J Korean Med Sci.
2022 May;37(21):e172. 10.3346/jkms.2022.37.e172.
Effects of Non-Pharmacological Interventions on Respiratory Viruses Other Than SARS-CoV-2: Analysis of Laboratory Surveillance and Literature Review From 2018 to 2021
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 2Department of Diseases Research, Incheon Metropolitan City Institute of Public Health and Environment, Incheon, Korea
- KMID: 2530116
- DOI: http://doi.org/10.3346/jkms.2022.37.e172
Abstract
- Background
Since the global coronavirus disease 2019 (COVID-19) pandemic, nonpharmacological interventions (NPIs) such as extensive and comprehensive hand hygiene, mask-wearing, and social distancing have been implemented globally. This study aimed to investigate changes in respiratory viruses other than severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) that occurred following the implementation of these NPIs.
Methods
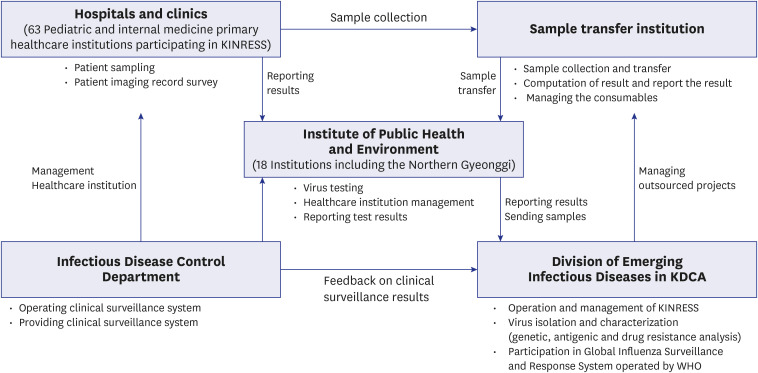
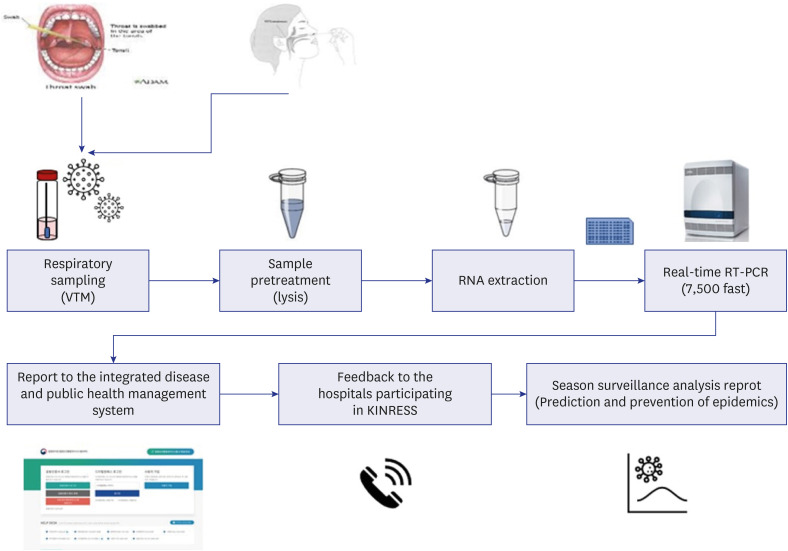
From January 2018 to December 2021, influenza-like illness patient specimens and specimens from the Korea Influenza and Respiratory Viruses Surveillance System were analyzed at the Incheon Metropolitan City Institute of Public Health and Environment. Oropharyngeal or nasopharyngeal swab samples from respiratory infection patients were transferred in a virus transport medium at 4°C. After RNA or DNA extraction, respiratory virus-specific genes for human influenza virus (IFV), adenovirus (ADV), parainfluenza virus (PIV), respiratory syncytial virus (RSV), human rhinovirus (hRV), human coronavirus, human bocavirus, and human metapneumovirus were detected by individual real-time reverse transcription polymerase chain reaction.
