J Stroke.
2022 May;24(2):278-287. 10.5853/jos.2021.03594.
A Practical Grading Scale for Predicting Outcomes of Radiosurgery for Dural Arteriovenous Fistulas: JLGK 1802 Study
- Affiliations
-
- 1Department of Neurosurgery, The University of Tokyo Hospital, Tokyo, Japan
- 2Jiro Suzuki Memorial Gamma House, Furukawa Seiryo Hospital, Osaki, Japan
- 3Department of Neurosurgery, Komaki City Hospital, Komaki, Japan
- 4Department of Neurosurgery, Nagatomi Neurosurgical Hospital, Oita, Japan
- 5Kyoto Gamma Knife Center, Rakusai Shimizu Hospital, Kyoto, Japan
- 6Tokyo Gamma Unit Center, Tsukiji Neurological Clinic, Tokyo, Japan
- 7Gamma Knife House, Chiba Cerebral and Cardiovascular Center, Ichihara, Japan
- 8Department of Neurosurgery, Shinsuma General Hospital, Kobe, Japan
- 9Katsuta Hospital Mito GammaHouse, Hitachinaka, Japan
- 10Department of Neurosurgery, Ehime Prefectural Central Hospital, Matsuyama, Japan
- 11Department of Neurosurgery, Brain Attack Center, Ota Memorial Hospital, Fukuyama, Japan
- 12Department of Neurosurgery, Osaka City General Hospital, Osaka, Japan
- 13Department of Neurosurgery, Kuroishi General Hospital, Kuroishi, Japan
- 14Data Science Office, Clinical Research Promotion Center, The University of Tokyo Hospital, Tokyo, Japan
- KMID: 2530530
- DOI: http://doi.org/10.5853/jos.2021.03594
Abstract
- Background and Purpose
To assess the long-term outcomes of intracranial dural arteriovenous fistula (DAVF) treated with stereotactic radiosurgery (SRS) alone or embolization and SRS (Emb-SRS) and to develop a grading system for predicting DAVF obliteration.
Methods
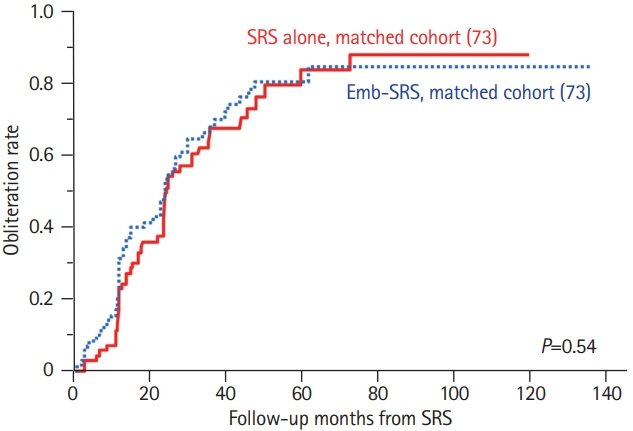
This multi-institutional retrospective study included 200 patients with DAVF treated with SRS or Emb-SRS. We investigated the long-term obliteration rate and obliteration-associated factors. We developed a new grading system to estimate the obliteration rate. Additionally, we compared the outcomes of SRS and Emb-SRS by using propensity score matching.
Results
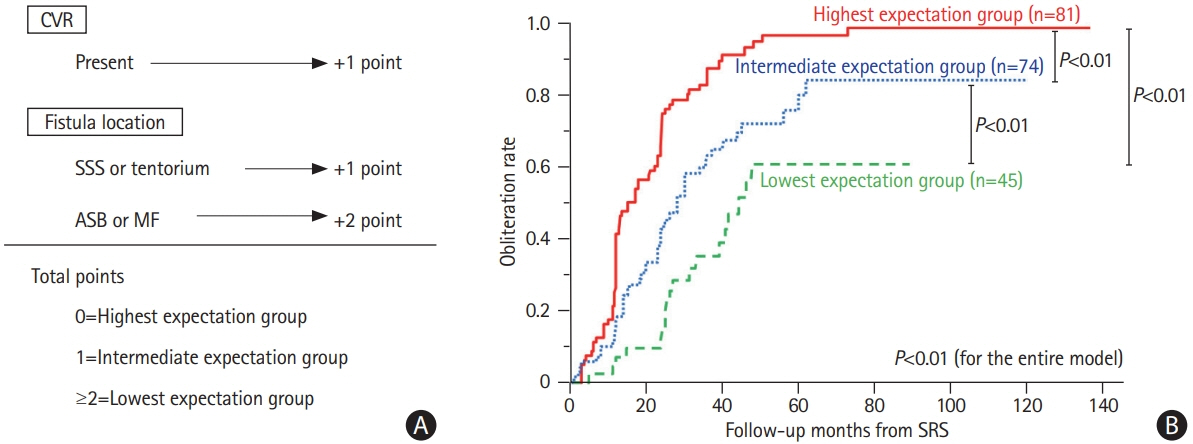
The 3- and 4-year obliteration rates were 66.3% and 78.8%, respectively. The post-SRS hemorrhage rate was 2%. In the matched cohort, the SRS and Emb-SRS groups did not differ in the rates of obliteration (P=0.54) or post-SRS hemorrhage (P=0.50). In multivariable analysis, DAVF location and cortical venous reflux (CVR) were independently associated with obliteration. The new grading system assigned 2, 1, and 0 points to DAVFs in the anterior skull base or middle fossa, DAVFs with CVR or DAVFs in the superior sagittal sinus or tentorium, and DAVFs without these factors, respectively. Using the total points, patients were stratified into the highest (0 points), intermediate (1 point), or lowest (≥2 points) obliteration rate groups that exhibited 4-year obliteration rates of 94.4%, 71.3%, and 60.4%, respectively (P<0.01).
