Reference
-
1. Shetty AK, Gedalia A. 2000; Sarcoidosis in children. Curr Probl Pediatr. 30:149–76. DOI: 10.1067/mps.2000.105929. PMID: 10826082.
Article2. Chiu B, Chan J, Das S, Alshamma Z, Sergi C. 2019; Pediatric sarcoidosis: a review with emphasis on early onset and high-risk sarcoidosis and diagnostic challenges. Diagnostics (Basel). 9:160. DOI: 10.3390/diagnostics9040160. PMID: 31731423. PMCID: PMC6963233.
Article3. Fauroux B, Clément A. 2005; Paediatric sarcoidosis. Paediatr Respir Rev. 6:128–33. DOI: 10.1016/j.prrv.2005.03.007. PMID: 15911458.
Article4. Heinle R, Chang C. 2014; Diagnostic criteria for sarcoidosis. Autoimmun Rev. 13:383–7. DOI: 10.1016/j.autrev.2014.01.035. PMID: 24424172.
Article5. Nathan N, Sileo C, Calender A, Pacheco Y, Rosental PA, Cavalin C, et al. 2019; Paediatric sarcoidosis. Paediatr Respir Rev. 29:53–9. DOI: 10.1016/j.prrv.2018.05.003. PMID: 30917882.
Article6. Rybicki BA, Major M, Popovich J Jr, Maliarik MJ, Iannuzzi MC. 1997; Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 145:234–41. DOI: 10.1093/oxfordjournals.aje.a009096. PMID: 9012596.
Article7. Rose CD, Wouters CH. Petty RE, Laxer RM, Lindsley CB, Wedderburn LR, Mellins ED, Fuhlbrigge RC, editors. 2021. Pediatric sarcoidosis. Textbook of pediatric rheumatology. 8th ed. Elsevier;Philadelphia: p. 559–66. e2.8. Gedalia A, Khan TA, Shetty AK, Dimitriades VR, Espinoza LR. 2016; Childhood sarcoidosis: Louisiana experience. Clin Rheumatol. 35:1879–84. DOI: 10.1007/s10067-015-2870-9. PMID: 25616361.
Article9. Hoffmann AL, Milman N, Byg KE. 2004; Childhood sarcoidosis in Denmark 1979-1994: incidence, clinical features and laboratory results at presentation in 48 children. Acta Paediatr. 93:30–6. DOI: 10.1111/j.1651-2227.2004.tb00670.x. PMID: 14989436.
Article10. Shetty AK, Gedalia A. 2008; Childhood sarcoidosis: a rare but fascinating disorder. Pediatr Rheumatol Online J. 6:16. DOI: 10.1186/1546-0096-6-16. PMID: 18811966. PMCID: PMC2559831.
Article11. Whang SW, Kim DS, Lee KH. 2000; A case of early-onset childhood sarcoidosis. Korean J Dermatol. 38:1696–8.12. Jang KA, Choi JH, Sung KJ, Moon KC, Koh JK, Kim HK. 1998; Sarcoidosis in a four-year-old girl. Korean J Dermatol. 36:331–4.13. Kim SA, Bae SY, Lee SY, Jeong DC, Chung SY, Kang JH. 2006; A case of pulmonary sarcoidosis in a 6-year-old girl. Pediatr Allergy Respir Dis. 16:253–8.14. Lee JH, Lim YJ, Lee S, Joo KB, Choi YY, Park CK, et al. 2012; Early-onset childhood sarcoidosis with incidental multiple enchondromatosis. J Korean Med Sci. 27:96–100. DOI: 10.3346/jkms.2012.27.1.96. PMID: 22219622. PMCID: PMC3247783.
Article