Results
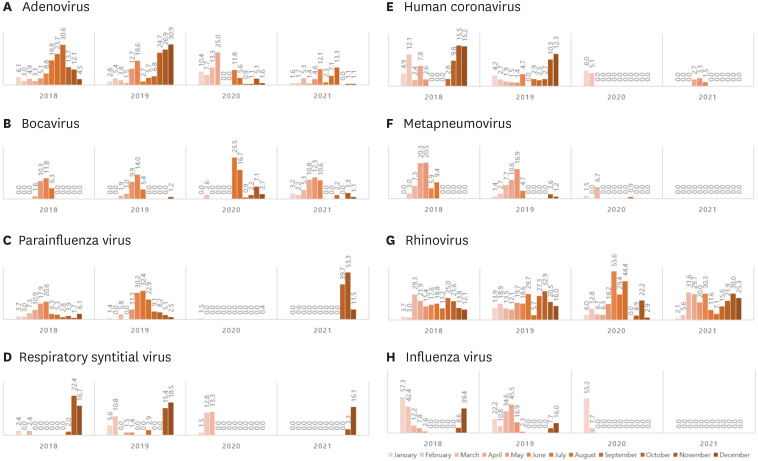
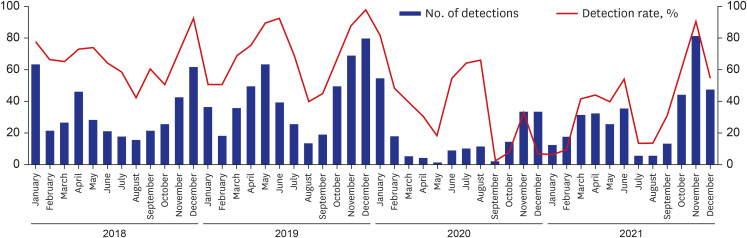
A total 3,334 samples were collected. After NPI was implemented, the detection of respiratory viruses other than SARS-CoV-2 decreased overall. The yearly detection rate of respiratory viruses was decreased from 69.5% (399/574) in 2018 and 73.3% (505/689) in 2019 to 19.8% (206/1,043) in 2020 and 34.9% (365/1,028) in 2021. The epidemic was more prominent in respiratory viruses such as IFV and RSV, which were considered dominant viruses, especially those with viral envelopes. Among viruses that were not considered dominant, hRV showed no clear change before and after NPI, while PIV showed a rapid increase compared to the existing dominant viruses between October–December 2021, after the increase in the number of gatherings started at the end of September and the “Relaxing COVID19 and mitigation policy,” which was implemented on November 1.
Conclusion
NPI seems to have influenced the isolation and transmission of respiratory viruses in South Korea. In the future, additional studies focusing on the isolation and transmission patterns of respiratory viruses following NPI are needed.
Keyword
Figure
Cited by 1 articles
-
Nationwide Trends in Non-COVID-19 Infectious Disease Laboratory Tests in the Era of the COVID-19 Pandemic in Korea
Sun Bean Kim, Young-Eun Kim, Taemo Bang, Minwoo Hong, Munkhzul Radnaabaatar, Kyungmin Huh, Ki Ho Hong, Jaehun Jung
J Korean Med Sci. 2023;38(47):e408. doi: 10.3346/jkms.2023.38.e408.
Reference
-
1. World Health Organization. WHO announces COVID-19 outbreak a pandemic. Updated 2020. Accessed March 12, 2022. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200509covid-19-sitrep-110.pdf?sfvrsn=3b92992c_6 .2. Korean Society of Infectious Diseases. Korean Society of Pediatric Infectious Diseases. Korean Society of Epidemiology. Korean Society for Antimicrobial Therapy. Korean Society for Healthcare-associated Infection Control and Prevention. Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020; 35(10):e112. PMID: 32174069.3. Oh J, Lee JK, Schwarz D, Ratcliffe HL, Markuns JF, Hirschhorn LR. National response to COVID-19 in the Republic of Korea and lessons learned for other countries. Health Syst Reform. 2020; 6(1):e1753464. PMID: 32347772.4. Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Curr Opin Virol. 2018; 28:142–151. PMID: 29452994.5. Korea Disease Control and Prevention Agency. Respiratory Infectious Disease Control Guidelines. Cheongju, Korea: Korea Disease Control and Prevention Agency;2021.6. Kim IH, Kang BH, Seo SH, Park YE, Kim GJ, Lee SW, et al. Early laboratory preparedness of the Korea Disease Control and Prevention Agency and response to unknown pneumonia outbreak from Wuhan, China, in January 2020. Ann Lab Med. 2021; 41(6):532–539. PMID: 34108280.7. Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020; 25(47):2001847.8. Yum S, Hong K, Sohn S, Kim J, Chun BC. Trends in viral respiratory infections during COVID-19 pandemic, South Korea. Emerg Infect Dis. 2021; 27(6):1685–1688. PMID: 34013875.9. Huang QS, Wood T, Jelley L, Jennings T, Jefferies S, Daniells K, et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat Commun. 2021; 12(1):1001. PMID: 33579926.10. Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020; 81(2):266–275. PMID: 32473235.11. Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020; 39(12):e423–e427. PMID: 32773660.12. Kim YG, Park H, Kim SY, Hong KH, Kim MJ, Lee JS, et al. Rates of coinfection between SARS-CoV-2 and other respiratory viruses in Korea. Ann Lab Med. 2022; 42(1):110–112. PMID: 34374357.13. Kim Z, Lee JH. Coinfection with severe acute respiratory syndrome coronavirus-2 and other respiratory viruses at a tertiary hospital in Korea. J Clin Lab Anal. 2021; 35(8):e23868. PMID: 34273182.14. Lee H, Lee H, Song KH, Kim ES, Park JS, Jung J, et al. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin Infect Dis. 2021; 73(1):e132–e140. PMID: 32472687.15. Alvi MM, Sivasankaran S, Singh M. Pharmacological and non-pharmacological efforts at prevention, mitigation, and treatment for COVID-19. J Drug Target. 2020; 28(7-8):742–754. PMID: 32643436.16. Odusanya OO, Odugbemi BA, Odugbemi TO, Ajisegiri WS. COVID-19: a review of the effectiveness of non-pharmacological interventions. Niger Postgrad Med J. 2020; 27(4):261–267. PMID: 33154276.17. Zildzic M, Salihefendic D, Masic I. Non-pharmacological measures in the prevention and treatment of COVID-19 infection. Med Arh. 2021; 75(4):307–312.18. Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev. 2020; 11(11):CD006207. PMID: 33215698.19. Varela FH, Scotta MC, Polese-Bonatto M, Sartor IT, Ferreira CF, Fernandes IR, et al. Absence of detection of RSV and influenza during the COVID-19 pandemic in a Brazilian cohort: likely role of lower transmission in the community. J Glob Health. 2021; 11:05007. PMID: 33791096.20. Agca H, Akalin H, Saglik I, Hacimustafaoglu M, Celebi S, Ener B. Changing epidemiology of influenza and other respiratory viruses in the first year of COVID-19 pandemic. J Infect Public Health. 2021; 14(9):1186–1190. PMID: 34399190.21. Kim JH, Roh YH, Ahn JG, Kim MY, Huh K, Jung J, et al. Respiratory syncytial virus and influenza epidemics disappearance in Korea during the 2020-2021 season of COVID-19. Int J Infect Dis. 2021; 110:29–35. PMID: 34245886.22. Noh JY, Seong H, Yoon JG, Song JY, Cheong HJ, Kim WJ. Social distancing against COVID-19: implication for the control of influenza. J Korean Med Sci. 2020; 35(19):e182. PMID: 32419400.23. Ippolito G, La Vecchia A, Umbrello G, Di Pietro G, Bono P, Scalia S, et al. Disappearance of seasonal respiratory viruses in children under two years old during COVID-19 pandemic: a monocentric retrospective study in Milan, Italy. Front Pediatr. 2021; 9:721005. PMID: 34422733.24. Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, et al. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa, 2020. Am J Transplant. 2020; 20(12):3681–3685. PMID: 33264506.25. Liu P, Xu M, Cao L, Su L, Lu L, Dong N, et al. Impact of COVID-19 pandemic on the prevalence of respiratory viruses in children with lower respiratory tract infections in China. Virol J. 2021; 18(1):159. PMID: 34344406.26. Partridge E, McCleery E, Cheema R, Nakra N, Lakshminrusimha S, Tancredi DJ, et al. Evaluation of seasonal respiratory virus activity before and after the statewide COVID-19 shelter-in-place order in Northern California. JAMA Netw Open. 2021; 4(1):e2035281. PMID: 33492377.27. Redlberger-Fritz M, Kundi M, Aberle SW, Puchhammer-Stöckl E. Significant impact of nationwide SARS-CoV-2 lockdown measures on the circulation of other respiratory virus infections in Austria. J Clin Virol. 2021; 137:104795. PMID: 33761423.28. Poole S, Brendish NJ, Clark TW. SARS-CoV-2 has displaced other seasonal respiratory viruses: results from a prospective cohort study. J Infect. 2020; 81(6):966–972. PMID: 33207254.29. Soo RJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis. 2020; 26(8):1933–1935. PMID: 32339092.30. Ye Q, Liu H. Impact of non-pharmaceutical interventions during the COVID-19 pandemic on common childhood respiratory viruses – An epidemiological study based on hospital data. Microbes Infect. 2022; 24(1):104911. PMID: 34871774.31. Jongbloed M, Leijte WT, Linssen CF, van den Hoogen BG, van Gorp EC, de Kruif MD. Clinical impact of human metapneumovirus infections before and during the COVID-19 pandemic. Infect Dis (Lond). 2021; 53(7):488–497. PMID: 33612055.32. Kim HM, Lee EJ, Lee NJ, Woo SH, Kim JM, Rhee JE, et al. Impact of coronavirus disease 2019 on respiratory surveillance and explanation of high detection rate of human rhinovirus during the pandemic in the Republic of Korea. Influenza Other Respi Viruses. 2021; 15(6):721–731.33. Seo YB, Song JY, Choi MJ, Kim IS, Yang TU, Hong KW, et al. Etiology and clinical outcomes of acute respiratory virus infection in hospitalized adults. Infect Chemother. 2014; 46(2):67–76. PMID: 25024868.34. Korea Disease Control and Prevention Agency. Public Health Weekly Report. Updated 2022. Accessed March 22, 2022. https://www.kdca.go.kr/board/board.es?mid=a30501000000&bid=0031&cg_code=C06 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lessons Learned from SARS-CoV and MERS-CoV: Preparation for SARS-CoV-2 induced COVID-19
- Severe Acute Respiratory Syndrome, SARS
- Understandings and Prospects of Laboratory Diagnosis of SARS-CoV-2
- Evaluation of Three Multiplex Realtime Reverse Transcription PCR Assays for Simultaneous Detection of SARS-CoV-2, Influenza A/B, and Respiratory Syncytial Virus in Nasopharyngeal Swabs
- Challenges of Scaling Up SARS-CoV-2 Rapid Antigen Tests