Conclusions
SRS-based therapy achieved DAVF obliteration in more than three-quarters of the patients at 4 years of age. Our grading system can stratify the obliteration rate and may guide physicians in treatment selection.
Keyword
Figure
Reference
-
References
1. Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: classification, imaging findings, and treatment. AJNR Am J Neuroradiol. 2012; 33:1007–1013.
Article2. Söderman M, Pavic L, Edner G, Holmin S, Andersson T. Natural history of dural arteriovenous shunts. Stroke. 2008; 39:1735–1739.
Article3. Fincher EF. Arteriovenous fistula between the middle meningeal artery and the greater petrosal sinus: case report. Ann Surg. 1951; 133:886–888.
Article4. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; 82:166–179.
Article5. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; 194:671–680.
Article6. Reynolds MR, Lanzino G, Zipfel GJ. Intracranial dural arteriovenous fistulae. Stroke. 2017; 48:1424–1431.
Article7. Miller TR, Gandhi D. Intracranial dural arteriovenous fistulae: clinical presentation and management strategies. Stroke. 2015; 46:2017–2025.8. Zipfel GJ, Shah MN, Refai D, Dacey RG Jr, Derdeyn CP. Cranial dural arteriovenous fistulas: modification of angiographic classification scales based on new natural history data. Neurosurg Focus. 2009; 26:E14.
Article9. Satomi J, van Dijk JM, Terbrugge KG, Willinsky RA, Wallace MC. Benign cranial dural arteriovenous fistulas: outcome of conservative management based on the natural history of the lesion. J Neurosurg. 2002; 97:767–770.
Article10. Shah MN, Botros JA, Pilgram TK, Moran CJ, Cross DT 3rd, Chicoine MR, et al. Borden-Shucart type I dural arteriovenous fistulas: clinical course including risk of conversion to higher-grade fistulas. J Neurosurg. 2012; 117:539–545.
Article11. Lunsford LD, Flickinger J, Lindner G, Maitz A. Stereotactic radiosurgery of the brain using the first United States 201 cobalt-60 source gamma knife. Neurosurgery. 1989; 24:151–159.
Article12. Gross BA, Albuquerque FC, McDougall CG, Jankowitz BT, Jadhav AP, Jovin TG, et al. A multi-institutional analysis of the untreated course of cerebral dural arteriovenous fistulas. J Neurosurg. 2018; 129:1114–1119.
Article13. Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg. 1990; 72:839–850.
Article14. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988; 19:604–607.
Article15. Starke RM, Yen CP, Ding D, Sheehan JP. A practical grading scale for predicting outcome after radiosurgery for arteriovenous malformations: analysis of 1012 treated patients. J Neurosurg. 2013; 119:981–987.
Article16. Hung YC, Mohammed N, Kearns KN, Chen CJ, Starke RM, Kano H, et al. Stereotactic radiosurgery for cavernous sinus versus noncavernous sinus dural arteriovenous fistulas: outcomes and outcome predictors. Neurosurgery. 2020; 86:676–684.
Article17. Dmytriw AA, Schwartz ML, Cusimano MD, Mendes Pereira V, Krings T, Tymianski M, et al. Gamma knife radiosurgery for the treatment of intracranial dural arteriovenous fistulas. Interv Neuroradiol. 2017; 23:211–220.
Article18. Park KS, Kang DH, Park SH, Kim YS. The efficacy of gamma knife radiosurgery alone as a primary treatment for intracranial dural arteriovenous fistulas. Acta Neurochir (Wien). 2016; 158:821–828.
Article19. Chen CJ, Lee CC, Ding D, Starke RM, Chivukula S, Yen CP, et al. Stereotactic radiosurgery for intracranial dural arteriovenous fistulas: a systematic review. J Neurosurg. 2015; 122:353–362.
Article20. Serizawa T, Higuchi Y, Nagano O, Kominami S, Hirai T, Ono J, et al. Roles of stereotactic radiosurgery for cerebral arteriovenous malformation and dural intracranial arteriovenous fistula. Jpn J Neurosurg. 2013; 22:917–926.
Article21. Pan DH, Wu HM, Kuo YH, Chung WY, Lee CC, Guo WY. Intracranial dural arteriovenous fistulas: natural history and rationale for treatment with stereotactic radiosurgery. Prog Neurol Surg. 2013; 27:176–194.
Article22. Söderman M, Dodoo E, Karlsson B. Dural arteriovenous fistulas and the role of gamma knife stereotactic radiosurgery: the Stockholm experience. Prog Neurol Surg. 2013; 27:205–217.
Article23. Yen CP, Lanzino G, Sheehan JP. Stereotactic radiosurgery of intracranial dural arteriovenous fistulas. Neurosurg Clin N Am. 2013; 24:591–596.
Article24. Yang H, Kano H, Kondziolka D, Niranjan A, Flickinger JC, Horowitz MB, et al. Stereotactic radiosurgery with or without embolization for intracranial dural arteriovenous fistulas. Prog Neurol Surg. 2013; 27:195–204.
Article25. Friedman JA, Pollock BE, Nichols DA, Gorman DA, Foote RL, Stafford SL. Results of combined stereotactic radiosurgery and transarterial embolization for dural arteriovenous fistulas of the transverse and sigmoid sinuses. J Neurosurg. 2001; 94:886–891.
Article26. Pollock BE, Nichols DA, Garrity JA, Gorman DA, Stafford SL. Stereotactic radiosurgery and particulate embolization for cavernous sinus dural arteriovenous fistulae. Neurosurgery. 1999; 45:459–467.
Article27. Šimundić AM. Measures of diagnostic accuracy: basic definitions. EJIFCC. 2009; 19:203–211.28. Starke RM, McCarthy DJ, Chen CJ, Kano H, McShane B, Lee J, et al. Evaluation of stereotactic radiosurgery for cerebral dural arteriovenous fistulas in a multicenter international consortium. J Neurosurg. 2019; 132:114–121.
Article29. Suh DC, Lee JH, Kim SJ, Chung SJ, Choi CG, Kim HJ, et al. New concept in cavernous sinus dural arteriovenous fistula: correlation with presenting symptom and venous drainage patterns. Stroke. 2005; 36:1134–1139.
Article30. Wu HM, Pan DH, Chung WY, Guo WY, Liu KD, Shiau CY, et al. Gamma Knife surgery for the management of intracranial dural arteriovenous fistulas. J Neurosurg. 2006; 105 Suppl:43–51.
Article31. Cifarelli CP, Kaptain G, Yen CP, Schlesinger D, Sheehan JP. Gamma knife radiosurgery for dural arteriovenous fistulas. Neurosurgery. 2010; 67:1230–1235.
Article32. Hanakita S, Koga T, Shin M, Shojima M, Igaki H, Saito N. Role of gamma knife surgery in the treatment of intracranial dural arteriovenous fistulas. J Neurosurg. 2012; 117 Suppl:158–163.
Article33. Chen CJ, Buell TJ, Diamond J, Ding D, Kumar JS, Taylor DG, et al. Stereotactic radiosurgery for high-grade intracranial dural arteriovenous fistulas. World Neurosurg. 2018; 116:e640–e648.
Article34. Tonetti DA, Gross BA, Jankowitz BT, Kano H, Monaco EA, Niranjan A, et al. Reconsidering an important subclass of high-risk dural arteriovenous fistulas for stereotactic radiosurgery. J Neurosurg. 2018; 130:972–976.
Article35. Tonetti DA, Gross BA, Jankowitz BT, Atcheson KM, Kano H, Monaco EA, et al. Stereotactic radiosurgery for dural arteriovenous fistulas without cortical venous reflux. World Neurosurg. 2017; 107:371–375.
Article36. Yang HC, Kano H, Kondziolka D, Niranjan A, Flickinger JC, Horowitz MB, et al. Stereotactic radiosurgery with or without embolization for intracranial dural arteriovenous fistulas. Neurosurgery. 2010; 67:1276–1285.
Article37. Oermann EK, Ding D, Yen CP, Starke RM, Bederson JB, Kondziolka D, et al. Effect of prior embolization on cerebral arteriovenous malformation radiosurgery outcomes: a case-control study. Neurosurgery. 2015; 77:406–417.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stereotactic radiosurgery for dural arteriovenous fistula
- Role of surgery in management of intracranial dural arteriovenous fistulas
- Multiple Dural Arteriovenous Fistulas Presenting as Pulsatile Tinnitus Treated with External Manual Compression
- Endovascular management of cavernous sinus dural arteriovenous fistulas: Overall review and considerations
- Novalis Stereotactic Radiosurgery for Spinal Dural Arteriovenous Fistula